Hospital Standards for Accreditation for Afghanistan
advertisement

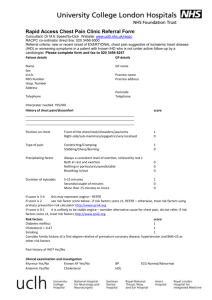
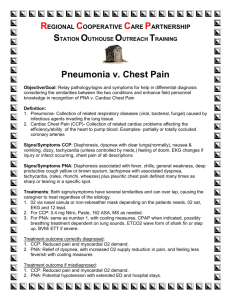
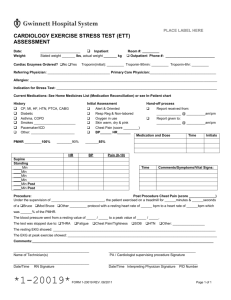
Hospital Standards for Accreditation for Afghanistan Section 2: Clinical Care Emergency Department: Acute Chest Pain Syndromes Hospital Standards for Accreditation for Afghanistan: Assessment of Progress in Achieving the Standards Hospital Department or Area: Emergency Department: Acute Chest Pain Syndromes Hospital Facility: ___________________________________ Assessor: __________________________ Standard Number Standard 1 Recognize that atraumatic chest pain has many causes and many variable presentations Date of Assessment: ________________ Emergency Department: Acute Chest Pain Syndromes Criteria for Verification of Meeting Standard Compliance in Meeting Standard Full Partial None 2 1 0 Clinical Features: - Consider variety of presentations or symptoms of patients with myocardial ischemia - Where is the pain located: retrosternal, epigastric, right or left chest, etc.? - Is there anything that makes the pain change in quality? For example, does the pain change with inspiration, with rest, with supine position, etc.? - When did the pain begin? How long does it last when it occurs? - Are there any other associated symptoms such as nausea, vomiting, diaphoresis, dyspnea, weakness, headache, etc.? - 2 3 Does the pain radiate anywhere? For example, does it radiate to the jaw, neck, arm, abdomen, back? - How is the pain described? Is it throbbing, burning, sharp, stabbing, dull, squeezing, etc.? - Does the patient have any coronary risk factors such as hypertension, known coronary artery disease, tobacco use, high cholesterol, obesity, diabetes mellitus? Is the patient male? Is there a family history of heart disease? Recognizes that - How does the patient look? physical examination - What are the vital signs? Is the patient may vary in patients tachycardic, dyspneic, febrile, with chest pain hyper/hypotensive, hypoxic? - Do you note rales, wheezing, rhonchi? - Is there a murmur present? - Is there any chest wall tenderness? Rapid, quick EKG: the ekg is quite clinically reliable and assessment is diagnostic in patients with acute infarctions performed and early - Is an EKG completed within 10 treatment is initiated Minutes of a patient presenting to the ED? - Recognize that a normal ekg does not rule out cardiac ischemia - Are there ST elevations, Q waves, T wave inversions, new bundle branch blocks which suggest ischemia? Serum Markers: If available, serum markers are very specific for acute myocardial infarction (AMI). - A CK, CK-MB and troponin were obtained shortly after patient arrival. - Serial enzymes were evaluated because these markers do not rise immediately. - Time of symptom onset is known to allow the physician to evaluate cardiac enzyme results. - Is aware that CK generally rises within 4-8 hours of an AMI and remains elevated for several days. CK-MB which is more specific to myocardium typically rises within 2-6 hours of an AMI and returns to normal within 1224 hours. Troponin is even more specific and rises within 4-6 hours of an AMI and remains elevated for up to 10 days. Echocardiogram: May be helpful in evaluating a patient with a normal ekg. - Notes wall motion abnormalities are suggestive of acute or previous myocardial injury. - Realizes that echocardiogram examination may assist in diagnosing pericarditis, aortic dissection and other acute chest pain processes. Oxygen/Monitoring/IVs: - Any patient suspected of having acute cardiac pain is placed on continuous cardiac monitoring, has an IV placed and receives supplemental oxygen. Aspirin: - Aspirin 325 mg is given to any patient suspected of having acute ischemia unless there are contraindications. 