Girdlestone
advertisement
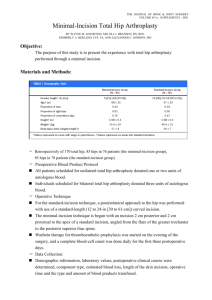
Complications Associated with Reimplantation After Girdlestone Arthroplasty CORR No. 407, pp. 119-126, Feb. 2003, William P.H. Charlton et al. Rothman Institute Orthopaedics, Thomas Jefferson University, Philadelphia, PA Objective: To report the complications and results of reimplantation total hip arthroplasty for patients treated with resection arthroplasty for hip infection. Materials and Method: *Till Nov. of 1997, 101 hips (100 patients) have received op. for infected hip prosthesis. *58 hips (57 patients) have had a two-stage exchange protocol, 6 pt’s (7 hips) died of unrelated causes, incomplete FU in 7 cases. *44 hips in 44 patients with mininum 2-year followup (range, 2-9 years), 22 men and 22 women, mean age : 63 (32-85). *Average 3.5 operations before resectional arthroplasty. 7: prior surgery for a prosthetic hip infection; 14: infected primary THA; 12: infected revision THA; 8: previous infected hardware; 3: previous infected hemiarthroplasty. *38 positive cultures from preoperative aspirates or surgical tissue specimens. All had documentation of the isolotaion of causal organisms at another institution. *All reimplantations were preceded by a resection arthroplasty: removal of all hardware and cement, extensive debridement, irrigation, and limited bone resection. *Cement spacers consisting of antibiotic impregnated PMMA were used in 30 hips (Tobramycin in 26 hips, Tobramycin and Vancomycin in 4 hips, 1.2g/vial of mement). *A 6-week course of parenteral antibiotic treatment based on the sensitivity tests. *Reimplantation:.3 months (14weeks – 22 months), one surgeon, cancellous allograft used in all hips, 11 bulk femoral allograft, 3 cortical only strut allograft. 37 uncemented femoral components, 35 uncemented acetabular components. *FU (pre-op., 6 months post-op. and then yearly): Charnley’s modified D’Aubigne and Postel scale (1~6 ) for pain, function and motion; Harris hip scoring system, and radiographic evaluation for loosening. Results: *Charnley’s modified scale Pre-op. Post-op. Pain 3.2 5.2 Function 2.8 4.3 ROM 4.6 5.1 40 78 Harris Hip Score *Two patients required subsequent revision: one for recurrent infection, one for recurrent dislocation *LLD: Pre-op. Post-op. 30.5mm (3-100mm) 6.5mm (5-30mm, 50% normal) *Limping: 39%, 12% severe. *Functional evaluation: 45% could walk at least 6 blocks, 43% could put on shoes, 73% could climb stairs, 68% could sit in any chair for 1 hour, and 57% could take public transportation. *Radiographic analysis: Acetabulum Cemented Cementless 0 loosen (7) all stable (37) 1 osteolysis (found at 2 yrs, stable at 6 yrs) Femur 0 loosen (7) 36 stable (37) 1 loosen (no symptom) *Complications Nonprosthesis-related: CHF (2), diarrhea (2), angina (1), arrhythmia (1), transfusion reaction (1), urinary retention (1), UTI (1). Prosthesis-related: postoperative wound drainage (1), hematoma (1), trochanteric nonunion (4), heterotopic ossification (1), early and late dislocation (5), recurrent infection (1). Conclusion: in Deep Infected THA *Resectional arthroplasty: LLD of 3-6cm, need walking aids, inadequate pain relief. *Current study: Successful rate 97.6% (1 stage: 38.5% ~ 90%, 2 stage: 60% ~ 100%.) Nonprosthetic–related complications: 23% Local complications: 33% Dislocation: 11.4% (3.8~18%) Persistent limping: 39% 2003/06/16