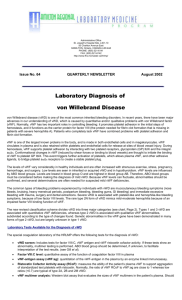
Von Willebrand Disease
advertisement

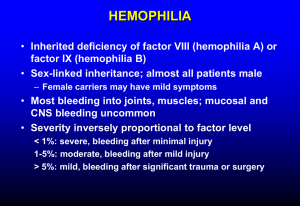
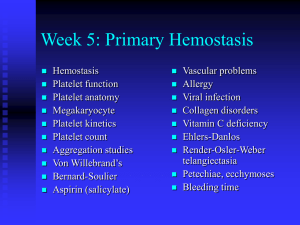
Von Willebrand Disease Uptodate - Classification and pathophysiology of von Willebrand disease Von Willebrand disease (VWD) is characterized by mutations that lead to an impairment in the synthesis or function of von Willebrand factor (VWF) It is the most common inherited bleeding disorder affecting 1% of the population Only 5% of those patients are symptomatic Clinical Presentation o Bleeding symptoms in VWD occur when von Willebrand Factor (VWF) is sufficiently decreased in the plasma or platelets, or when a qualitative defect in VWF impairs one of its functions o Abnormalities mostly affect platelet plug formation during the primary hemostatic response. As a result, many of the usual clinical manifestations of VWD are similar to those seen in platelet disorders. These include: o Easy bruising o Skin bleeding o Prolonged bleeding from mucosal surfaces (eg, oropharyngeal, gastrointestinal, uterine). o Patients can become symptomatic at any age o Women usually report menorrhagia or post partum hemorrhage o GI Bleeding – can be serious but is less common o If patient has mild disease then ingestion of aspirin or other antiplatelet agent mat exacerbate bleeding Laboratory Testing o 3 tests are recommended o Plasma VWF antigen (VWF:Ag) o Plasma VWF activity (ristocetin cofactor activity, VWF:RCo and VWF collagen binding; VWF:CB) VWF activity is commonly assayed as ristocetin cofactor activity (VWF:RCo), which tests the ability of VWF to agglutinate platelets by binding to its primary receptor, platelet glycoprotein Ib (GP Ib) in the presence of ristocetin The standard plasma used for the initial curve should be related to the WHO standard, and the results reported in IU/dL or IU/mL, where 100 percent activity equals 100 IU/dL or 1 IU/mL. o Factor VIII activity (FVIII) Since normal VWF protects factor VIII from proteolysis, decreased plasma VWF or a mutation in the VWF binding site for factor VIII (eg, type 2N VWD) can lead to decreased plasma factor VIII concentrations o Platelet function analyzer assay Bleeding time o BT does not correlate well with any specific plasma VWF assay, it is helpful diagnostically if it is abnormal o If there is still a high index of suspicion in the face of normal results then the tests should be repeated. If one of the tests is abnormal then specialized assays can be performed o VWF multimer distribution using gel electrophoresis o This test is used to identify variants of type 2 VWD that lack the largest multimers (types 2A and 2B), or have unusually large multimers, or other qualitatively abnormal "bands" that indicate an abnormal VWF structure Ristocetin-induced platelet aggregation (RIPA) Measures the affinity with which VWF binds to the platelet receptor GP Ib by limiting the concentration of ristocetin in the assay. It is used primarily to look for the type 2B variant of VWF which has mutations in the binding site for GP Ib such that the type 2B VWF binds to GP Ib more readily than normal Physiology of von Willebrand Factor o Plays an important role in primary hemostatis by binding platelets and endothelium o It also contributes to fibrin clot formation by acting as a carrier protein for factor VIII, which has a greatly shortened half-life and abnormally low concentration unless it is bound to VWF. o Plasma VWF is synthesized by megakaryocytes and endothelial cells and undergoes extensive post-synthetic processing. When released acutely from these cells, VWF contains even larger multimers than are normally observed in the circulation. Because these “unusually large” forms are prothrombotic they are rapidly proteolyzed to the “normal” multimer size distribution as defined by a normal plasma pool. Mutations of Von Willebrand Factor o Type 1 – AD inheritance – most common 75% of patients o Partial quantitative deficiency of VWF o Type 2 – usually AD inheritance – several qualitative abnormalities of VWF o 4 subtypes – 2A, 2B, 2M, and 2N o 2A Approximately 10 to 20 percent of cases of VWD, and is usually transmitted as an autosomal dominant trait. Affected patients usually present with moderate to moderately severe bleeding o 2B Type 2B VWD accounts for approximately 5 percent of cases of VWD, and is transmitted as an autosomal dominant trait. These mutations appear to disrupt the structure within the A1 domain that contains the binding site for platelet GP Ib, and result in a VWF that binds more readily to GP Ib; thus it represents a “gain-of-function” mutation The increase in binding of larger VWF multimers to platelet GP Ib results in their sequestration or loss from the circulation and, in some patients thrombocytopenia Thrombocytopenia is an independent risk factor for bleeding in these patients o 2M Uncommon, autosomal dominant disorder characterized by reduced binding of VWF to GP Ib, resulting in decreased platelet adhesion Affected patients typically have significant bleeding symptoms o 2N Type 2N VWD (N is for Normandy where one of the first patients was described) is an uncommon disorder that is inherited as an autosomal recessive trait o Type 3 Affected patients present with low levels of factor VIII (usually 5 to 15 percent of normal) due to proteolytic cleavage of factor VIII that is normally impeded by the binding of factor VIII to VWF and as a result some patients are misdiagnosed as having hemophilia A n order to be symptomatic, type 2N mutations must be inherited in a recessive manner, or must occur in patients with a second VWF defect causing decreased synthesis of the second allele ar inheritance – severe disease with undetectable levels of VWF Present with severe bleeding involving both the skin and mucous membrane surfaces (due to decreased VWF-related platelet function) as well as in soft tissues and joints (due to the low concentration of factor VIII) Treatment o There are 5 classes of medications for the treatment of VWD o Desmopressin Desmopressin (dDAVP) is a synthetic analog of antidiuretic hormone which retains antidiuretic activity but lacks vasopressor activity Promotes the release of VWF from endothelial cell storage sites; this response is indirect, since it cannot be reproduced by direct exposure of endothelial cells to dDAVP dose of 0.3 micrograms/kg (maximum 20 micrograms) is diluted in 50 mL of normal saline and infused over 20 to 30 minutes Type 1 - Desmopressin is effective in almost all patients with mild or moderate type 1 disease Type 2A – Desmopressin has a variable effect on the VWF level, the reduced hemostatically active high and intermediate molecular weight multimers, and the prolonged bleeding time Type 2B – desmopressin can increase the already abnormal binding of VWF and GP1b increasing thrombocytopenia – do not use unless a previously documented trial has been performed and shown to be beneficial Type 2M - Although data are limited, desmopressin may produce a good response in some patients with type 2M VWD Type 2N - have normal VWF platelet function but impaired binding to factor VIII, leading to low factor VIII levels. These patients may benefit from desmopressin, despite the shorter than normal half-life of the released factor VIII Type 3 - Desmopressin does not increase VWF levels in patients with type 3 VWD, probably due to a lack of VWF in the storage sites o Replacement therapy with VWF-containing concentrates Patients with type 3 VWD and severe type 2A, 2B and 2M o Antifibrinolytic drugs o Topical therapy with thrombin or fibrin sealant o Estrogen therapy in some settings in women