Scenario 2 session 1 Case 1 Miss X presented to her GP with a 24
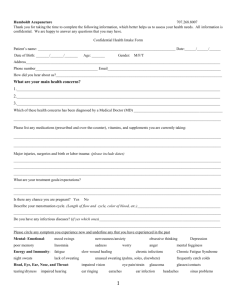
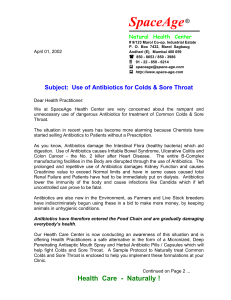
advertisement

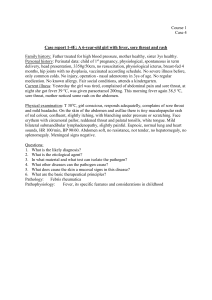
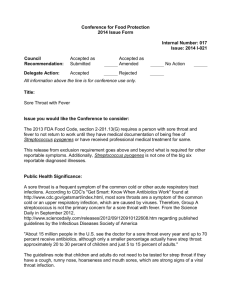
Scenario 2 session 1 Case 1 Miss X presented to her GP with a 24 hour history of sore throat not associated with a cough nor any other respiratory symptoms. On examination she had a temperature of 38⁰ C with exudates on her tonsils and tender cervical lymph nodes. The GP knew that this presentation is suggestive of group A β haemolytic streptococcus infection. The GP prescribed a seven day course of penicillin and took a throat swab. The swab result confirmed group A β haemolytic streptococcus and sensitivity to penicillin. Nine days later, the patient returned to the GP with continuing symptoms of sore throat. On examination, the patient still had an inflamed throat but there was no exudates and lymph nodes were still tender. The GP prescribed a further course of penicillin. A later consultation identified that the sore throat had settled two days later. Case 2 Miss Y presented to her GP with a history of sore throat for two days and a blocked nose. On examination, the pharynx was inflamed with some exudates on tonsils but otherwise the patient was well. She has described a similar episode a few years back that had been successfully treated with antibiotics and she was requesting antibiotics for this episode. After negotiation, antibiotics were not given and a throat swab taken. A week later a throat swab confirmed group A (non β) haemolytic streptococcus and the patient was given a prescription for penicillin. Following this, the patient wrote a letter of complaint stating that she still had a sore throat and that her sister had presented on the same day and been seen by a different doctor who had given her antibiotics. An appointment was given to discuss with the patient but he patient did not attuned. These cases presented the practice with two clinical questions: 1. Does the use of throat swab improve diagnostic accuracy? 2. Do antibiotics improve symptoms and reduce complications? The following information was found following a search of the Cochrane library and a review form the Drugs and Therapeutics Bulletin. Throat swab is currently recommended as a diagnostic aid for patients presenting with sore throat The sensitivity (26-30%) and specificity (73-80%) reported is low compared ot the gold standard of antistreptolysin O titre. The low predictive rate of throat swab is likely due to the high symptomless carriage of group A β haemolytic streptococcus. Antistreptolysin O titre is not convenient to use in routine clinical practice due to cost, delay and inconvenience. Cochrane report that 90% of all patients, whether treated or not are relieved of their symptoms within one week. Of those treated with antibiotics, symptoms settle at day three. Maximum benefit of antibiotics is at three and a half days, when the symptoms of half of the treated patients have already subsided. There are many risks associated with prescribing antibiotics such as diarrhoea, rashes and rarely anaphylaxis. Treating with antibiotics ‘medicalises’ sore throat and the patient subsequently expects antibiotics to be prescribed. Answer he following questions: 1. Given the facts presented, what would your recommendation be to the practice about taking throat swabs? 2. About the use of antibiotics for sore throat? 3. Would other things need to be considered before developing a protocol for routine use? 4. Do you think the right questions were asked? 5. What types of studies would have answered the questions? 6. Do you think either doctor was guided by clinical expertise? 7. What might have been some of the advantages of undertaking a literature search? Taken from Graham, A and Fahey, T. (2008). Evidence based case report: sore throat: diagnostic and therapeutic dilemmas. BMJ. 319: 173-174.