A New Assay for "True" Bio-Intact Parathyroid Hormone
advertisement

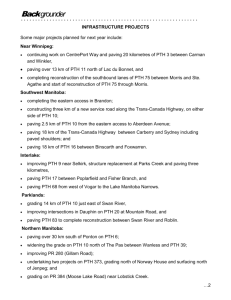
Administrative Office St. Joseph's Hospital Site, L301-10 50 Charlton Avenue East HAMILTON, Ontario, CANADA L8N 4A6 PHONE: (905) 521-6141 FAX: (905) 521-6142 http://www.fhs.mcmaster.ca/hrlmp/ Issue No. 75 QUARTERLY NEWSLETTER June 2004 A New Assay for "True" Bio-Intact Parathyroid Hormone Parathyroid hormone (PTH) is an 84 amino acid polypeptide produced by the parathyroid glands that influences calcium and phosphate homeostasis by its action on target organs, bone and kidney. In bone, it mobilizes calcium and phosphate thus raising serum calcium concentration. In the kidney, calcium is conserved by increasing renal tubular reabsorption, and excretion of phosphate in the urine is increased by inhibition of tubular reabsorption. PTH also stimulates renal hydroxylation of 25-(OH) vitamin D to 1,25 (OH)2 vitamin D which, in turn, enhances intestinal calcium absorption. PTH secretion is regulated by free calcium concentrations in the blood through a negative feedback mechanism. A fall in serum calcium concentration stimulates PTH secretion, whereas a rise in serum calcium produces an opposite effect. The measurement of serum PTH levels is crucial in the assessment of calcium metabolism disorders. In combination with calcium levels, determination of PTH is useful in the differential diagnosis of primary and secondary hyperparathyroidism, hypoparathyroidism; vitamin D deficiency, and hypercalcemia of malignancy; and particularly in diagnosis and management of patients with renal osteodystrophy. This is a complex disorder of bone that is commonly encountered in patients with chronic renal failure. These patients develop hypocalcemia that stimulates PTH secretion and causes secondary hyperparathyroidism and increased bone turnover leading to the development of renal osteodystrophy. Controlling hyperparathyroidism by suppressing PTH secretion is the key to treating renal osteodystrophy. Monitoring the decrease in serum PTH is important to avoid oversuppression of the parathyroid glands. Human blood contains both intact PTH (1-84) and several PTH fragments. Intact PTH has a half-life in the blood of only 3-4 minutes. It is rapidly degraded either within the parathyroid glands or in the peripheral tissues (liver and kidney) to yield N- and C- terminal PTH fragments. The small N-terminal fragment (134) is a full PTH agonist, which is rapidly cleared from the circulation and is usually undetectable. The large C-terminal fragment, also known as N-terminal truncated fragment, has a relatively long half-life of a few hours and is removed from the circulation primarily by glomerular filtration. Therefore, intact PTH (184) and N-terminal truncated fragments are the principal circulating forms of PTH. N-terminal truncated fragments have been traditionally thought to lack biological activity. Recent evidence shows that they may act as PTH antagonists. The major biological effects of PTH are through the activation of the PTH receptor, and activation requires the N-terminal portion of PTH (1-84) and PTH (1-34). This effect is eliminated when the N-terminal serine residue is truncated (7-84). The ratio of fragments to intact PTH is very variable and largely depends on renal function. N-terminal truncated fragments represent approximately 1-20% of circulating PTH in healthy individuals and in primary hyperparathyroidism. This ratio may increase to 35% or more in end-stage renal failure due to decreased clearance of PTH fragments. Blood calcium concentrations also influence the proportion of PTH fragments. When blood calcium concentrations rise, relatively greater amounts of N-terminal truncated fragments and lesser amounts of intact PTH are detected in the plasma. In contrast, more intact PTH and less C-terminal fragments are found when blood calcium concentrations are reduced. Initially, PTH was measured using radioimmunoassay (RIA) with a single antibody directed against the more immunogenic C-terminal region of PTH. The heterogeneous nature of circulating PTH made these assays nonspecific and unreliable especially in kidney disease where clearance may be compromised. The specificity has been improved with the introduction of two-site immunoradiometric assays (IRMA) for intact PTH. The principle of these assays is to detect intact PTH using two distinct antibodies, one is a solid phase capture antibody directed against the C-terminal region of PTH, and one is a radiolabeled detection antibody directed against the N-terminal region of the PTH peptide. A major drawback of these assays is that they not only detect intact PTH (1-84), but also cross react with large N-terminal truncated PTH fragments (7-84). As N-terminal truncated PTH fragments may inhibit PTH activity, simultaneous measurement of intact PTH and its potential inhibitor not only overestimates PTH levels, but also makes it difficult to interpret PTH measurements. This is particularly true in chronic renal failure where these large fragments may accumulate in the blood and have implications in the management of secondary hyperparathyroidism in these patients. The Bio-Intact PTH assay, a two-site immunochemiluminometric assay recently developed for measurement of “true” intact PTH (1-84) was introduced in our laboratory and is provided by the HRLMP. The major advantage of this assay over the first-generation IRMA test is to specifically measure intact PTH (1-84) in human serum or plasma, and not PTH fragments (7-84). The specificity of this assay is achieved by using a detection antibody directed toward the first six amino acids at the N-terminal end. PTH fragments lacking one or several amino acid residues at N-terminal region will not be detected. Recently, we have completed the method validation of this new Bio-Intact PTH assay and our results support clinical application of this assay for detection of PTH. The reference value for this assay is 6 - 40 pg/mL. 1) Inaba M, Nakatsuka K, Imanishi Y, Watanabe M, Mamiya Y, Ishimura E and Nishizawa Y. Technical and clinical characterization of the Bio-PTH (1-84) immunochemiluminometric assay and comparison with a second-generation assay for parathyroid hormone. Clin Chem 2004;50:385-390. 2) Goodman WG, Juppner H, Salusky IB, Sherrard, DJ.Parathyroid hormone (PTH), PTH-derived peptides, and new PTH assays in renal osteodystrophy. Kidney Int. 2003 Jan;63:1-11. Dr. Liju Yang, Post-Doctoral Fellow Dr. Vijay Grey, McMaster University Medical Centre Dr. Gillian Luxton. St Joseph Healthcare Discipline of Clinical Chemistry Hamilton Regional Laboratory Medicine Program