Lesson 23 Ethanol: Student notes ethanollessonStudent15
advertisement

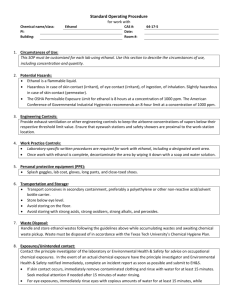
Ethanol In September 2010, an advisory board recommended that the National Institute on Drug Abuse (NIDA) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA) merge. The new addictions institute now rightly places addiction into both the alcohol and other drug realms and recognizes that the changes that underlie addiction are universal. The phrase “drug and alcohol” is confusing to many – because alcohol IS a drug. To center the focus of addiction into one institute may not only cut administration it may improve communication and speed up research on this topic. This lesson is named "ethanol" because there are really many types of alcohol. But it is ethyl alcohol, or ethanol, that most people are talking about when they use the word alcohol. Ethanol is our one "legal" intoxicant in the U.S.. The use of ethanol has been questioned in the past, but the Prohibition did little to dissuade people from using it. Thus ethanol's status as "legitimate" is quite engrained. So much so that for many, calling it a "drug" is even contradictory. But there can be no doubt that ethanol IS a drug and none either that it is the gateway drug - a drug whose use leads to the use of other "harder" drugs. Since ethanol is such a well-known and widely-used drug, you should anticipate that this lesson will take a bit longer to complete than previous drug lessons. Lesson: Ethanol Guiding Questions 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Why is ethanol addictive? What are the recommendations about ethanol rehabilitation? Why does ethanol impact brain and many other body systems? Which neurotransmitters are particularly impacted by ethanol? Why do different people respond to ethanol in different ways? Why does ethanol make a person: feel high? feel sleepy? forget? lose balance? suffer liver damage? How does ethanol-related depolarization happen and how does that relate to opiates? What is a “dose” of ethanol? How many doses are considered “binge” drinking? How and why does ethanol metabolism vary between individuals? Who is at risk for alcoholism? How does ethanol impact brain function and volume? Key Terms 1 Ethanol Kindling Alcohol dehydrogenase and aldehyde dehydrogenase Blood alcohol content (BAC) J-curve “French paradox” Resveratrol Cirrhosis Diuretic Fetal alcohol syndrome Antabuse Activity One: Web Site Review 1) Please review the overview page on alcohol from NIDA. Guiding questions When one consumes alcohol, which organs in the body are affected? What is binge drinking and how common is it? http://www.nida.nih.gov/drugpages/alcohol.html 2) Next review several pages at “HowStuffWorks” site on alcohol. Review pages 3 through 13. While this is a lot to review, anticipate that it will take you through almost all of the lesson. Guiding questions: What is the structure of ethyl alcohol? Is ethanol fat soluble? What influences how fast ethanol gets into the blood? What metabolizes ethanol and what are the metabolites? What are the effects of ethanol and how do they progress at higher and higher doses? What areas of the brain are most impacted (even at low doses)? If you affect decision making centers early on, what could that mean about going from low dose to high dose? What are the long-term concerns when a person becomes an alcoholic? What underlies the development of tolerance in a steady drinker? http://health.howstuffworks.com/wellness/drugs-alcohol/alcohol.htm 3) Lastly, visit the mouse party site again. The mouse with the bottle is the one that explains ethanol. 2 Ethanol Guiding questions: What is ethanol's "double sedative punch"? Note - it is INCORRECT that ethanol interacts directly with GABA and glutamate receptors (this site is largely correct). What brain functions are very sensitive to ethanol's impact? http://learn.genetics.utah.edu/content/addiction/drugs/mouse.html Activity Two: What is Ethanol? Why do we use Ethanol? Ethanol is a very small molecule that is the intoxicating portion of any alcoholic drink. You will find ethanol, in differing concentrations, in beer, wine, whiskey, and related drinks. People use ethanol for a variety of reasons. In the U.S., it is a social "lubricant". It is served at parties and gatherings. Some enjoy the taste, others find it relaxes them and makes a social encounter more comfortable and fun. In many cultures it is also the beverage that accompanies a meal. It aids digestion in modest amounts, and, again, relaxes a user. Some use ethanol in greater amounts to get euphoric and a little out-of-control. Ethanol is a highly effective "disinhibiting" drug. Others use these greater amounts to sedate them - aid sleep. At yet higher doses, ethanol will bring on amnesia and other undesired effects. The problem with an intoxicant