36) Scope_of_Anesthesia_Services
advertisement

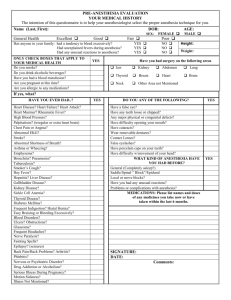
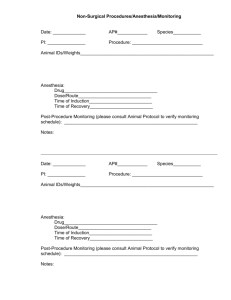
MEDICAL STAFF POLICY & PROCEDURE TITLE: SCOPE OF ANESTHESIA SERVICES No. MS-9 Effective Date: 06/11 _____________________________________________________________________________ POLICY: Anesthesia services throughout the hospital are under the direction of the Medical Director of Anesthesia Services. Anesthesia services are divided into two categories to include “Anesthesia” and “Conscious Sedation/Analgesia.” PURPOSE: The purpose of these policies and procedures is to establish the standards and expectations for all patients receiving anesthesia services, including but not limited to, topical or local anesthesia, minimal sedation, moderate sedation/analgesia, deep sedation/analgesia, regional anesthesia and general anesthesia. These policies and procedures apply to all locations in the hospital where anesthesia services are administered, including but not limited to the Operating Room suite (both inpatient and outpatient), Emergency Department, Critical Care areas, Obstetrical Suite, Radiology Department, Psychiatry Department, Recovery Rooms, Outpatient Clinics, Outpatient surgery areas, and Special procedure areas, e.g. Endoscopy Suite and Pain Management Clinics, and including all departments in all campuses and off-site locations where anesthesia services are provided. This policy specifically does not apply to patients who are intubated, mechanically ventilated, appropriately monitored, and intentionally sedated for longer periods of time in an ICU/ER environment. PROCEDURE: (A) DEFINITIONS (1) The practice of “anesthesia” specifically includes: General Anesthesia, Regional Anesthesia, Monitored Anesthesia Care (MAC) (Deep Sedation/Analgesia). (2) General anesthesia, regional anesthesia and monitored anesthesia care, including deep sedation/analgesia, may only be administered by a qualified anesthesiologist; a non-anesthesiologist MD or DO credentialed by SAMC to administer “anesthesia”, a CRNA who is supervised by an anesthesiologist who is immediately available if needed. ; or an anesthesiologist’s assistant under the supervision of an anesthesiologist who is immediately available if needed. (3) A CRNA administering general, regional and monitored anesthesia must be supervised either by an anesthesiologist who is immediately available if needed, and not otherwise occupied in a way that prevents him/her from immediately conducting hands-on intervention, if needed. (4) An anesthesiologist’s assistant may administer anesthesia when under the direct supervision of an anesthesiologist. The anesthesiologist must be immediately available if needed, and not otherwise occupied in a way that prevents him/her from immediately conducting hands-on intervention, if needed. (5) General Anesthesia is a drug-induced loss of consciousness during which patients are not arousable, even by painful stimulation. The ability to independently maintain ventilatory function is often impaired. Patients often require assistance in maintaining a patent airway, and positive pressure ventilation may be required because of depressed spontaneous ventilation or drug-induced depression of -1- (6) (7) (8) (9) (B) neuromuscular function. Cardiovascular function may be impaired. Deep Sedation/Analgesia is a drug-induced depression of consciousness during which patients cannot be easily aroused but respond purposefully following repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. Patients may require assistance in maintaining a patent airway, and spontaneous ventilation may be inadequate. Cardiovascular function is usually maintained. The Policy for the practice of “Conscious Sedation/Analgesia” specifically including Topical or Local Anesthesia, Minimal Sedation, and Moderate Sedation/Analgesia (“Conscious Sedation”) can be found in the Medical Staff Policy Guidelines for Moderate (Conscious) Sedation and Analgesia. Moderate Sedation/Analgesia (“Conscious Sedation”) is a drug-induced depression of consciousness during which patients respond purposefully to verbal commands, either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascular function is usually maintained. Because sedation is a continuum, it is not always possible to predict how an individual patient will respond. Hence, practitioners must be prepared to rescue patients whose level of sedation becomes deeper than initially intended, for example, patients who inadvertently enter a state of Deep Sedation/Analgesia when moderate sedation was intended. Rescue of a patient from a deeper level of sedation than intended is an intervention by a practitioner proficient in airway management and advanced life support. The qualified practitioner corrects adverse physiologic consequences of the deeper-than intended level of sedation (such as hypoventilation, hypoxia and hypotension) and returns the patient to the originally intended level of sedation. MEDICAL DIRECTOR OF ANESTHESIA SERVICES (1) The Medical