Preferred Choice - Virginia Department of Health
advertisement

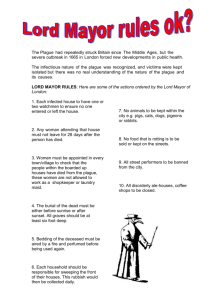
Virginia Department of Health Plague: Guidance for Health Care Providers Key Medical and Public Health Interventions After Identification of a Suspected Case 1. Clinical Manifestations Plague is caused by the bacteria Yersinia pestis and has three forms: bubonic, pneumonic, and septicemic. Pneumonic plague is communicable from person-to-person by respiratory droplets. In rare circumstances, contact with exudates from buboes has been a source of plague transmission. A small number of patients with bubonic or septicemic plague may develop secondary pneumonic plague, which can then be spread by respiratory droplet. A. Bubonic Plague Incubation Period – 2-8 days Symptoms and signs – Patients develop sudden onset of fever, headache, weakness, chills and swollen, extremely painful lymph nodes (buboes). Buboes generally develop in the nodes that drain the site of the initial infection (typically in the groin, axilla or cervical region). Nausea, vomiting, and diarrhea are common. Patients may develop secondary septicemic plague or secondary pneumonic plague. B. Pneumonic Plague Incubation period – typically 2-4 days (range 1 to 6 days) Symptoms and signs – patients exhibit acute and often fulminant onset of high fever, malaise, headache, myalgias, and cough with production of sputum that is initially watery, before becoming bloody. Pneumonia rapidly progresses to dyspnea, stridor, and cyanosis. Patients develop respiratory failure, shock, and ecchymosis. Nausea, vomiting, diarrhea, and abdominal pain may be present. C. Septicemic Plague Incubation Period – 1-7 days Symptoms and signs – clinically resembles septicemia caused by other Gram-negative bacteria. Patients are febrile and often have chills, headache, malaise, and gastrointestinal disturbances. May progress rapidly to septic shock, meningitis, and coma. Patients may develop secondary pneumonic plague. 2. Identification and Isolation of Cases Plague does not occur naturally in Virginia, but it does occur rarely in the western United States and in other parts of the world. If any cases of plague were to be reported in Virginia, it would be very important to determine recent travel history to high-risk areas (New Mexico, Arizona, Nevada, Oregon, Colorado and California, and areas of Africa, Asia and South America). If travel history does not implicate a possible source of exposure, bioterrorism may be suspected. Early indications that plague may have been used as a biological weapon include: occurrence of cases in locations not known to have enzootic infection; occurrence of cases in persons without known risk factors; absence of prior rodent deaths; and sudden outbreak of illness in patients presenting with severe pneumonia and sepsis. Page 1 of 5 Updated 07/27/2003 Use standard precautions for all types of plague. Additionally, for pneumonic plague, follow droplet precautions until the patient has had 48 hours of appropriate antibiotics and shown clinical improvement: Patients should be placed in a private room and persons entering the room should wear a surgical mask, especially important when within six feet of the patient (N-95 mask not required, but is also protective). Gloves, gown, and eye protection should also be used; Patients should remain isolated during the first 48 hours. When private rooms are not available, cohort symptomatic patients with similar symptoms and the same presumptive diagnosis; Limit movement and transport of patients and place a surgical mask on the patient when transport is necessary; and Practice concurrent disinfection of sputum and purulent discharges (also for bubonic plague). If applicable, use an insecticide to rid patients and their clothing of fleas. 3. Handling Laboratory Specimens Routine laboratory tests other than culture may be performed at Biosafety Level 2, but any procedure that may generate an aerosol should be performed within a biosafety cabinet. Cultures or manipulations of cultured material should be performed at Biosafety Level 3. The Division of Consolidated Laboratory Services (DCLS) should be consulted about specimen collection and processing. The DCLS Emergency Services Officer can be reached 24 hours a day/7 days a week at 804-418-9923. Sample collection instructions are shown below. Table 1. Sample Collection for Suspected Plague Samples Amount Type of Plague Instructions Bronchial/tracheal wash or induced sputum Lymph node aspirate (bubo) 5-10 cc Pneumonic 1-2 cc Bubonic Blood 10 cc Septicemic Cerebrospinal Fluid 5-10 cc Serum Acute and convalescent 14 days apart 1 gram Any type if meningeal symptoms Septicemic or Bubonic Specimen of choice for pneumonic plague. Place in sterile container. Store and ship refrigerated. Specimen of choice for bubonic plague. Place in sterile container. Ship to lab ASAP; if more than 2 hours, refrigerate. Blood isolator tube or aerobic culture bottle. Ship at room temperature. Transport to lab within 16 hours. Ship to lab ASAP; if more than 2 hours, refrigerate. Tissue: liver, spleen, lung or bone marrow Page 2 of 5 Any fatal case Collect in red top or tiger top tube. Remove serum and place in sterile tube, then store frozen. Place in sterile container; moisten with sterile broth or saline. Ship to lab ASAP at room temperature. If more than 2 hours, freeze and ship on dry ice. Updated 07/27/2003 Isolates from the respiratory tract, blood or lymph node containing the major characteristics below should be suspected as Y. pestis: Bipolar staining rod (Wright-Giemsa or Wayson) on direct smear Pinpoint colony at 24 hours on sheep blood agar Non-lactose fermenter, may not be visible on MacConkey agar or eosin methylene blue at 24 hours Oxidase and urease negative Catalase positive Growth often better at 28C Additional laboratory guidance is available in the CDC publication Level A Laboratory Procedures for Identification of Yersinia pestis, available at: http://www.bt.cdc.gov/agent/plague/index.asp 4. Diagnostic Procedures Table 2 lists the epidemiology, clinical signs, and laboratory studies for a diagnosis of pneumonic plague infection. Table 2. Diagnosis of Pneumonic Plague Infection* Category Indications of a possible bioterrorism event Clinical Manifestations Laboratory Studies Findings Sudden appearance of several persons with fever, cough, shortness of breath, hemoptysis and chest pain. Any case of pneumonic plague in the United States should raise concern. Gastrointestinal symptoms (e.g., nausea, vomiting, abdominal pain and diarrhea) Patients have fulminant course and high mortality Tachypnea, dyspnea, and cyanosis Pneumonic consolidation on chest examination Sepsis, shock and organ failure Infrequent presence of cervical bubo Purpuric skin lesions and necrotic digits only in advanced disease Sputum, bronchial/tracheal wash or blood Gram-negative bacilli with bipolar appearance (like a safety pin) on Wright, Giemsa, or Wayson stain Pulmonary infiltrates on chest radiograph Additional tests are available at DCLS and CDC *Excerpted from: Inglesby TV et al. Plague as a Biological Weapon: Medical and Public Health Management. JAMA. 2000;283(17):2281-2290. 5. Treatment and Prophylaxis Supportive care combined with the rapid administration of parenteral antibiotics is the key to successful management of plague. Pneumonic and septicemic plague are almost always fatal if antibiotics are not started within 24 hours of onset of symptoms. Standard treatment should continue for 10 days. Treatment regimens are shown in Table 3. Page 3 of 5 Updated 07/27/2003 Close contacts of pneumonic plague patients are individuals with contact at less than 6 feet when the case is symptomatic and has not yet received 48 hours of antibiotic therapy. Close contacts (including household and healthcare workers) should receive prophylaxis for seven days and should be placed under medical surveillance for seven days. Contacts who develop a fever or cough should seek prompt medical treatment, notifying the healthcare facility before arrival so that proper infection control precautions can be implemented. Contacts who refuse prophylaxis should be quarantined for 7 days after exposure. Prophylaxis regimens are shown in Table 3. Table 3. Working Group Recommendations for Treatment and Prophylaxis of Patients with Plague Standard treatment should continue for 10 days and prophylaxis should continue for 7 days. Oral