that disinhibits is that the normal inhibitions on "uh oh, I'm getting out of control, I should slow down" are inhibited and we drink more and more. Some people use ethanol because they are addicted and cannot stop. Ethanol addiction is very powerful and the physical dependence that is established in long-term drinkers is very dangerous to defy (more on this in activity six). TEST OF CONTENT In Peru, the social lubricant (served at gatherings and festivals) is cocaine tea. In the U.S., the social lubricant is ethanol. How do these drugs compare from the perspective of brain function and symptoms? Activity Three: How Is Ethanol Administered? How Much Ethanol is Used? Ethanol is administered orally. Whether it is in a beer or a shot of whiskey, the ethanol molecule is the same. How much is used varies from person to person. About 90% of the alcohol consumed by people under 21 results from binge drinking.1 The Center for Disease Control and Prevention defines binge 1 http://www.cdc.gov/alcohol/fact-sheets/binge-drinking.htm 3 Ethanol drinking as use that results in blood alcohol content (BAC) to 0.08 or higher. For women, this means consuming 4 drinks within a 2-hour interval. For men, consumption of 5 drinks within 2 hours can lead to this BAC. A BAC of 0.5 or higher is lethal for most of us. This high a blood concentration occurs with steady consumption of 15 or more drinks (again, depending upon previous experience, health, nutritional status, and other drugs consumed). Ethanol added on to ANY depressant shrinks the therapeutic index synergistically. Visit NIDA's page found at http://rethinkingdrinking.niaaa.nih.gov/WhatCountsDrink/HowMuchIsTooMuch.asp Click on the following sub-pages: What's a "standard" drink? How many drinks are in common containers? (Optional - take the survey entitled "what's your pattern"? TEST OF CONTENT What is the relationship between "proof" and alcohol concentration (% of the volume that is alcohol and not water)? . A 12-ounce beer, which is 5% alcohol, is 0.6 ounces of pure alcohol. 12 ounces x 5% = 0.6. Follow this mathematical logic to discover how many "drinks" one is having if one consumes 1.5 ounces of 160 proof tequila in a margarita. Activity Four: Bioavailability of Ethanol Ethanol is metabolized in two steps. First, ethanol is converted to acetyl aldehyde (often referred to just as “aldehyde”) by an enzyme called alcohol dehydrogenase (ADH). Note that it is not incorrect for this enzyme to have a generic (alcohol) name because the enzyme also metabolizes other alcohols. Ethanol = C2H5OH which loses two hydrogens (de-hydrogen-ase = hydrogen-removing-enzyme) to become acetyl aldehyde = CH3CHO. Aldehyde is then converted into acetic acid (CH3COO-) by a second hydrogen-removing enzyme, aldehyde dehydrogenase (ALDH). Thus, both enzymes are necessary to metabolize ethanol into a form that can be excreted. While aldehyde does not have an intoxicating impact, it does have an impact that is associated with feeling ill. Individuals who make the first conversion easily but the second conversion with more difficulty find the ethanol experience to be most uncomfortable (see activity 9). 4 Ethanol image source themedicalbiochemistrypage.org TEST OF CONTENT There is a CH3 group on ethanol and both of its metabolites. Why isn’t it conventional to say that these molecules have a methyl group? What symptoms would you predict for someone who has a lot of ADH activity? What about insufficient ADH activity? If a person overdoses on methanol or isopropanol, the treatment is ethanol. All three are metabolized by alcohol dehydrogenase. Why would ethanol administration be helpful? Activity Five: Where Does Ethanol Bind? Then What? Ethanol doesn’t quite bind ANYTHING. Its size and chemical properties enable it, however, to sink into and permeate almost every membrane of every cell. Like a wine marinate for food, ethanol “marinates” membranes. This causes the proteins embedded within those membranes to function differently. Because membranes enclose all cells in the body – the impact of ethanol is extremely broad (not just a brain issue). But ethanol does not bind to these membrane proteins! If asked what ethanol binds to – it’s a trick question! Among the membrane proteins affected by an ethanol-“marinated” membrane, four are particularly important. Two are ion channels and two are neurotransmitter receptors. The ion channels impacted by ethanol are those that need to open and close quickly in order for an action potential to move down the neuronal membrane. These channels, the sodium channel and the potassium channel, open to enable the exchange of ions during the action potential. In the presence of ethanol, the channels are sluggish. They respond to change in membrane potential and open more slowly. The neurotransmitter receptors impacted most by ethanol