4 Considers causes of chest pain and is aware of their presentations and immediate treatment. Angina Pectoris: - Is aware that this is often described as squeezing or aching and usually lasts less than 15 minutes. - Realizes that this is usually episodic in nature, relieved by rest or sublingual (SL) nitroglycerin (ntg). NTG typically relieves anginal pain in less than 3 minutes. - Understands the difference between stable and unstable angina. Unstable angina is much more concerning due to increased risk of sudden cardiac death. Acute Myocardial Infarction/Acute Coronary Syndromes: Is aware that: - Pain may not be relieved by ntg. - May be accompanied by nausea, vomiting, diaphoresis, radiation to jaw or arm - Patients with diabetes mellitus, the elderly, women and others may present with very atypical symptoms. Performs the following: - Ensures patient placed on monitor, receives O2 and an IV. Obtains an ekg within 10 minutes of arrival. - Gives the patient 325 mg aspirin to chew (unless contraindications). - Obtains a complete set of vital signs immediately. - Gives SL Ntg if considering AMI, angina or ischemia. - Is aware that Ntg may cause headache in patients. Is aware that Ntg may decrease blood pressure and is prepared to counteract this. - Understands that Ntg is contraindicated in patients with Right Ventricular (RV) infarction. - Considers the use of IV beta blocker to treat MI, hypertension, recurrent ischemia, tachycardic rhythms, etc. - Understands contraindications to beta blockade: asthma, bradycardia, hypotension, severe CHF, COPD, severe peripheral vascular disease. - Considers pain treatment with IV morphine. Understands that this may worsen hypotension. - - - Considers heparin therapy. Considers fibrinolytics as appropriate. Understands fibrinolytic relative and absolute contraindications. Recognizes RV infarcts and the need for intravascular volume/elevated RV filling pressures. Admits patients with unstable angina, acute myocardial infarction and continues treatment and cardiac monitoring. Aortic Dissection: - Considers in any patient who presents with acute onset, severe, tearing or ripping pain that is retrosternal and/or radiates to the back. The pain is usually maximal at onset. - Recognizes that nausea, vomiting and Diaphoresis may also be present. - Obtains immediate vital signs, including blood pressures in all four extremities. - Obtains an immediate chest xray and/or CT scan if the patient is hemodynamically stable. - Immediately stabilizes the patient, obtains large-bore IV access. - Obtains abo/rh and cross match. - Manages hypertension appropriately with beta blockers IV or calcium - - channel blockers (2nd line). Titrates to pain relief and systolic blood pressure of 100-120 mm Hg. Understands the classification of aortic dissections and the treatments of each. - Stanford A: involves ascending aorta and is typically treated surgically. - Stanford B: involves descending aorta and is most often medically managed. Places appropriate consults to cardiology, vascular or thoracic surgery. Pericarditis: Acute pericarditis may be difficult to distinguish from other causes of chest pain. - Recognizes that pain may be acute or gradual in onset. It may radiate to the back, left arm, neck or jaw. - Is aware that symptoms may be increased when supine and relieved when leaning forward. - Recognizes a friction rub heard at the left lower sternal border or apex as indicative of pericarditis. - Knows that pericarditis may be associated with fever and dyspnea. - Can name etiologies of pericarditis including viral, autoimmune, bacterial, fungal, malignancy, drugs, radiation, - - - uremia, myxedema, idiopathic, etc. Orders an ekg immediately and recognizes changes that may occur with acute pericarditis, including: diffuse ST segment elevation early (this may resolve), diffuse T wave inversion, PR depression in inferolateral leads, etc. Obtains a chest xray to rule out other