therapy should be substituted when clinically appropriate. Standard Treatment Prophylaxis Regimens in this column may also be used for treatment in severe circumstances when standard IM or IV treatment is impractical or unavailable. Adults Preferred Choices: Preferred Choices: Streptomycin, 1 g IM twice daily,* or Doxycycline, 100 mg orally twice daily, or Gentamicin, 5 mg/kg IM or IV once daily or 2 mg/kg Ciprofloxacin, 500 mg orally twice daily loading dose followed by 1.7 mg/kg IM or IV 3 times daily Alternative Choice: Chloramphenicol, 25 mg/kg orally 4 times daily‡ Alternative Choices: Doxycycline, 100 mg IV twice daily or 200 mg IV once daily, or Ciprofloxacin, 400 mg IV twice daily, or Chloramphenicol, 25 mg/kg IV 4 times daily*‡ Children Preferred Choices: Preferred Choice: Streptomycin, 15 mg/kg IM twice daily (maximum Doxycycline, adult dosage if > 45 kg, if < 45 kg, then daily dose 2 g), or give 2.2 mg/kg orally twice daily, or Gentamicin, 2.5 mg/kg IM or IV 3 times daily Ciprofloxacin, 20 mg/kg orally twice daily, not to exceed 1 g/day Alternative Choices: Doxycycline, adult dosage if > 45 kg, if <45kg give 2.2 Alternative Choice: mg/kg IV twice daily (maximum 200 mg/d), or Chloramphenicol, 25 mg/kg orally 4 times daily (not if Ciprofloxacin, 15 mg/kg IV twice daily, not to exceed child < 2yrs) ‡ 1 g/day, or Chloramphenicol, 25 mg/kg IV 4 times daily (not if child < 2yrs) ‡ Treatment regimens shown are not necessarily approved by the FDA. *Not recommended for pregnant women. Other flouroquinolones can be substituted at doses appropriate for age. ‡ Higher concentrations (e.g., >25 ug/ml) are associated with increased risk of reversible bone marrow suppression. In addition, chloramphenicol can rarely cause irreversible bone marrow suppression. Children younger than 2 years of age should not receive chloramphenicol. 6. Vaccine U.S. licensed vaccine for plague was discontinued in 1999 and is no longer available. Page 4 of 5 Updated 07/27/2003 7. Decontamination If a release of plague used as a biological weapon is suspected, instruct potentially exposed individuals to: remove contaminated clothing and store in labeled, plastic bags; handle clothing minimally to avoid agitation; and shower thoroughly with soap and water. Initiate post-exposure prophylaxis when appropriate. Hospital rooms of patients with plague should receive terminal cleaning consistent with standard precautions, and clothing or linens contaminated with body fluids should be disinfected according to hospital protocol. Potentially contaminated material should be cleaned with a solution of 1 part household bleach to 9 parts water (0.5% sodium hypochlorite solution). 8. Postmortem Practices If plague is suspected as a cause of death, the regional office of the state medical examiner should be immediately notified. Consultation should occur regarding: whether an autopsy should be conducted, parties responsible for conducting the autopsy, and proper personal protective procedures to follow. Contact with and transport of body should be limited to trained personnel. 9. Public Health Measures A. Suspected cases of plague should be reported immediately to hospital epidemiology/infection control, who in turn should notify laboratory personnel, other medical care providers and public health. B. Arrange for laboratory testing by consulting with DCLS at 804-418-9923 (24 hour/7 day). C. Designated public health authority should begin an epidemiologic investigation immediately. a. Identify and treat close contacts of pneumonic plague patients with appropriate antibiotic. b. Put all contacts of cases of pneumonic plague under surveillance for illness for seven days. Individuals who develop a fever or cough should seek prompt medical treatment. Contacts who refuse prophylaxis should be placed under quarantine for seven days. c. If appropriate, flea and rodent control should be a part of the investigation and follow-up. Information excerpted from Inglesby TV; Dennis DT; Henderson DA, et al. Plague as a Biological Weapon: Medical and Public Health Management. JAMA. 2000;283(17):2281-2290 and Chin, J. Control of Communicable Diseases Manual, 17th edition; 2000; Plague; 381-387. Page 5 of 5 Updated 07/27/2003