Administrative Office St. Joseph`s Hospital Site, L301
advertisement

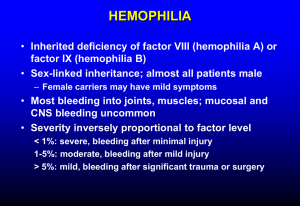
Administrative Office St. Joseph's Hospital Site, L301-10 50 Charlton Avenue East HAMILTON, Ontario, CANADA L8N 4A6 PHONE: (905) 521-6141 FAX: (905) 521-6142 http://www.fhs.mcmaster.ca/hrlmp/ Issue No. 64 QUARTERLY NEWSLETTER August 2002 Laboratory Diagnosis of von Willebrand Disease von Willebrand disease (vWD) is one of the most common inherited bleeding disorders. In recent years, there have been major advances in our understanding of vWD, which is caused by quantitative and/or qualitative problems with von Willebrand factor (vWF). Normally, vWF has two important roles in controlling bleeding: it promotes platelet adhesion in the initial steps of hemostasis, and it functions as the carrier protein for factor VIII (the protein needed for fibrin clot formation that is missing in patients with severe hemophilia A). Patients who completely lack vWF have combined problems with platelet adhesion and fibrin clot formation. vWF is one of the largest known proteins in the body, and is made in both endothelial cells and in megakaryocytes. vWF circulates in plasma and is also retained within platelets and endothelial cells for release at sites of blood vessel injury. During hemostasis, vWF supports platelet adhesion by interacting with two platelet receptors, glycoprotein (GP) IbIX and the integrin aIIbb3. Conformational changes in vWF (induced by shear forces or binding to blood vessels) are thought to initiate the binding of vWF to platelet GP IbIX. This event triggers further activation of platelets, which allows plasma vWF, and other adhesive ligands, to bridge platelet aIIbb3 receptors to create a stable platelet plug. The levels of vWF vary considerably in healthy individuals and are often increased with strenuous exercise, stress, pregnancy, hemorrhage, and surgery. Low levels are seen in inherited or acquired vWD and in hypothyroidism. vWF levels are influenced by ABO blood groups. Levels are lowest in blood group O and are highest in blood group AB. Therefore, ABO blood groups must be considered before making the diagnosis of mild vWD. Because vWF levels can fluctuate, abnormalities should be confirmed, and several determinations are often needed for suspected mild vWF deficiencies. The common types of bleeding problems experienced by individuals with vWD are mucocutaneous bleeding symptoms (nose bleeds, bruising, heavy menstrual periods, postpartum bleeding, bleeding gums, GI bleeding) and immediate excessive bleeding with trauma, surgery and dental extractions. Severe vWD is associated with platelet-like and hemophilia-like bleeding symptoms, because of low factor VIII levels. The rare type 2N form of vWD mimics mild-moderate hemophilia because of an impaired factor VIII binding function of vWF. The new revised classification scheme divides vWD into three major categories (see chart, Page 2). Types 1 and 3 vWD are associated with quantitative vWF deficiencies, whereas type 2 vWD is associated with qualitative vWF abnormalities, subdivided according to the type of changes found. Genetic abnormalities in the vWF gene have been demonstrated in many forms of type 2 vWD, but are largely unknown in type 1 vWD. Laboratory Tests Available for the Diagnosis of vWD The special coagulation laboratory of the HRLMP offers the following tests for the diagnosis of vWD: vWD screen: Includes tests for factor VIII:C, vWF antigen and vWF ristocetin cofactor activity. If these tests show an abnormality, multimer testing is performed. ABO blood group should be determined, if unknown, to facilitate interpretation of the test results. (see Gill et al). Factor VIII:C level: quantitative assay of the function of coagulation factor VIII in plasma vWF-antigen assay (vWF:ag): quantitation of the vWF-antigen in the plasma by an enzyme linked immunoassay. Ristocetin Cofactor Activity assay (RCoF): measures the ability of the patient’s plasma vWF to support aggregation of standardized test platelets with ristocetin. Normally, the ratio of vWF RCoF to vWF:ag are close to 1 whereas low ratios (<0.7) are typical of type 2A, 2B and 2M vWD. vWF multimer analysis: Western blot assay that evaluates the sizes of vWF multimers in the patient’s plasma. Should be done when vWD screens indicate abnormalities and/or the ratio of vWF RCoF:vWF:ag is <0.7. Multimer patterns are helpful in distinguishing quantitative and qualitative forms of vWD. Patients with abnormal multimers should have RIPA testing done. Ristocetin Induced Platelet Aggregation (RIPA) studies: The RIPA assay evaluates the ability of the patient’s plasma and platelets to aggregate in response to low and high concentrations of ristocetin. RIPA tests are recommended when vWD screening tests show an abnormality and/or type 2B vWD is suspected based on initial investigations and/or family history. Reduced RIPA with high dose ristocetin can be seen in types 1, 2, and 3 vWD, and in patients with platelet disorders. Abnormally increased RIPA with low dose ristocetin is seen in type 2B vWD, and much less commonly, in "platelet type vWD" where the platelet GPIbIX has increased vWF binding. Bleeding time: a standardized cut is made on the forearm and the time to stop bleeding is determined. Test is not sufficiently sensitive to screen patients for vWD, and is of limited value in investigating vWD. Classifications of vWD Classification Inheritance Type 1 vWD autosomal dominant Description / variants quantitative deficiency, below the level expected for the individual’s ABO blood group accounts for approximately 70% of vWD Type 2 vWD Typ e 2A most forms autosomal dominant qualitative abnormalities in vWF platelet-dependent adhesive function and an absence of the most potent, high and intermediate molecular weight vWF multimers autosomal dominant the most common type 2 variant Typ e 2B abnormally affinity of vWF for the platelet receptor GP IbIX. Unlike type 2A, there is abnormally platelet aggregation with low dose (0.5 mg/ml) ristocetin. Often associated with a lack of the largest vWF multimers. autosomal dominant second most common type 2 variant Typ e 2M autosomal dominant platelet-dependent adhesive function with normal vWF multimers Typ e 2N typically autosomal recessive markedly affinity of vWF for factor VIII, resulting in low factor VIII levels Type 3 vWD autosomal recessive rare virtually complete deficiency of vWF Summary table of typical laboratory findings in the different forms of vWD vWD Factor VIII vWF:ag RCoF Type 1 proportionally with vWF:ag RIPA can be at high conc., normal normal at low dose at high conc. relative to Type 2A or normal or normal relative to vWF:ag VWF Multimers vWF:ag, large and intermediate multimers absent normal at low dose or normal; Type 2B or normal or normal Type 2M or normal or normal Type 2N moderately normal typically relative to the level of vWF:ag relative to the level of vWF:ag normal with low dose; mixing studies indicate the defect is in the patient’s plasma large multimers usually absent usually normal normal normal Type 3 ( 5% of normal) absent or trace absent absent none or only traces detected For further information please contact the Special Coagulation laboratory at 905-521-2100 ext. 76277. REFERENCES 1. 2. Colman RW, Hirsh J et al. "Hemostasis and Thrombosis, Basic Principles and Clinical Practice, 4th edition"; Lippincott Williams and Wilkins; pp 825-837: 2001. Gill JC, Endres-Brooks J, Bauer PJ, Marks WJ, Montgomery RR. The effect of ABO blood groups on the diagnosis of von Willebranddisease. Blood 69: 1691-1695, 1987. Karen A. Moffat, ART, Technical Specialist, Specialized Regional Coagulation Laboratory Catherine P.M. Hayward, MD, PhD, FRCP(C), Head, Specialized Regional Coagulation Laboratory HRLMP, Hamilton Health Sciences, McMaster University Medical Centre Site