Shenandoah University Division of Physical Therapy
advertisement

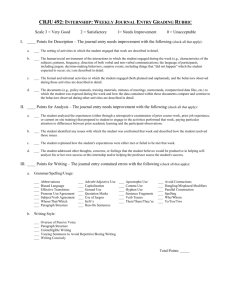
Shenandoah University Division of Physical Therapy Course Name: Clinical Internship 2 – Spring 3rd Year Clinical Internship 3 – SpringSummer 3rd Year Course Number: Credit: Hours: Semester: Faculty: PT 854 and PT 855 6 Credits 13 weeks, full time Spring and Summer, 3rd year Dr. Missy Wolff-Burke - course coordinator Course Description The purpose of each learning experience is to progress the PT student to the level of an entry-level clinician at the completion of EACH clinical internship. The amount of assistance required by the clinical instructor will gradually decrease as the student progresses within each Clinical Internship. These experiences are geared toward expanding clinical problem solving and demonstrating the critical thinking and patient management skills of an entry-level Physical Therapist. New concepts and skills specific to the clinical experience will be incorporated. The three Clinical Internship experiences should be varied between IP, OP, Rehab, Pediatrics and other clinical experiences as clinical contracts allow. An in-service (or service-in-kind) is required in each setting. Under the direct supervision of a practicing physical therapist, the experience is designed to allow the student “hands-on” learning. Adherence to and a progression of behaviors as identified in the PT-Specific Generic Abilities (updated to Professional Behaviors) and Core Values are expected. Direct Supervision: The physical therapist is physically present and immediately available for direction and supervision. The physical therapist will have direct contact with the patient during each visit. Telecommunications does not meet the requirements of direct supervision. (Definitions from the 2000 APTA House of Delegates, Position Levels of Supervision, RC-25-00. Levels of supervision ) These definitions do NOT supersede the regulations of a facility or state.) Required Texts None. Students should avail themselves of their textbooks, and other educational material as needed to be effective and to advance their own learning during the clinical experience. Course Objectives Clinical Internship 2 and 3 (PT 854, 855): At the completion of each full-time clinical experience, the student will have progressed to entry-level clinical performance, (interval 5) on the CPI Web, with comments that support that interval. The student will be evaluated on all 18 clinical performance criteria: Professional Practice 1. Safety 2. Professional Behavior 3. Accountability 4. Communication 5. Cultural Competence 6. Professional Development Patient Management 7. Clinical Reasoning 8. Screening 9. Examination 10. Evaluation 11. Diagnosis and Prognosis 12. Plan of Care 13. 14. 15. 16. 17. 18. Procedural Interventions Educational Interventions Documentation Outcomes Assessment Financial Resources Direction and Supervision of Personnel Professional Behavior: Professional Behaviors and The Core Values have been adopted by the Shenandoah University Division of Physical Therapy faculty as essential components of the program and considered necessary for successful fulfillment of the requirements of the program. The process of becoming an effective physical therapist involves attaining competency in cognitive knowledge, psychomotor skills and professional behavior. Each aspect of this triad is equally important for the student to develop as s/he progresses through the Physical Therapy Program. The items define the professional behavior expected of Shenandoah University Division of Physical Therapy students. Appropriate levels of behavior are expected in all courses. To facilitate development of competency in the professional behaviors, the instructors will provide, when necessary, opportunities to practice, and provide formal and informal feedback to the student throughout the semester. The student will be responsible for ongoing self-assessment and for seeking feedback from faculty and fellow students. Professional Behaviors 1. Critical Thinking - The ability to question logically; identify, generate and evaluate elements of logical argument; recognize and differentiate facts, appropriate or faulty inferences, and assumptions; and distinguish relevant from irrelevant information. The ability to appropriately utilize, analyze, and critically evaluate scientific evidence to develop a logical argument, and to identify and determine the impact of bias on the decision making process. 2. Communication - The ability to communicate effectively (i.e. verbal, nonverbal, reading, writing, and listening) for varied audiences and purposes. 3. Problem Solving – The ability to recognize and define problems, analyze data, develop and implement solutions, and evaluate outcomes. 4. Interpersonal Skills – The ability to interact effectively with patients, families, colleagues, other health care professionals, and the community in a culturally aware manner. 5. Responsibility – The ability to be accountable for the outcomes of personal and professional actions and to follow through on commitments that encompass the profession within the scope of work, community and social responsibilities. 6. Professionalism – The ability to exhibit appropriate professional conduct and to represent the profession effectively while promoting the growth/development of the Physical Therapy profession. 7. Use of Constructive Feedback – The ability to seek out and identify quality sources of feedback, reflect on and integrate the feedback, and provide meaningful feedback to others. 8. Effective Use of Time and Resources – The ability to manage time and resources effectively to obtain the maximum possible benefit. 9. Stress Management – The ability to identify sources of stress and to develop and implement effective coping behaviors; this applies for interactions for: self, patient/clients and their families, members of the health care team and in work/life scenarios. 10. Commitment to Learning – The ability to self direct learning to include the identification of needs and sources of learning; and to continually seek and apply new knowledge, behaviors, and skills. May WW, Morgan B, Lemke JC, et al. Model for ability-based assessment in physical therapy. Journal of Physical Therapy Education. 1995;9(1):3-6. *Professional Behaviors were developed by Warren May, Laurie Kotney and Annette Iglarsh (2010) as an update to the Generic Abilities referenced above. The Core Values (American Physical Therapy Association, 2002) Students are expected to selfassess and demonstrate the Core Values frequently. 