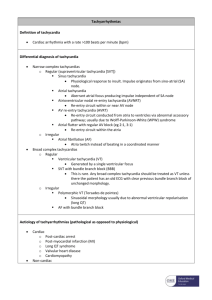
Supraventricular Tachycardia
advertisement

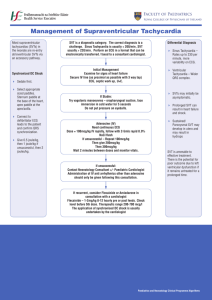
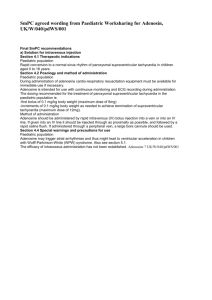
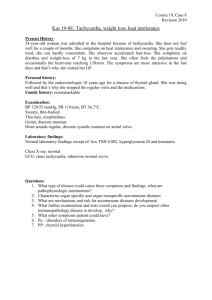
Paediatric Clinical Guidelines Cardiology 2.1 Supraventricular Tachycardia Short Title: Supraventricular Tachycardia Full Title: Date of production/Last revision: Guideline for the investigation and management of supraventricular tachycardia in children and young people August 2008 Explicit definition of patient group to which it applies: This guideline applies to all children and young people under the age of 19 years. Name of contact author Dr Muthu Dhanarass, Paediatric SpR Dr Damian Wood, Consultant Paediatrician Ext: 67319 August 2011 Revision Date This guideline has been registered with the Trust. However, clinical guidelines are 'guidelines' only. The interpretation and application of clinical guidelines will remain the responsibility of the individual clinician. If in doubt contact a senior colleague or expert. Caution is advised when using guidelines after the review date. Supraventricular Tachycardia Please note there is a separate neonatal supraventricular tachycardia guideline for infants less than 28 days of age. Introduction SVT is the commonest symptomatic arrhythmia in children Typically o The heart rate is usually above 200. o 12 lead ECG shows a narrow complex, regular tachycardia. o If present, p waves are seen for each QRS complex. Assessment History: Infants – pallor, tachypnoea, poor feeding, irritability Older children – palpitations, chest discomfort, dizziness Often non-specific such as “feeling funny” Examination: Heart rate over 180 bpm (over 220/min in infants) No beat to beat variation as in sinus tachycardia Hypotension may be present Heart failure (esp. in infants) Investigations: 12 lead ECG if suspected Urgent cardiology referral if tachycardia is broad complex Or irregular Other – if on medication, measure levels i.e. Digoxin, Theophylline. Management Move to Resuscitation area when safe to do do Assess ABC Check BP and start continuous cardiac monitoring with paper recording Oxygen Saturation. 12 lead ECG-Rhythm strip (P waves may not be visible) Muthu Dhanarass Page 1 of 3 October 2004 Paediatric Clinical Guidelines Cardiology 2.1 Supraventricular Tachycardia Algorithm for the Management of Supraventricular Tachycardia If Shocked 1. Call for senior help, 2. Make sure airway equipment available IF HAEMODYNAMICALLY STABLE – consider before drug treatment 1. Vagal manoeuvre a. Bag of ice on face, Max. Duration 15 secs. (Ice cubes available in Children’s Emergency Department Refrigerator ) b. Facial Immersion – wrap infant in towel, and immerse the whole head in iced water for 5 seconds. No need to obstruct the mouth or nose. c. Unilateral carotid massage 2. Valsalva in older children DO NOT USE EYEBALL PRESSURE IN CASES OF SVT IV Access – in large PROXIMAL vein preferably with a 3 way tap Muthu Dhanarass Page 2 of 3 October 2004 Paediatric Clinical Guidelines Cardiology 2.1 Supraventricular Tachycardia Adenosine Prepare all doses of adenosine (as in algorithm) and 5ml saline flushes Start with adenosine 100mcg/kg Turn on ECG paper recorder RAPIDLY administer adenosine as push, followed IMMEDIATELY by saline flush If rhythm does not revert to Sinus rhythm, repeat Adenosine at increasing doses. Maximum dose is 300mcg/kg (<1 month); 500mcg/kg (>1 month) up to maximum of 12 mg. For adolescents adenosine doses can be rounded as 3mg followed by 6mg and then 12mg Perform ECG post reversion Adenosine side effects – flushing, nausea, chest tightness. Caution should be taken if patients are on Dipyrimadole – it prolongs the action of the adenosine. The dosage of adenosine should be reduced by a factor of 4. IF THESE MEASURES FAIL, Contact the ON-CALL ACUTE PAEDIATRIC CONSULTANT and discuss with Dr Thakker or Paediatric Cardiologist at Glenfield Hospital(0116 2871471) and fax the ECG to cardiac centre Other Drugs Used in the Treatment of SVT One of the following drugs may be suggested. But many of them are unsafe to use in the same patient. The patient can be treated by external cardioversion with a general anaesthesia, but we strongly recommend discussion with the on call Paediatric Cardiologist before administration of drugs other than Adenosine. Give on PICU only, monitoring BP and ECG closely. Make sure defibrillator and pacemaker facilities available. Amiodarone: Used in refractory atrial tachycardia, (Dose 5mg/kg over 30mins, Dilute in 4ml/kg of 5% Dextrose) Procainamide: Loading dose 15mg/kg over 30 to 60 mins with ECG and BP monitoring. STOP if QRS complex widens in ECG or Blood pressure falls. Flecainide 2mg/kg IV over 20 minutes Particularly useful for WPW STOP if new arrhythmias in ECG and changes in QRS. Verapamil Should not be given if <1 year of age (risk of irreversible hypotension, asystole) Beta-blocker (eg.propronolol) used within the last 24 hrs if there are signs of heart failure or poor LV function Administer as slow IV o Age 1-2 years, 100 to 200 mcg/kg (max 2g) over 3 mins o Over 2 years 100 to 300 mcg/kg (max 5g) STOP infusion if sinus rhythm achieved or BP drops greater than 10mmHg Muthu Dhanarass Page 3 of 3 October 2004