Title: There are still no adequate studies
advertisement
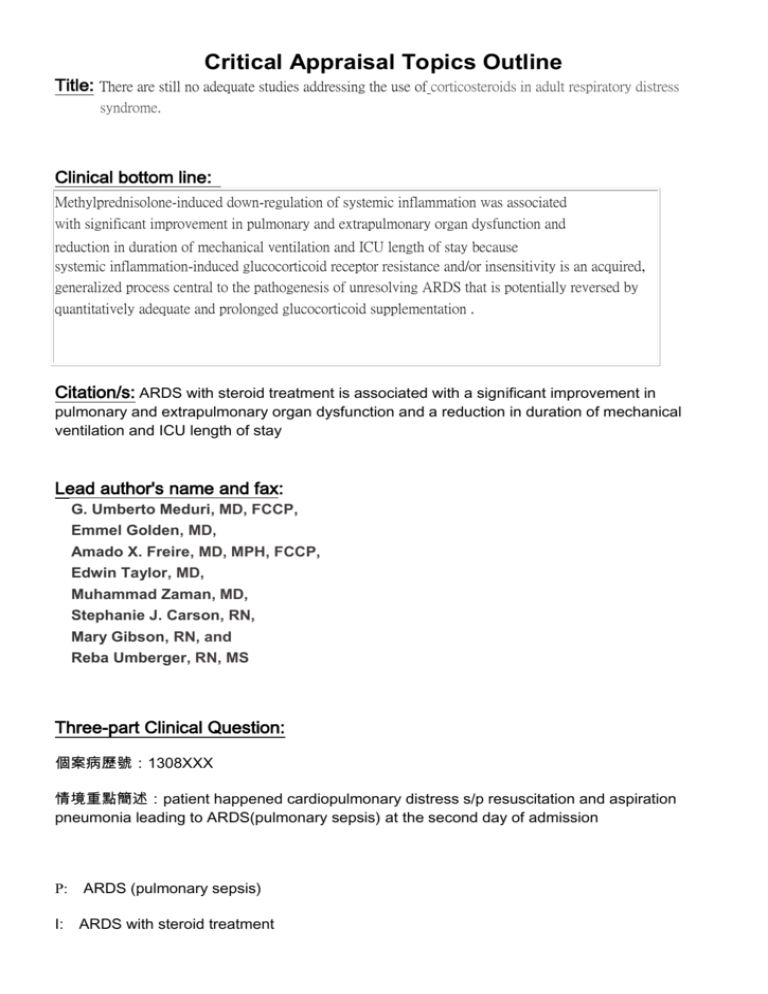
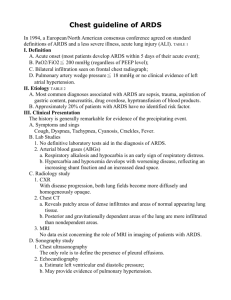
Critical Appraisal Topics Outline Title: There are still no adequate studies addressing the use of corticosteroids in adult respiratory distress syndrome. Clinical bottom line: Methylprednisolone-induced down-regulation of systemic inflammation was associated with significant improvement in pulmonary and extrapulmonary organ dysfunction and reduction in duration of mechanical ventilation and ICU length of stay because systemic inflammation-induced glucocorticoid receptor resistance and/or insensitivity is an acquired, generalized process central to the pathogenesis of unresolving ARDS that is potentially reversed by quantitatively adequate and prolonged glucocorticoid supplementation . Citation/s: ARDS with steroid treatment is associated with a significant improvement in pulmonary and extrapulmonary organ dysfunction and a reduction in duration of mechanical ventilation and ICU length of stay Lead author's name and fax: G. Umberto Meduri, MD, FCCP, Emmel Golden, MD, Amado X. Freire, MD, MPH, FCCP, Edwin Taylor, MD, Muhammad Zaman, MD, Stephanie J. Carson, RN, Mary Gibson, RN, and Reba Umberger, RN, MS Three-part Clinical Question: 個案病歷號:1308XXX 情境重點簡述:patient happened cardiopulmonary distress s/p resuscitation and aspiration pneumonia leading to ARDS(pulmonary sepsis) at the second day of admission P: ARDS (pulmonary sepsis) I: ARDS with steroid treatment C: ARDS without steroid treatment O: mortality Type of question: Intervention Search Terms & Strategy: Database: Pubmed Key words & Search strategy: ARDS(acute respiratory distress syndrome) and corticosteroid and mortality 1. 2. 3. 4. Pub med MeSH ARDS(acute respiratory distress syndrome)narrow search #1 Pub med MeSH corticosteroidnarrow search #5 Pub med MeSH mortality narrow search #7 #1 and #5 and #7- advanced searchMethylprednisolone infusion in early severe ARDS: results of a randomized controlled trial.Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, Gibson M, Umberger R.Chest. 2007 Apr;131(4):954-63.PMID: 17426195 [PubMed - indexed for MEDLINE]Related articlesFree article The Study: Type: Randomized, double-blind, placebo-controlled trial (A Randomized, double-blind, placebo-controlled trial was performed to determine the effects of low-dose prolonged methylprednisolone infusion on lung function in patients with early severe ARDS. Ninety-one patients with severe early ARDS (≤ 72 h), 66% with sepsis. Patients were randomized (2:1 fashion) to methylprednisolone infusion (1 mg/kg/d) vs placebo. The duration of treatment was up to 28 days. Results: Treated patients had significant reduction in C-reactive protein levels, and by day 7 had lower LIS and multiple organ dysfunction syndrome scores. Treatment was associated with a reduction in the duration of mechanical ventilation, ICU stay, ICU mortality and lower rate of infections. ) Level of Evidence: 1b The Evidence: 1. Compared with placebo, steroids were associated with