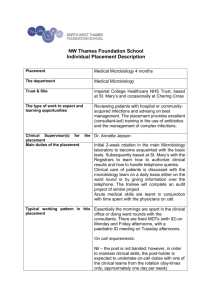
Paediatric Continuing Care Assessment Form
advertisement

NHS Additional Funding Contribution Assessment Form1 Guidance to Professionals completing this assessment form The NHS funds services to meet the child’s health needs regardless of where they live. In order to be eligible for additional funding to support an individually commissioned placement/treatment package, it is necessary to demonstrate why the child’s health need cannot be met from mainstream NHS services. The decision making body for these funding requests is the Children’s Complex Cases Panel (CCCP). This form should be completed as fully as possible and relevant supporting evidence attached. The documentation presented by NCC to the CCCP must include as a minimum a report from either, a Consultant Clinical Psychologist, Paediatrician or Child Psychiatrist and ensure that the questions below have been addressed. All cases presented to the CCCP should have previously been discussed at and have full approval from the relevant NCC CS’s County Panel. There is no process in place for urgent decisions to be made outside of the CCCP for this group of children. If the health need is urgent the child will receive treatment in the normal way via A&E or be admitted to an appropriate in-patient bed. NHS professionals who are working with a child or young person who NCC is considering for a specialist placement/care package should provide evidence based advice to support the CCCP decision making. Health professionals should be clear in all communications to NCC staff that, whatever their recommendations, they are not able to commit resources and that this decision sits with the CCCP. Their report should contain detailed information on the child’s health needs, the resource/therapy requested and how it will meet the child’s health needs. It should also explain the limitations of local child health services and why they are not able to support the child adequately. Please note - where, e.g. a Clinical Psychologist provides advice to NCC on the suitability of a placement in terms of meeting the child’s social care or educational needs, this in no way implies that a child will be entitled to additional NHS funding. 1 This form is in draft and will be piloted for 6 months from March 2012 Page 1 of 9 Date of consent by person/s with Parental Legal status of child Responsibility to this assessment/information sharing with NHS Complex Cases Panel __/__/__ (Written consent to be attached) Child’s Name: NHS No: Address: Date of Birth: Tel no Mobile: Family members Relationship D.O.B Child lives with: Height & Weight of Child: Date Weight Recorded: Summary of Family & Social Background: (please append relevant detailed reports) Current health problems: GP name and address: Consultant(s): Paediatrician/s Psychiatrist Psychologist Page 2 of 9 Contact number Ethnic origin: School/Nursery: Language spoken: Why is a health contribution being requested? INVOLVED PROFESSIONALS NAME Social worker Health visitor/school nurse Children’s community nursing team Learning disability nurse Outreach nurse Physiotherapist Occupational therapist Speech and language therapist Dietician Education professionals Class teacher Educational Psychologist SEN Caseworker Others – please specify Page 3 of 9 TELEPHONE NUMBER CARE REQUIREMENTS Please complete the following sections or clearly signpost in each section to where evidence can be found within reports attached (e.g. Assessment report from Darwin House page .., paragraph …) Behaviour Does s/he have challenging behaviour? Are there any specific triggers for this? Describe the specific behaviours and symptoms including duration and severity and ability to self regulate behaviours. Does s/he have impaired capacity for emotional regulation and behavioural control and/or impaired capacity for empathy and impulse control leading to aggressive and other behaviours that place the young person and / or others at risk and leading to significant impairment in the young person’s life. Detail level of supervision required in various settings, day/night to manage risk. Communication Describe the child’s ability to communicate their needs in familiar and unfamiliar situations. How does he/she communicate? (e.g. communication aids) Is she/he visually impaired? Does he/she wear glasses or a hearing aid? Page 4 of 9 Mobility Is it normal for his/her age? Is their sleep affected by their problems? Nutrition . Are there special dietary needs? Are there problems with intake of food of food or drink requiring skilled intervention to manage nutritional needs; recognised eating disorder with self imposed dietary regime of self neglect, e.g. depression leading to intake problems placing young person at risk? Continence or Elimination Is he/she continent? Does she manage menstruation appropriately? Skin Any areas of concern? Eczema or other skin conditions? Self Harm related problems? Breathing Any use of inhaler / nebulisers? Is monitoring required? Is overnight ventilation required? Are sleep patterns affected? Page 5 of 9 Drug Therapies & Medicines Is he/she on regular medication? Are there issues of non-compliance? If so what level of support/supervision is required? Does he/she have emergency medication? (epipen, buccal midazolam etc) Does pain affect sleep regularly? Psychological Are there: - Signs of unresolved emotional distress/ low mood and an inability to be comforted. - Fluctuating levels of distractibility and poor attention - Anxiety with high levels of safety behaviours and avoidance - Thought disorder - Rapidly fluctuating moods of depression which have severe impact on child’s health so that individual can’t engage with daily activities eg eating, sleeping or which place them at risk. - Episodes of acute psychological deregulation, poor impulse control placing child at risk to self and others, including high risk intentional self harm. Seizures Description of type of seizure What is the seizure pattern? Is a recovery period required? Page 6 of 9 Interventions to date. What methods have already been employed to try and resolve the child’s difficulties? Give full details of the placements the child has lived in and medical and therapeutic input received. Please give names of professionals involved and dates of treatment What was the outcome of the therapy/ treatment? What was resolved? What difficulties remain? Is further therapy/treatment planned? Proposed intervention Why is this placement being considered at this point in time? What else has been considered? Why where these deemed unsuitable? How will the proposed placement benefit the child? What are the components of the package of care and treatment that is requested? Please be specific. What effects are these likely to have on the child’s difficulties? How long is the suggested package of care needed for? How long is the treatment needed for? Please give an explanation for the length predicted. Page 7 of 9 What is the evidence to support a likely positive health outcome? Does the health professional treating the child believe this likely? Monitoring and Evaluation How will the child’s progress be monitored and evaluated? Who will be responsible for monitoring and what input will health professional/s have into this? How will it be decided that sufficient improvement has been achieved and the treatment or placement is no longer needed? What will be the plan for the child following this placement? Current situation Where is the child living at the time of this assessment, e.g. at home, foster care, residential care, hospital, hospice, short breaks setting. Views of person/s with PR about proposed placement/intervention Carers’ view if different Page 8 of 9 Views of child about proposed placement/intervention Form Completed by: Print Name: Signed: Designation: Date: Declaration (Paediatric consultant or panel signatory only) This patient is ELIGIBLE for additional NHS funding in addition to the mainstream NHS services already in place. Please Tick Yes No Print Name: Signed: Designation: Date: Page 9 of 9