are the ones that bind to GABA and glutamate. GABA is an inhibitory neurotransmitter while glutamate is excitatory. The impact of ethanol to a neuron via these receptors is, however, the same: ethanol causes neurons to be less likely to engage in an action potential. Since GABA is an inhibitory neurotransmitter, ethanol must impact this receptor by enhancing GABA binding. And glutamate, an excitatory neurotransmitter, is inhibited from binding in the presence of ethanol. The easiest way to think about this is that, with the exception of GABA, ethanol diminishes function of the channel or receptor. But GABA is fairly unique. GABA binds 5 Ethanol relatively poorly to its receptor in normal situations. Ethanol changes the membrane in which the GABA receptor sits which changes the receptor, making it a better fit for GABA. Ethanol serves as a match maker – enhancing the ability of GABA to bind to its receptor. The GABA receptor is a chloride channel. When GABA binds, chloride is allowed to flow into a neuron, making it more negative on the inside and farther away from threshold (hyperpolarized). TEST OF CONTENT Contrast hyperpolarization from ethanol to previously learned hyperpolarization from opiates. There are two main differences. Activity Six: Why Is Ethanol Addictive? Ethanol is extremely addictive. Among all the drugs you will study, alcohol causes the most pervasive and slow-to-reverse adjustments in human physiology. Since ethanol influences virtually all membranes of all cells, the entire body is impacted by ethanol. The body adapts to life in an "ethanol marinated" world and the withdrawal symptoms upon removal of the marinate are very difficult to tolerate and even life-threatening. Between 5% and 25% of people detoxifying from heavy ethanol consumption actually die during withdrawal! It is important to get physician help with this process. It is unwise to repeatedly detoxify and then resume drug use. Each episode of withdrawal gets progressively worse, a phenomenon called "Kindling". 2 Ethanol use leads to development of tolerance. As the body adjusts to the presence of the drug, more ADH and ALDH are produced so that more efficient metabolism is found among regular users. This causes increased drug clearance and reduced drug effect (resulting in the decision to use more drug). Ethanol use leads to euphoria for a number of reasons. Interference with glutamate AND GABA pathways contributes to dopamine release in the nucleus accumbens. But additionally, alcohol metabolites have the ability to stimulate opiate receptors when combined with monoamines. 3 Ethanol abuse is costly. In the U.S., we spend >$68 million a year on harm to self and others as well as programs that help an alcoholic break their ethanol addiction. TEST OF CONTENT Which phrase best explains “Kindling”? 2 3 http://www.ncbi.nlm.nih.gov/pubmed/11324233 http://www.ncbi.nlm.nih.gov/pubmed/2990502 6 Ethanol Early attempts to quit use of ethanol lead to greater withdrawal symptoms experienced by later attempts Ethanol becomes more addictive with repeated use Ethanol use kindles the craving to use other “hard” drugs Activity Seven: Does Ethanol do ANY Good? Beyond its “usefulness” as a social lubricant, ethanol has a number of surprising health benefits. But before going into that, bear in mind that these benefits come from LOW doses. In fact, with regard to Indicators of poor health health outcomes, ethanol displays a “J curve” . Ethanol dosage People who consume NO ethanol have been shown to have more life-threatening health conditions that people who consume 1 – 2 drinks a day4. This “French Paradox” was named because despite the rich nature of a French diet, people in France suffered less from cardiovascular illness than people from cultures with more ethanol use. Because there are SO many variables that influence a condition, such as cardiovascular health, it can be very difficult to determine if any one life-style choice is implicated. Imagine trying to do a dose-response curve for ethanol studied in a “single variable” method. You would have to find people who consume different doses of ethanol, but whom all have the same diet, same occupation, same level of stress, same genes, (you get the idea). The need to know about life style and health outcomes was profound enough that an alternate method of study is most useful. Epidemiology is the study that replaces great number of individuals with control over single variables. These subjects will indicate their own habits of relevance (such as ethanol consumption) and will check in with the data collectors frequently to update them on, for instance, health outcomes. From this analysis, patterns are found. And because there are so 4 http://www.cdc.gov/alcohol/faqs.htm 7 Ethanol many subjects, the statistical significance of these patterns is evaluated. From