significant improvement in pulmonary and extrapulmonary organ dysfunction and reduction in duration of mechanical ventilation and ICU length of stay. 2. Treatment with methylprednisolone significantly reduced mortality of ARDS. Comments: Methylprednisolone-induced down-regulation of systemic inflammation in ARDS was associated with significant improvement in pulmonary and extrapulmonary organ dysfunction and reduction in duration of mechanical ventilation and ICU length of stay. No bias because patients were selected with randomized fashion (2:1 fashion) of ARDS patients 1. The choice of therapy for ARDS remains a controversial area, but in our opinion adjunctive therapy with corticosteroids should only be considered in patients with sustained ARDS with severe sepsis and ventilator support patients. 2. The efficacy of corticosteroids has not been adequately evaluated by RCT in the context of such a ‘standard regimen’. 3. The renoprotective efficacy of the ‘standard regimen’ means that evaluation of any additional intervention will require increasingly large and prolonged RCTs to prove benefit for additional agents unless robust surrogate measures of outcome are developed to enable studies to be scaled down without loss of power. Information from well-designed RCTs remains a pressing priority if uncertainties in the treatment of corticosteroids are to be resolved. In intention-to-treat analysis, the response of the two groups (63 treated and 28 control) clearly diverged by day 7, with twice the proportion of treated patients achieving a 1-point reduction in LIS (69.8% vs 35.7%; p _ 0.002) and breathing without assistance (53.9% vs 25.0%; p _ 0.01). Treated patients had significant reduction in C-reactive protein levels, and by day 7 had lower LIS and multiple organ dysfunction syndrome scores. Treatment was associated with a reduction in the duration of mechanical ventilation (p _ 0.002), ICU stay (p _ 0.007), and ICU mortality (20.6% vs 42.9%; p _ 0.03). Treated patients had a lower rate of infections (p _ 0.0002), and infection surveillance identified 56% of nosocomial infections in patients without fever. Conclusions: Methylprednisolone-induced down-regulation of systemic inflammation was associated with significant improvement in pulmonary and extrapulmonary organ dysfunction and reduction in duration of mechanical ventilation and ICU length of stay. References: 1. Meduri, GU, Yates, CR Systemic inflammation-associated glucocorticoid resistance and outcome of ARDS. Ann N Y Acad Sci 2004;1024,24-53 2. Parsons, PE, Eisner, MD, Thompson, BT, et al Lower tidal volume ventilation and plasma cytokine markers of inflammation in patients with acute lung injury. Crit Care Med 2005;33,1-6 3. Annane, D, Sebille, V, Bellissant, E Effect of low doses of corticosteroids in septic shock patients with or without early acute respiratory distress syndrome. Crit Care Med 2006;34,22-30 Kill or Update By: 科部會議名稱 舉行日期時間 報告者: 姓名 指導臨床教師 : 彰化基督教醫院腎臟內科 EMB 個案報告會議 : 99 / 01 / 05 , 0730-0830 : 謝浩明 Code :141930 Email :141930@cch.org.tw : 邱炳芳醫師