causes of pain. If available, obtains an echocardiogram. If the diagnosis is pericarditis and the patient is stable, treats with nonsteroidal anti-inflammatory. Admits patients with pericarditis of presumed uremic origin or any patient who is unstable. Pericardial Tamponade: May be traumatic or nontraumatic in origin. - Immediately places patient on monitor, Oxygen, IV. - Immediately obtains ekg. - Recognizes etiologies as trauma, malignancy, idiopathic, bacterial, uremia, chronic pericarditis, TB, collagen vascular diseases, etc. - Notes symptoms consistent with Tamponade, including dyspnea, positional or pleuritic chest pain. - Is aware of physical examination Findings such as tachycardia, JVD, - - - hypotension, muffled heart sounds, etc. Recognizes pulsus paradoxus (on Inspiration 10 mm Hg decrease in SBP) as a sign of tamponade or constrictive pericarditis. Recognizes electrical alternans (beat to beat variability of QRS amplitude) as an indicator of tamponade. Performs immediate pericardiocentesis if patient is critically unstable. Prior to pericardiocentesis, gives 1 L Crystalloid fluid bolus to improve right heart filling (if time permits). Pulmonary Embolism: A high index of suspicion must be used for this diagnosis given its nonspecific symptoms and variable presentation. - Immediately obtains EKG. - Immediately places patient on monitor, IV, O2. Begins IV crystalloid fluid infusion to correct hypotension. - Recognizes that symptoms may include dyspnea, chest pain, tachycardia, hypoxia, syncope, tachypnea, etc. - Recognizes potential causes as malignancy, hypercoagulable states, venous stasis (trauma, post-operative, sedentary/paralytic), pregnancy, etc. - Immediately obtains chest xray to rule out other causes of chest pain. - - - - Orders blood tests including cbc, electrolytes, coagulation studies, creatinine, cardiac enzymes (if available). If available, orders CT scan of the chest to further evaluate for PE size and distribution. Begins anticoagulation therapy. This may be heparin or low molecular weight heparin as available. If hemodynamically unstable, considers treatment with thrombolytics. Recognizes other causes of acute chest pain and potential presentations as noted in attachment (1). These include pulmonary, musculoskeletal and gastrointestinal causes. DIFFERENTIAL DIAGNOSIS OF CHEST PAIN AMI Pericarditis Angina CHF Aortic Dissection Severe, nausea/vomiting, shortness of breath, diaphoresis, Radiation to jaw or arm, Lasts more than 15 minutes Positional pain, dyspnea, Symptoms relieved by sitting forward Associated with exertion or change in stable angina Dyspnea, Paroxysmal nocturnal dyspnea, Orthopnea, Peripheral Edema, JVD Maximal at onset, ripping, radiates to back May have altered mental status/loc Pulmonary Edema Bronchitis COPD Pulmonary Embolism Pneumonia Dyspnea, Tachycardia, Exertional symptoms, Paroxysmal Nocturnal Dyspnea Cough, dyspnea, +/- Fever Chronic cough, dyspnea Acute onset, dyspnea, pleuritic pain, tachycardia Fever, Cough, Dyspnea, Chills Gastritis Esophagitis Esophageal Rupture Splenic Rupture PUD Burning, often worse after eating Burning, often worse after eating, may have dysphagia Retrosternal or epigastric pain after vomiting/trauma TTP, hypotension, tachycardia, Kehr sign Abdominal pain, burning, +/- hematemesis, melena Cholecystitis Cholangitis Pancreatitis RUQ or R chest pain, often follows fatty meal, nausea/vomiting RUQ pain, nausea/vomiting, fever RUQ or midabdominal pain, nausea/vomiting Costochondritis Trauma Not always inciting event; tender to palpation, symptoms increase with movement YOU MUST ASK: History: Onset of symptoms; description Pain: where, what, radiation Other six: diaphoresis, dizziness, syncope, fever, cough, shortness of breath Past Medical History: COPD, Trauma, DM, Hypertension, CHF, Hyperlipidemia Family History: AMI (age, sex), Medications: