Self-Management in Patients with End Stage Renal Disease
advertisement

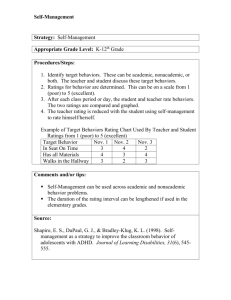
Self-Management in Patients with End Stage Renal Disease: Exploring Domains and Dimensions Roberta Braun Curtin, Donna Mapes, Dori Schatell, Sally BurrowsHudson. Nephrology Nursing Journal. Pitman: Jul/Aug 2005.Vol.32, Iss. 4; pg. 389, 7 pgs » Jump to full text » Translate document into: » More Like This - Find similar documents Subjects: Author(s): Document types: Publication title: Source type: ISSN/ISBN: ProQuest document ID: Text Word Count Document URL: Select language Kidney diseases, Medical treatment, Hemodialysis, Disease management, Neph Roberta Braun Curtin, Donna Mapes, Dori Schatell, Sally Burrows-Hudson Feature Nephrology Nursing Journal. Pitman: Jul/Aug 2005. Vol. 32, Iss. 4; pg. 389, 7 pg Periodical 1526744X 889774431 5072 http://proquest.umi.com.dbgw.lis.curtin.edu.au/pqdweb?did=905723471&sid=1& Abstract (Document Summary) The management and appropriate treatment of chronic disease are ongoing challenges in health care. As the population ages, the prevalence of chronic disease can be expected to increase. Since by definition there is no cure for chronic disease, controlling, minimizing, or managing its negative effects becomes a primary goal. In the self-management perspective, it is neither clinicians nor health care systems who must accomplish the bulk of chronic disease management but rather the patients themselves. Moreover, selfmanagement has been shown to be associated with improved outcomes. Selfmanagement is comprised of two domains: self-management of health care and self-management of everyday life. Self-management of health care includes self-care activity, partnership in care, communication, self-care self-efficacy, and adherence. Self-management of everyday life entails achieving/maintaining "normality" in everyday roles and functioning. End stage renal disease (ESRD) is a chronic diseasefor which self-management is particularly relevant. Understanding the components of self-management may help patients and clinicians to embrace this approach, to enter the mutual relationship it requires, and to maximize positive outcomes for patients with ESRD. [PUBLICATION ABSTRACT] Full Text (5072 words) Copyright Anthony J. Jannetti, Inc. Jul/Aug 2005 [Headnote] The management and appropriate treatment of chronic disease are ongoing challenges in health care. As the population ages, the prevalence of chronic disease can be expected to increase. Since by definition there is no cure for chronic disease, controlling, minimizing, or managing its negative effects becomes a primary goal. In the selfmanagement perspective, it is neither clinicians nor health care systems who must accomplish the bulk of chronic disease management but rather the patients themselves. Moreover, self-management has been shown to be associated with improved outcomes. Self-management is comprised of two domains: self-management of health care and self-management of everyday life. Self-management of health care includes self-care activity, partnership in care, communication, self-care self-efficacy, and adherence. Self-management of everyday life entails achieving/maintaining "normality" in everyday roles and functioning. End stage renal disease (ESRD) is a chronic diseasefor which self-management is particularly relevant. Understanding the components of selfmanagement may help patients and clinicians to embrace this approach, to enter the mutual relationship it requires, and to maximize positive outcomes for patients with ESRD. Management and appropriate treatment of chronic disease are ongoing challenges for health care institutions as well as for society as a whole (Clark, 2003). In the next 20 years, the number of people in the U.S. over the age of 65 is expected to increase to more than 53 million, and there is every reason to believe that as the population ages, the prevalence of chronic disease will increase concomitantly (Bodenheimer, Lorig, Holman, SL Grumbach, 2002). Chronic disease is already the principal basis for disability, the main reason for health care seeking, and is responsible for 70% of health care spending in this country (Holman & Lorig, 2000). Since no cure is available for most chronic diseases, controlling, minimizing, or managing negative effects becomes an important charge. Any chronic disease may require significant medical intervention over its course. Nonetheless, some believe that clinicians and health care systems cannot bear the major responsibility for the management of chronic disease on an everyday basis; but rather that patients themselves must do so (Clark, 2003). Moreover, at the same time that it is becoming increasingly apparent that some degree of patient self-management is necessary in chronic disease, there is also growing verification that selfmanagement by patients contributes to better health outcomes (Lorig, Sobel et al., 1999; Meers et al, 1996). As is evidenced by its explicit inclusion in the Institute of Medicine (IOM) report, Crossing the (Quality Chasm: A New Health System for the 21st Century (IOM, 2003), the topic of patient self-management has definitely come of age in the U.S. End stage renal disease (ESRD), whether treated by transplant or dialysis, is a chronic disease for which patient self-management is particularly important. Individuals with ESRD are at risk for a broad array of complications, experience many symptoms, have stringent dietary and fluid restrictions, and have to adhere to complex medication regimens. Simply stated, the goal of chronic disease management is to simultaneously achieve the highest level of functioning and the lowest level of symptoms given the severity of the disease (Clark, 2003). In the case