Director of Anesthesia Services has the responsibility and authority for developing policies and procedures governing the provision of all categories of anesthesia services, including specifying the minimum qualifications for each category of practitioner who is permitted to provide anesthesia services. Anesthesiology is the practice of medicine including, but not limited to, preoperative patient evaluation, anesthetic planning, intra-operative and postoperative care and the management of systems and personnel to support these activities. In addition, anesthesiology involved peri-operative consultation, the prevention and management of untoward peri-operative patient conditions, the treatment of acute and chronic pain, and the care of critically ill patients. This care is personally provided by or directed by the anesthesiologist who possesses the Degree of Doctor of Medicine (M.D.) or Doctor of Osteopathy (D.O.) (2) The Medical Director of Anesthesia Services has the authority and responsibility for directing the administration of all anesthesia services throughout the hospital including all departments where anesthesia services are provided. All anesthesia services includes both “anesthesia” and “sedation/analgesia” services. (3) The Credentials Committee certifies the credentials for specific anesthesia service privileges which are ultimately granted by the Medical Executive Committee, and approved by the Hospital Board, including type and complexity of procedures, for each practitioner who furnishes anesthesia services, addressing the type of supervision required, if applicable. Clinical privileges in the practice of anesthesia are granted to physicians and CRNAs, and AAs who are qualified by training to administer general anesthesia, regional anesthesia, monitored anesthesia care, and deep sedation/analgesia that will render patients insensible to pain and minimize stress during surgical, obstetrical and certain medical procedures. Clinical privileges are also granted to qualified practitioners who are not -2- (4) (5) (6) (7) anesthesia professionals to administer sedative and analgesic drugs to establish a level of moderate or minimal sedation. Specifically, Board Certified Emergency Physicians who have documented anesthesia training in their residency program may provide deeper levels of sedation under specific conditions in the Emergency Room environment. Similar to Conscious Sedation Practice Guidelines an abbreviated history and physical must be performed, including assessment of the patient’s airway, and an ASA Classification Status assigned. The patient must be NPO (6-8 hours for solids, 2-3 hours for clear liquids) and the risk factors for aspiration considered. The patient should be monitored to include EKG, Blood Pressure, Pulse Oximetry, and expired End Tidal CO2 as an indication of a patent airway gas exchanging airway. The practice of unconscious sedation in the Emergency Room environment should always allow for two Board Certified ER physicians, one to manage the airway during the procedure, and the other to administer medications. Although the State of Alabama does allow the operating practitioner to supervise a CRNA administering anesthesia, operating practitioners do not supervise a CRNA administering anesthesia at SAMC. Delivery of anesthesia services consistent with recognized standards for anesthesia care include: Patient consent, infection control measures, safety practices in all anesthetizing areas; protocols for supportive life functions including cardiac and respiratory emergencies, reporting and documentation requirements, equipment requirements, as well as the monitoring, inspection, testing, and maintenance of anesthesia equipment in the hospital’s biomedical equipment program, delineation of pre- and post-anesthesia staff responsibilities, responsibility for planning, directing and supervising all activities of the anesthesia service, responsibility for establishing staffing schedules, responsibility for evaluating the quality and appropriateness of the anesthesia patient care. The Medical Director of Anesthesia Services should have: successfully completed a training program in anesthesiology accredited by the Accreditation Council for Graduate Medical Education (ACGME), the American Osteopathic Association (AOA) or equivalent organization, possess a current, full and unrestricted license to practice medicine in the State of Alabama, possess a current, unrestricted DEA registration (schedules II-IV) or no history of revocation of DEA registration (schedules II-IV) within the past five years, possess either a permanent certification by the American Board of Anesthesiology (ABA) or maintain current recertification within the time interval required by the ABA, and maintain compliance with the ABA Maintenance of Certification in Anesthesiology Program (MOCA), and maintain compliance with Alabama requirements for CME for state licensure. Approved by: Medical Executive Committee: 5-10-11 Board: 06-28-11 Reviewed/Revised: 09-15-11; 2-2012 -3-