Treatment_in_Practice_-_recurrent_positives
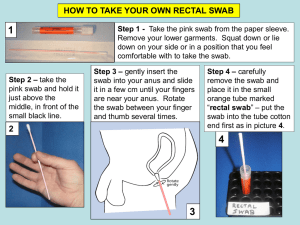
advertisement

Treatment in Practice PREPARED BY What this session includes • Diagnosing and managing sore throats – The use of throat swabs – Update on antibiotics for Strep A – What to do with recurrences – Tips on taking on taking antibiotics – Storage of antibiotics Diagnosing and managing Strep A sore throats • Difficult to always differentiate clinically between strep A and viral sore throats • A throat swab is the gold standard for identifying the presence of strep A in the throat – however cannot differentiate whether there is infection or carriage When do you take a throat swab • All symptomatic children in school sore throat management clinics should have a throat swab taken and results received before commencement of antibiotics • In rapid response clinics – may consider giving antibiotics to high risk individuals without a throat swab • If throat swab taken, good practice to let client know results of swab; consider discontinuing antibiotics if throat swab GAS negative • The Heart Foundation does not routinely recommend re-swabbing patients after an antibiotic course is completed Treating Group A streptococcal sore throats (based on 2014 Heart Foundation guidelines) First line treatment Amoxicillin orally for 10 days < 30 kg: 750 mg daily ≥ 30 kg: 1000 mg Benzathine penicillin G, intramuscular injection, single dose < 30 kg: 450 mg (600,000 Units ≥ 30 kg: 900 mg (1,200,000 Units) Definite or possible anaphylaxis to penicillin or amoxicillin Erythromycin ethyl succinate orally for 10 days 40 mg/kg/day in 2 – 3 doses Note: • Decrease in maximum dose of amoxicillin from 1500mg to 1000mg • Maximum dose for erythromycin ethyl succinate – 3200 mg (Medsafe datasheet) to 4000 mg (New Zealand Paediatric Formulary) Managing children who keep presenting with a GAS positive sore throat - a challenge for all • Concern expressed repeatedly at meetings, DHB visits, question times • Typically child or young person who presents with recurrent sore throats and throat swab is positive each time • Sometimes post treatment swab is positive • Causing concerns to parents • Undermining the relationship between the professional and the parent/patient Confirming a Strep A carrier • Suspect if closely spaced symptomatic recurrences of pharyngitis with a positive throat swab i.e. child with repeated sore throats who always has a positive swab • Confirm by testing to check after an effective course of antibiotic has been delivered – Verbal assurance of adherence? – Directly Observed Therapy? – IM injection? • If positive swab after a known effective course of antibiotics – they are a Strep carrier What does being a Strep carrier mean? • Not alone. Around 1 in 8 school age children in NZ are strep A carriers • Very little or no risk for Rheumatic Fever • Can transmit the strep A to others who may become infected and therefore at risk of RF – Especially if also have a cough – But much less likely to that those have an actually infection • Don’t swab asymptomatic children (GAS positives most likely carriage) What do you do when you find a Strep carrier • Explain to the child and/or caregiver what being a carrier means • To help them avoid passing the bug onto household contacts – Emphasise the importance of sneeze and cough etiquette – Highlight the importance of not crowding childrenespecially when they sleep • Refer to your GP or nurse practitioner to decide whether and how to treat Deciding whether to treat a carrier • Unwise to treat a known carrier if obvious viral symptoms - cough and runny nose • Don’t keep giving courses of oral amoxicillin to people who are GAS carriers - it won’t make any difference to the child and may contribute to antibiotic resistance • Refer to your lead GP or nurse practitioner • Ministry and NHF are producing a fact sheet and guidance to assist GPs and nurse practitioners Should carriage be treated? • Possible to “clear” the strep A carriage – Which reduces the confusion – But takes powerful antibiotics – Theoretically carriage may protect against infection with strep A • Clear once. • Key question is whether to do it again and what to do if not • Fact sheet will pick up these issues For more information Gregory P deMuri and Ellen R Wald. The Group A Streptococcal Carrier State Reviewed: Still an Enigma. Journal of Paediatric Infectious Diseases Society April 2014 Most school-aged children are able to learn to swallow tablets and capsules Possible Barriers • Anxiety • Strong gag reflex • Texture, size and shape Techniques for swallowing tablets and capsules • Ask the child to have a drink of water or their favourite drink to moisten their mouth • Place the tablet or capsule into the centre of the child’s mouth • Ask the child to take a big sip of their drink, and then swallow Top tips • Yoghurts and thick drinks • A straw • A small spoonful of apple sauce or ice cream Capsules Leaning forward when swallowing can help the capsule go down • Ask the child look down at the floor instead of up at the ceiling • Slip the capsule into the centre of the child’s mouth. • Ask the child to take a big sip of their favourite drink or water while still looking at the floor. The capsule should float to the back of the child’s mouth and roll down their throat with the drink Practice Makes Perfect Encouraging children to swallow tablets and capsules: http://www.bpac.org.nz/Supple ment/2014/September/pillswall owing.aspx Giving medicines to children: http://www.pharmac.health.nz/medi cines/medicines-information/bestuse-of-medicines/giving-medicinesto-children#capsules