guidelines for writing a winning abstract
advertisement
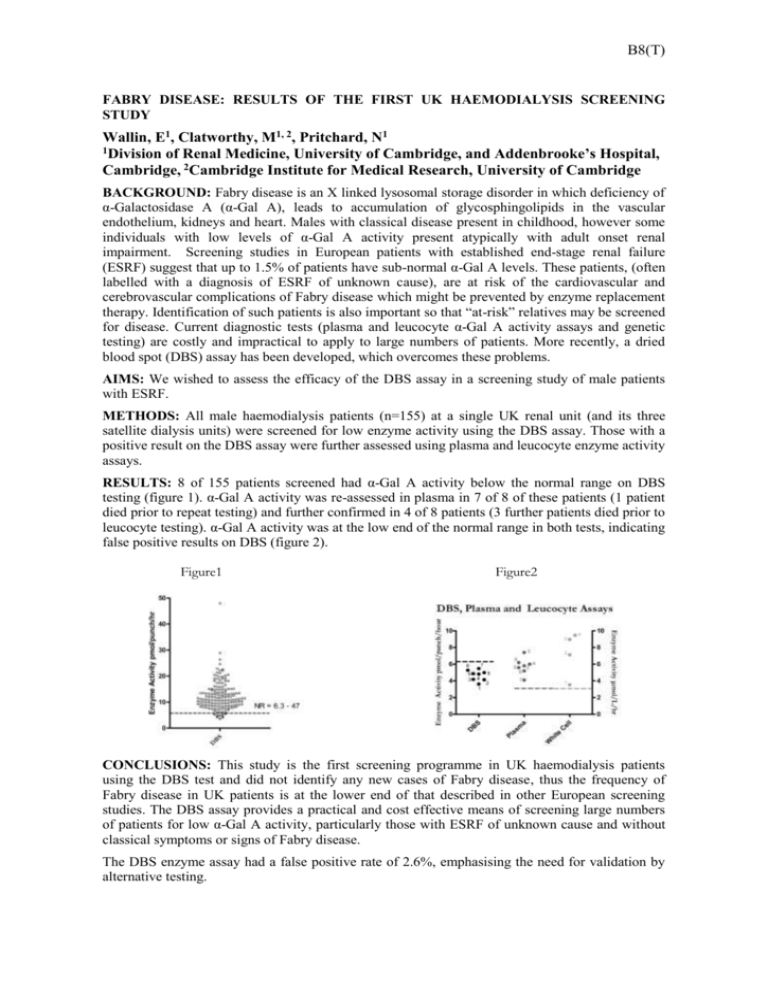
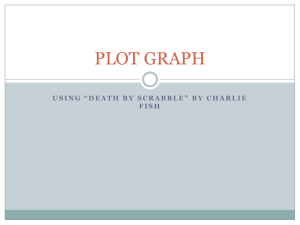
B8(T) FABRY DISEASE: RESULTS OF THE FIRST UK HAEMODIALYSIS SCREENING STUDY Wallin, E1, Clatworthy, M1, 2, Pritchard, N1 1Division of Renal Medicine, University of Cambridge, and Addenbrooke’s Hospital, Cambridge, 2Cambridge Institute for Medical Research, University of Cambridge BACKGROUND: Fabry disease is an X linked lysosomal storage disorder in which deficiency of α-Galactosidase A (α-Gal A), leads to accumulation of glycosphingolipids in the vascular endothelium, kidneys and heart. Males with classical disease present in childhood, however some individuals with low levels of α-Gal A activity present atypically with adult onset renal impairment. Screening studies in European patients with established end-stage renal failure (ESRF) suggest that up to 1.5% of patients have sub-normal α-Gal A levels. These patients, (often labelled with a diagnosis of ESRF of unknown cause), are at risk of the cardiovascular and cerebrovascular complications of Fabry disease which might be prevented by enzyme replacement therapy. Identification of such patients is also important so that “at-risk” relatives may be screened for disease. Current diagnostic tests (plasma and leucocyte α-Gal A activity assays and genetic testing) are costly and impractical to apply to large numbers of patients. More recently, a dried blood spot (DBS) assay has been developed, which overcomes these problems. AIMS: We wished to assess the efficacy of the DBS assay in a screening study of male patients with ESRF. METHODS: All male haemodialysis patients (n=155) at a single UK renal unit (and its three satellite dialysis units) were screened for low enzyme activity using the DBS assay. Those with a positive result on the DBS assay were further assessed using plasma and leucocyte enzyme activity assays. RESULTS: 8 of 155 patients screened had α-Gal A activity below the normal range on DBS testing (figure 1). α-Gal A activity was re-assessed in plasma in 7 of 8 of these patients (1 patient died prior to repeat testing) and further confirmed in 4 of 8 patients (3 further patients died prior to leucocyte testing). α-Gal A activity was at the low end of the normal range in both tests, indicating false positive results on DBS (figure 2). Figure1 Figure2 CONCLUSIONS: This study is the first screening programme in UK haemodialysis patients using the DBS test and did not identify any new cases of Fabry disease, thus the frequency of Fabry disease in UK patients is at the lower end of that described in other European screening studies. The DBS assay provides a practical and cost effective means of screening large numbers of patients for low α-Gal A activity, particularly those with ESRF of unknown cause and without classical symptoms or signs of Fabry disease. The DBS enzyme assay had a false positive rate of 2.6%, emphasising the need for validation by alternative testing.




![[Date] - Fabrazyme](http://s3.studylib.net/store/data/007856986_2-92736280fd31154fb73068d0df9b074f-300x300.png)