these epidemiology studies, such as the 5Framingham “Heart” study, the “French Paradox” was validated. So what was it in ethanol that improved cardiovascular health? You might wonder if it relates to the calming (sedating) influence that ethanol has on a person. Stress certainly elevates blood pressure: therefore stress-relievers must promote cardiovascular health. This was studied by examining the cardiovascular health of beer drinkers compared to wine drinkers compared to whiskey drinkers (for instance). Some measure of benefit is seen regardless of the ethanol form. But darker beverages, such as red wine or dark rum, were seen to be particularly helpful. Part of the benefit from darker beverages is that like darker colored foods (pomegranate, cranberry, blueberry) , dark beverages have more antioxidants. 6But another ingredient was implicated because red wine was so particularly beneficial. One ingredient within red wine, named Resveretrol (rez-VAIR-a-troll), has been studied extensively, and marketed nearly as extensively. One study on reveratrol prolonged the lifespan of fish by 59%7. Another showed that obese mice, forced to consume a high calorie, high fat diet, would not experience shortened longevity expected for that diet IF they consumed resveratrol as well. Death rate in the resveratrol mice was cut by 31% 8and additionally, other obesity-related complications, such as diabetes, were seen less frequently. Other studies have shown that ethanol helps keep blood sugar levels lower9, accounting for lower diabetes incidence. The same studied also followed blood lipids as related to ethanol consumption. Low dose of ethanol can increase total cholesterol levels a modest amount, the levels of the “good” cholesterol (HDL) increase steeply, suggesting that as “good” cholesterol increases, “bad” cholesterol does not, or lowers with ethanol consumption10. But returning to dosage, the dosage of resveratrol fed to the obese mice was the equivalent of drinking 100 glasses of wine a day! So while resveratrol may indeed be a “fountain of youth”, the adverse effects of such a high dosage have not been studied and getting your resveratrol in the form of wine comes with obvious disadvantages. TEST OF CONTENT Explain the “J curve” of ethanol exposure and health Explain the “J curve” of ethanol exposure and health. 5 http://www.framinghamheartstudy.org/ http://lpi.oregonstate.edu/f-w00/flavonoid.html 7 Valenzano, et al. (2006) Current Biology 16:296-300. 8 Baur et al. (2006) Nature 7177:337-342 9 Brand-Miller American Journal of Clinical Nutrition 2007 6 10 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1059549/ 8 Ethanol Activity Eight: What are Ethanol’s Harmful Side Effects? Review the table showing the adverse health outcomes associated with ethanol consumption. Ethanol related illnesses account for the 4th leading cause of death in the US. For people who consume ethanol on a regular basis, it is estimated that they have lost 10 – 12 years from their expected life-span. Health outcome Relationship to Ethanol Explanation Liver damage, Prolonged, and / or high doses Ethanol metabolic enzymes must be produced by cirrhosis, liver of ethanol result in damage to the liver. Excessive use leads to excessive work cancer the liver. load on the liver and untimely death of cells. “Gateway drug” Ethanol users and abusers are Ethanol is readily available and a high percentage 11 more likely to use other “hard” of young adults consume it. drugs.12 Hypertension Ethanol is associated with Ethanol causes the adrenal glands to increase the elevation of blood pressure. release of dissolved salts in the blood which leads to osmosis – bringing more water into the blood – which leads to a higher blood pressure (more volume in the same, small space). Vasodilation Peripheral areas “flush” and Ethanol causes increased volumes of warmed heat. This can lead to increases blood are directed to these areas by widened in heat exchange with the blood vessels. environment. Keep this in mind when using ethanol in cold weather or in a hot tub! Dehydration Ethanol causes user to increase Ethanol alters the availability of water to tissues. urinary output. This is a large part of why people get hangovers. Balance and Ethanol causes users to be Coordination and balance are related. Both take coordination uncoordinated and have nervous system feedback about posture and difficulties with balance. motor adjustments as we move. Nervous system is depressed due to hyperpolarization. Balance 11 Explanatory video at - cirrhosis http://video.about.com/alcoholism/Cirrhosis-of-Liver.htm 12 Blaze-Temple, D.; Kai Lo, S. (1992). Stages of drug use: a community survey of Perth teenagers. British Journal of Addiction, 87, 215-225. 