1. Accountability 2. Altruism 3. Compassion/Caring 4. Excellence 5. Integrity 6. Professional Duty 7. Social Responsibility Clinic Preparation The student is required to be current in all health records, CPR, criminal background check and other items as stated in the clinical contract and additional documentation before beginning any clinical experience. Clinical Education Promotion and Dismissal Policies statement Clinical experiences are expected to be in a variety of settings with the expectation of entry- level competence at the completion of the second and third internships. All clinical experiences must be passed in progression to continue in the program and meet program requirements for graduation. Grading Policy A grade of Pass, Incomplete or Fail can be awarded for each clinical experience. The grade is determined by the DCE with input from the CI and CCCE and when necessary, the SU PT faculty. The pass/fail grade relates to the quality and consistency of the student performance, efficiency and complexity of tasks as appropriate for level, amount of supervision/guidance, and adherence to all safety criteria. Pass The student meets the criteria for level in the program. 60% of the grade is reflected in the grade assigned to the clinical internship by the DCE. 40% of the grade is reflected in the following: completeness and timeliness of the assignments (15%), attendance at class meetings (10%), and timely submission of all required forms (15%). Assignments (15% of course grade) Clinic assignments need to be turned into Blackboard by the date listed, one page max. The purpose is to increase your awareness of your professional growth and behaviors. No points will be awarded for assignments not in Blackboard on the due date. PROOF OF ATTENDANCE at an 8-hour Continuing Education Course and Conclave is required by the completion of Clinical Internship 3. (Class of 2014 – 16 hours a NSC accepted.) Class meetings (10% of the course grade) There will be a minimum of 3 MANADATORY class meetings scheduled during semester. These meetings are required as they cover policy and procedures related to successful clinical practice, including expectations for performance, understanding the clinical evaluation tool, clinical practice assignments, and discussion of issues pertinent to clinical education. If for some reason, the student is unable to attend or will be tardy, the student is expected to notify the instructor prior to the class. Excused absences follow University guidelines (personal illness, death in the immediate family) and professional or special activities that have prior approval. Physician and dental appointments, etc, other than emergency, are not excused absences. In the event of a missed meeting, the student will be required to obtain the content from a classmate, and complete any required material within one week of the class meeting. It is the responsibility of the student to obtain the information presented in the meeting. Submission of Forms (15% of the course grade) Grades for all clinical experience are pass/fail/incomplete. It is the responsibility of the student to see that all materials (grading forms, evaluations of the clinical site, course evaluations and other information/assignments as required) are complete and turned into the DCE by the stated deadlines. Delays or repeat emails to individuals will be reflected in a decrease in this portion of the grade. Incomplete An incomplete will be assigned following the guidelines in the graduate student handbook. Fail Did not meet the criteria for your level in the program. Failure to complete paperwork (unless extenuating circumstances are apply and are accepted) will result in the student not being allowed to continue the succeeding semester in the clinical experiences. A failed clinic will be repeated in a similar clinical learning environment (if possible) at the discretion of the faculty. The student will be required to register for the repeat course. If a second or repeat clinical experience is failed, the student cannot continue in the program as failure of a second course, regardless of GPA, results in dismissal from the Division of Physical Therapy (12.0 Student handbook). Remediation procedures When necessary remediation will take place during a clinical experience. The DCE, the student, the CI, and CCCE will be involved in writing a remediation contract. The contract will identify specific areas of deficit and the expected outcomes to demonstrate improvement. The contract requirements must be fulfilled in addition to the usual expectations for the clinical experience. Inservice/Service in Kind The student is required to provide education to the PT (or other) staff members of the affiliating institution. This can be a didactic session or service-in-kind (a brochure or quality assurance, etc.). Any unoriginal materials (i.e.: class notes) used for the inservice must follow appropriate copyright laws. Disabilities Any student who has a disability and is in need of clinic accommodations, please contact the instructor and the Office of Academic Affairs. (540-665-4525). Dress Code See student handbook. Reminder: maximum of two earrings/ear and no other visible body piercing or tattoos. No hats, no exposed torso, no gum. Keep nails short. Honor Code Patient safety and professionalism, in addition to trust and mutual respect are critical behaviors in a health care environment. To encourage and support such an environment, Shenandoah University has adopted an Honor Code. Students are expected to read the provision of the Honor Code and to abide by them. The Shenandoah University Honor Code allows for evaluative judgments to be made based on professional conduct and ethical behavior. Should a student be found guilty of violations of the Honor Code the student may not be given the option to repeat a clinical experience. Plagiarism Plagiarism is the willful copying of the language, structure, ideas, or thoughts of another person without proper acknowledgement, or submitting purchased work, or misrepresenting another person’s work as one’s own. Plagiarism will not be tolerated and is an Honor Code offense. These policies are subject to change and based on the needs of the student and the ability of the clinics and program to accommodate the needs of the student. Syllabus Internship 2 & 3 December 2012