Supplementary Material 1 Patients and Methods Patients The cohort
advertisement

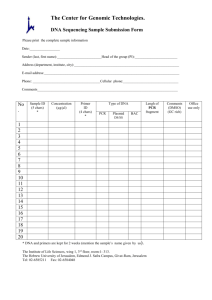
Supplementary Material 1 Patients and Methods Patients The cohort comprised 68 probands from unrelated families selected for matching either “classic” Li–Fraumeni Syndrome (LFS) [1], or one of the Li-Fraumeni Like (LFL) criteria [15] and negative for mutations on the TP53 gene [6]. All subjects were seen at the AC Camargo Hospital, São Paulo, Brazil. As control, a Brazilian group of 404 unrelated individuals from families investigated for reasons other than cancer was used. DNA samples obtained from peripheral blood after informed consents were provided by the Genetic Center of the Institute of Biosciences, University of São Paulo, São Paulo, Brazil. Array-CGH DNA from patients and controls was obtained from peripheral blood. Investigation of copy number changes was performed by array-CGH using the whole genome Agilent SurePrint G3 Human CGH Microarray (Agilent Technologies, Santa Clara, USA) containing ~180.000 oligonucleotides. Briefly, samples were labeled with Cy3- and Cy5-dCTPs by random priming; purification, hybridization, and washing were carried out as recommended by the manufacturer. Scanned images of the arrays were processed and analyzed using Feature Extraction and Genomic Workbench software (both from Agilent Technologies), together with the statistical algorithm ADM-2, and using a sensitivity threshold of 6.7. We used two reversed labeled hybridizations for each sample. Gains or losses in copy number were accepted when the log2 ratio of the Cy3/Cy5 intensities of a given genomic segment encompassing at least three consecutive probes was > 0.3 or < -0.3, respectively; any alterations not detected in both dye-swap experiments were disregarded. All detected imbalances were compared to CNVs reported in the Database of Genomic Variants (DGV; http://projects.tcag.ca/variation/ - freeze of March, 2011) and to data from our own group. Gene annotation was performed using University of California Santa Cruz Genome Browser (UCSC). Copy number variation by Real time PCR Gene dosage ratios were calculated for BAX and FTL genes using the methods of 2-∆∆Ct [7]. Primers for GAPDH intron 7 (12p13) and HPRT1 exon 3 (Xq26.1) were used as normalizer (norm) genes. All assays were conducted in 96-well plates (MicroAmpOptical 96-Well Reaction Plate, Applied Biosystems, Foster City, CA). As the reference sample or calibrator, we used commercial human genomic DNA (Promega, Madison, USA). 20 ng of each DNA sample were amplified in a 20 uL reaction, containing 0.3 µmol of each primer and 1X SYBR® Green PCR MasterMix (Applied Biosystems). qPCR was performed on an ABI Prism 7500 detection system (Applied Biosystems) and entailed a preincubation of 95°C for 10 minutes followed by 40 cycles of denaturation at 95°C for 15 seconds, annealing and extension at 60°C for 1 minute. Samples were amplified in triplicate for both target and normalizer genes. The average Ct of the duplicate was used in the gene dosage ratio calculations. For each gene, two control individuals were used to calculate the average control Ct. Gene dosage ratios were calculated using the following equation: 2-[∆Ct (target) - ∆Ct (norm)] where ∆Ct (target) equals the difference between the Ct values for the patient and the control average for the target exon, and the ∆Ct (norm) equals the difference between CT values for the patient and the control average for the normalizer gene. Ratios between 0.82 and 1.22 were considered normal, between 0.41 and 0.61 indicated deletions in one allele and above 1.4 indicated amplifications. DNA sequencing Genomic DNA was prepared following standard DNA extraction procedures. Direct sequencing for P16INK4, P14ARF, CDK4, KIT, PDGFRA and BAX genes were performed on the peripheral blood DNA. Each exon was amplified individually using 50 ng of genomic DNA. The PCR reactions contained 0.25 uM of each primer, 0.2 mM of each dNTPs, 2.0 mM of MgCl2 and 0.5 U Platinum Taq DNA Polymerase (Invitrogen) in a final reaction volume of 20 ul. PCR products were purified with ExoSAP-IT (USB) and sequenced in both directions. Sequencing reactions were performed with Big Dye v.3.1 (Applied Biosystems) and separated on ABI Prism 3500 (Applied Biosystems) and analyzed using CLC Bio software. Primers sequences are available upon request. References 1. 2. 3. 4. 5. 6. Li FP, Fraumeni JF, Mulvihill JJ, Blattner WA, Dreyfus MG, Tucker MA, Miller RW. A cancer family syndrome in twenty-four kindreds. Cancer Res 1988; 48(18):5358-5362. Eeles RA. Germline mutations in the TP53 gene. Cancer Surv 1995; 25:101-124. Birch JM, Heighway J, Teare MD, Kelsey AM, Hartley AL, Tricker KJ, Crowther D, Lane DP, Santibáñez-Koref MF. Linkage studies in a Li-Fraumeni family with increased expression of p53 protein but no germline mutation in p53. Br J Cancer 1994; 70(6):1176-1181. Birch JM, Hartley AL, Tricker KJ, Prosser J, Condie A, Kelsey AM, Harris M, Jones PH, Binchy A, Crowther D. Prevalence and diversity of constitutional mutations in the p53 gene among 21 Li-Fraumeni families. Cancer Res 1994; 54(5):1298-1304. Tinat J, Bougeard G, Baert-Desurmont S, Vasseur S, Martin C, Bouvignies E, Caron O, Bressac-de Paillerets B, Berthet P, Dugast C et al. 2009 version of the Chompret criteria for Li Fraumeni syndrome. J Clin Oncol 2009; 27(26):e108-109; author reply e110. Achatz MI, Olivier M, Le Calvez F, Martel-Planche G, Lopes A, Rossi BM, AshtonProlla P, Giugliani R, Palmero EI, Vargas FR et al. The TP53 mutation, R337H, is associated with Li-Fraumeni and Li-Fraumeni-like syndromes in Brazilian families. Cancer Lett 2007;245(1-2):96-102. 7. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001; 25(4):402408.