9 Ethanol also requires a particular density of inner-ear fluid which is altered when ethanol is consumed. Cognitive Ethanol is associated with Part of the rationale here is related to performance reduction of cognitive hyperpolarization – a temporary (while using performance by many drug) loss of brain function. But part goes way measurements and also is beyond that. Tapert and colleagues estimate a associated with memory loss 10% reduction in cognitive function in people who (amnesia). use as little as ONE episode of consuming 4-5 drinks.13 This could, in part, be due to neurotoxicity described briefly below. It is also due in part to malnutrition (see below). Brain matter Ethanol users have been Brain scans on heavy users have identified these atrophy (or loss) shown to have reductions in reductions that are not specific to any area, but both white and gray matter wide-spread. The mechanism for the volume. neurotoxicity is not known. Ethanol users are often Ethanol abusers get so many calories from malnourished. ethanol, they often don’t eat as much “real” food. Malnutrition Additionally, absorption of some nutrients is reduced in an ethanol users – in particular – vitamin B12 which is needed for, among other things, cognitive function. Gastrointestinal Ethanol irritates the GI track, Ethanol can be toxic to the cells lining the GI track. symptoms making a person feel ill or It can also influence stomach acid production. vomit Kidney function Ethanol stimulates urinary The increased kidney output puts a strain on the function (it is a diuretic) kidneys, leading to premature loss of kidney function. Fetal alcohol The babies born to women Ethanol arrives in the fetus through shared blood syndrome who use ethanol while supply. There is nothing about the placenta that pregnant have a characteristic screens fetal blood to reduce transmission of these suite of symptom: low birth toxins. Additionally, the fetus has a diminished 13 SOURCES: Susan F. Tapert, Ph.D., associate professor, psychiatry, University of California, San Diego, director of Substance Abuse/Mental Illness, VA San Diego Healthcare System; John R. Knight, M.D., associate professor, pediatrics, Harvard Medical School, director, Center for Adolescent Substance Abuse Research (CeASAR), Children's Hospital Boston; April 22, 2009, Alcoholism: Clinical and Experimental Research, 10 Ethanol Risk of accident weight, delay in reaching capacity (if any) to make alcohol dehydrogenase developmental landmarks, which effectively increase the ethanol half life in a irritability, and others. fetal body. Ethanol impairment is Disinhibition, lack of coordination, and responsible for 40% or more of diminished cognitive capacity lead to the making traffic fatalities. Loss of life or of unwise choices, slowed reaction time, and injury rates are elevated even if uncoordination (previously discussed). To Risk of cancer you don’t drive. Some prevent a friend who might have passed out from “accidents” involve the aspirating vomit – lay her in the “safe position” on aspiration of vomit. her side! Ethanol increases cancer risk, No evidence is available for carcinogenic impacts leading to an estimated 3% of of ethanol. It is possible that ethanol does not cancer deaths.14 This increase is directly result in cancer but an increase in other synergized by simultaneous life-style choices (such as nicotine use) that often use of ethanol and nicotine. accompany ethanol use. Acute system failure (as “Marinated” membranes and the proteins within opposed to failure due to long- them cannot function as needed to keep a person’s term exposure) happens at systems active. The brain stem neurons which high alcohol (all alcohols) result in a signal to lower the diaphragm and take doses. a breath are diminished in function, resulting in 15 Ethanol toxicity respiratory depression. Metabolites can, in some cases be even more toxic. A metabolite for methanol (a 1-carbon alcohol) is formaldehyde! Ethanol has been used for such a long time and by so many people, we probably have a particularly long list of bad side-effects because we have had an opportunity to study ethanol for so long. Despite this potential bias, the list of negative impacts is particularly impressive for a “legal” product. TEST OF CONTENT Compare the list of symptoms displayed by ethanol users. Rearrange the list to show long and short term concerns. Which require long-term ethanol use? “Antabuse” (disulphiram) is a product that inhibits aldehyde dehydrogenase. Explain who might use antabuse and why. 14 15 Liska, section 9.4.10 Liska, section 9.4.10 11 Ethanol Activity Nine: Individual Experience May Vary Both genes (nature) and environment (nurture) can influence the experience had while using ethanol and the likelihood of using ethanol. Nature Because the tendency to become an alcoholic are 5 times higher if you have a close family member who is an alcoholic, researchers and