Diagnosis and treatment of Fabry nephropathy, with clinical practice
advertisement
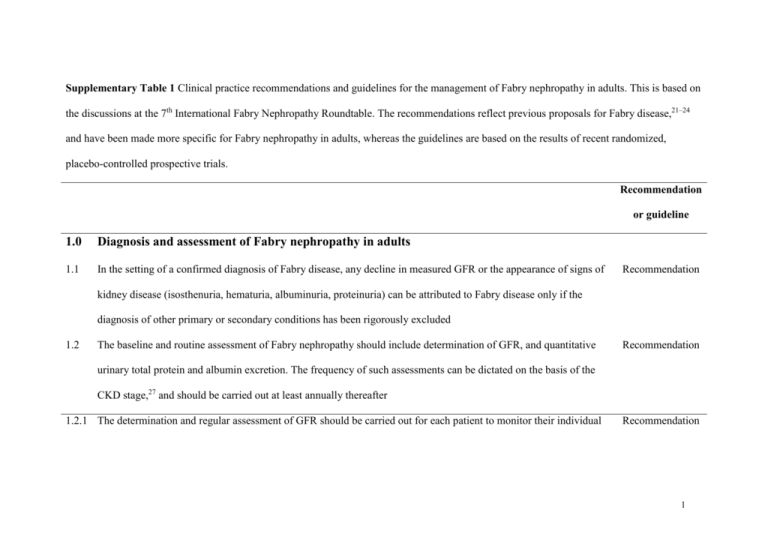
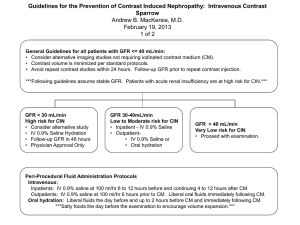
Supplementary Table 1 Clinical practice recommendations and guidelines for the management of Fabry nephropathy in adults. This is based on the discussions at the 7th International Fabry Nephropathy Roundtable. The recommendations reflect previous proposals for Fabry disease,21–24 and have been made more specific for Fabry nephropathy in adults, whereas the guidelines are based on the results of recent randomized, placebo-controlled prospective trials. Recommendation or guideline 1.0 Diagnosis and assessment of Fabry nephropathy in adults 1.1 In the setting of a confirmed diagnosis of Fabry disease, any decline in measured GFR or the appearance of signs of Recommendation kidney disease (isosthenuria, hematuria, albuminuria, proteinuria) can be attributed to Fabry disease only if the diagnosis of other primary or secondary conditions has been rigorously excluded 1.2 The baseline and routine assessment of Fabry nephropathy should include determination of GFR, and quantitative Recommendation urinary total protein and albumin excretion. The frequency of such assessments can be dictated on the basis of the CKD stage,27 and should be carried out at least annually thereafter 1.2.1 The determination and regular assessment of GFR should be carried out for each patient to monitor their individual Recommendation 1 Recommendation or guideline progression (ml/min/1.73 m2/year) 1.2.2 The estimation of GFR from serum creatinine lacks sufficient precision when the baseline GFR exceeds 60 Recommendation ml/min/1.73 m2, and other methods can be considered (e.g. inulin, iohexol, 51Cr-EDTA)8,28 1.3 Kidney biopsy is necessary to define Fabry nephropathy, and exclude other primary or secondary conditions. Recommendation Significant lesions have been described early in the course of Fabry nephropathy before there are overt clinical signs of kidney involvement.17,51 Kidney biopsy is an important tool for diagnosing, staging, and assessing the response to therapies in Fabry disease 2.0 Management of Fabry nephropathy in adults (Figure 6) 2.1 The current guidelines for the management of CKD should be applied to the diagnosis and management of Fabry Recommendation nephropathy27 2.2 In the opinion of the Roundtable, there is a compelling indication for the use of ACE inhibitors and/or ARBs in Recommendation patients with Fabry nephropathy who have proteinuria >500 mg/day. As recommended in other forms of CKD, the 2 Recommendation or guideline systolic pressure should be titrated below 130 mm Hg if the urine protein excretion exceeds 500 mg/day2,11,48,27 2.2.1 Double-blind, placebo-controlled trials with agalsidase alfa or agalsidase beta,8,37,38 as well as open-label, Guideline observational studies,10,40,52,58 have shown that ERT alone does not reduce urine protein excretion or slow the progressive decline in GFR in patients who have advanced Fabry nephropathy (estimated GFR <60 ml/min/1.73 m2, urine protein excretion >1 g/24 hours, or >50% glomerular sclerosis score) 2.2.2 ERT appears to stabilize GFR in mild to moderate Fabry nephropathy (baseline GFR >60 ml/min/1.73 m2, urine Guideline protein <500 mg/day, or < 50% glomerular sclerosis score)8,9,37,58 2.2.3 Initiation of anti-proteinuric therapy in patients with overt proteinuria in the absence of appropriate ERT is not Recommendation supported by any weight of evidence. The use of anti-proteinuric therapy for patients with minimal urinary albumin excretion to forestall the development of overt Fabry nephropathy, and avoid the initiation of ERT is not supported by any weight of evidence 2.3 In accord with the UK Guidelines,23 the following signs of Fabry nephropathy are compelling indications for the Recommendation institution of effective ERT in Fabry disease: significantly reduced GFR (<80 ml/min/1.73 m2); proteinuria >300 3 Recommendation or guideline mg/24 hours, or albuminuria >30 mg/24 hours when a kidney biopsy demonstrates endothelial deposits in glomerular capillaries 2.4 The management of Fabry nephropathy should be the same for males and females, recognizing that females usually Recommendation develop severe Fabry nephropathy at a later age than males4,17 2.5 Kidney transplant is an effective treatment for Fabry nephropathy,53 but does not address the other organ systems Recommendation involvement in Fabry disease. There are benefits of initiating ERT even after kidney transplantation, but more detailed prospective evaluations are needed.54 Likewise, providing ERT to Fabry patients who are already transplanted or on dialysis may forestall cardiac or cerebrovascular events, but definitive outcome studies are not yet available. 4