the public believed that alcohol abuse is a genetically controlled trait. Bear in mind, the family-resembles-family argument is weak! It is probably that seeing alcohol used and abused in a home will influence others in the home to seek escape through ethanol consumption. Ethanol use and abuse have been examined in correlation with different alleles of ADH (alcohol dehydrogenase) and ALDH (aldehyde dehydrogenase) genes. The strongest correlation is between alleles of ALDH that make POOR quantity/quality enzyme and the PROTECTION from alcoholism that is afforded by increasing the amount of aldehyde in the blood, and the consequent ill-feeling associated with that aldehyde. Similarly, the gene encoding the dopamine receptor is implicated in ethanol abuse, much as it was for cocaine (and many other euphoriants). In people who dopamine reception is diminished, additional stimuli that trigger dopamine release are craved. This reward-deficiency syndrome can lead to abuse of drugs as well as craving for activities that induce reward pathway stimulation such as sex, gambling, and gaming. In 2006, Mulligan et al. (supplementary reading) published a meta-analysis of candidate genes. These candidate genes were all expressed differently when a subject (mouse) comes from a family line of mice who prefer alcohol as compare to family lines of non-preferrers. In fact, such family lines have been established in several mouse strains. The authors took the mRNA made from transcription (a measure of active genes) and compared that mRNA for thousands of genes between preferring and non-preferring "siblings. The color red indicates when there is more gene expression for a gene in the alcohol preferring line while green indicates 12 Ethanol when there is more gene expression for another gene in the non-alcohol preferring line. Examine the figure from their paper. The panel on the left shows all the genes examined while the panel on the right highlights the genes showing the most preference-dependent change. For instance, the Scn4b gene (star) is upregulated in mice who prefer alcohol. This gene encodes for a voltage-gated sodium channel. The Hyou gene is downregulated in preferring mice. This gene is involved in the cellular response to stress. The take home here is that there are likely to be thousands of genes that influence our alcohol consumption and it is impossible we will ever identify "THE" alcoholism gene. Nuture Factor impacting Rationale ethanol response Peer and family use A leading influence upon whether or not someone will abuse ethanol is the influences by close friends and family. Sex Males and females have different body-fat composition – different amount of “water space” to hold your ethanol Age Liver has reduced capacity to make metabolic enzymes in the very young and the very old Previous exposure Tolerance to ethanol develops, even cross tolerance to unexpected drugs such as barbiturates develops. Food eaten If there is food in the belly, it dilutes the ethanol, slowing absorption into the blood. Activity Ten: Alcoholism Treatment 13 Ethanol The search for alcoholism treatment options is ongoing. Antabuse (described in activity 8’s TEST OF CONTENT) is an unsavory option. The many side effects overwhelm the benefits for most alcoholics. Quitting “cold turkey” (which means just stopping without treatment or reduction in use, and which was named because [possibly] of a couple of reasons – cold turkey requires little preparation and cold-turkey quitters exhibit cold sweats) is a bad choice because of the elevated risk of death (activity 6). Some newer products are being tried, including antidepressants (reducing the desire to turn to ethanol to selfmedicate depression) and even psychedelic drugs (see Unit 6), which may “startle” the brain out of an addiction cycle. Activity Eleven: Reading Required Reading Liska – Chapter 9: 9.1 – 9.6, and 9.8 – 9.10 and questions 1, 3, 7, 9, 10, 12, 20, 24, 29, and 31. Internet http://rethinkingdrinking.niaaa.nih.gov/WhatCountsDrink/HowMuchIsTooMuch.asp http://health.howstuffworks.com/wellness/drugs-alcohol/alcohol.htm http://learn.genetics.utah.edu/content/addiction/drugs/mouse.html Supplemental Reading Internet http://en.wikipedia.org/wiki/Alcohol_withdrawal_syndrome http://www.cdc.gov/alcohol/faqs.htm http://www.framinghamheartstudy.org/ Science Literature Mulligan, et al., Proc Natl Acad Sci U S A. 2006 April 18; 103(16): 6368–6373. Meta-analysis on genes influencing alcohol abuse. http://pubs.niaaa.nih.gov/publications/arh21-2/144.pdf (paper on neurotransmitters during use and withdrawal) ANY 2010 or 2011 paper by Dr. Susan Tapert from UCSD (search on PubMed). A former UW undergraduate doing prolific and fascinating work in this area (or just read news story on her work http://www.npr.org/templates/story/story.php?storyId=122765890 ). 14