of ESRD, this goal is largely unattainable without patients' active and comprehensive self-management of all aspects of life with ESRD (Curtin, Johnson, Schatell, 2004; Curtin, Mapes, Petillo, & Oberley, 2002). Self-Management of Health Care and Self-Management of Everyday Life Gruman and Von Korff (1996) have proposed that self-management involves patients' engagement in activities that protect and promote health; their observation of symptoms and signs of illness; their adherence to treatment regimens; and their management of the effects of illness on functioning, emotions, and interpersonal relationships. Similarly, Curtin and Mapes (2001) have defined self-management as "patients' positive efforts to oversee and participate in their health care to optimize health, prevent complications, control symptoms, marshal medical resources, and minimize the intrusion of the disease into their preferred lifestyles" (p. 386). Enlarge 200% Enlarge 400% Figure 1 Patient Self-Management of Chronic Illness The same two distinct and major domains of self-management can be distilled from each of these definitions (see Figure 1). The first domain is selfmanagement of health care. This self-management of health care domain subsumes several interdependent dimensions: (a) communication, (b) partnership in care, (c) adherence, (d) self-care activities, and (e) self-care selfefficacy (Curtin, Johnson, et al., 2004; Holman & Lorig, 2000; Zrinyi et al., 2003). The second domain suggested by both definitions of self-management is self-management of everyday life, which is represented as "functioning, emotions, and interpersonal relationships" in the first definition and as "preferred lifestyles" in the second. This second domain involves achievement and maintenance of "normality" in usual roles and functioning (Curtin, Johnson et al., 2004; Kelly-Powell, 1997; Lindqvist, Carlsson, & Sjoden, 2000). The First Domain Self-management of health care: Communication. Communication is the cornerstone upon which the other dimensions of self-management are built; none of the other dimensions is possible without good communication between patients and clinicians. For self-management to be a possibility, patients must be able to report their symptoms, problems, experiences, and concerns, and must receive, in turn, from the health care team, information, answers, support, and guidance. The ultimate endpoint of effective communication is "concordance" - an agreement between a patient and a health care professional that respects the patient's wishes and beliefs and assures that the patient has had a proactive role in treatment decisions (Epstein, Alper, & Quill, 2004; UKDepartment of Health, 2001; UK-Department of Health, 1999). It is important for clinicians to communicate specific information and messages that patients can translate into actual self-care behaviors. As well-known author on the topic Noreen Clark (2003) notes, "Information that is irrelevant to patients' personal concerns or that does not affect behavior is not constructive" (p. 306). Clark further suggests that although clinicians other than physicians can provide such information, the doctor is usually viewed by patients as the most credible source of medical advice. In the case of patients with ESRD treated with hemodialysis (HD) or peritoneal dialysis (PD), dialysis nurses may also be able to fill this role. Similarly, transplant patients may look to their transplant coordinators for regular information exchange. Regardless of which member of the health team serves as the primary "communicator," it is clear that regular, mutual, and comfortable exchanges of experience and information between clinicians and patients can clarify the best possible ways to manage the disease and its effects in everyday life (Bodenheimer et al., 2002; Clark, 2003). Self-management of health care: Partnership in care. Partnership in care is a second key component of self-management. Its interdependence with the communication dimension is clear: Partnership is only possible with effective communication (Clark, 2003; Epstein et al., 2004). In the past, health care professionals were considered the experts in health care and patients were regarded as passive recipients of care (Bodenheimer et al., 2002). This perspective, which was useful in the treatment of acute illness, has been replaced by a paradigm that better suits the reality of chronic dis ease in general and ESRD in particular (Bodenheimer et al., 2002; Curtin & Mapes, 2001; Lorig & Holman, 2003). The new viewpoint suggests that patients need to become experts in their own health care since they literally live with their illness and its consequences every day (UK-Department of Health, 2001). However, although patients may become knowledgeable about their own illness experience and circumstances, it is not possible for them to safely engage in self-care activity unless excellent communication has been established and a working partnership relationship with key health care professionals is in place. For example, patients with ESRD frequently suffer from one or more comorbid conditions and also may have a broad array of symptoms on a fairly regular basis (Curtin, Bultman, Thomas-Hawkins, Walters, & Schatell, 2002). To be effective self-managers, patients must be able to distinguish between symptoms/situations they can manage themselves (at least until their next meeting with their health care professionals) and those which should be reported immediately (Curtin, Mapes et al., 2002). They must be encouraged to manage the self-manageable and to consult with their health care partners for circumstances that need urgent intervention. This is a far more independent and proactive role for patients than has been the case in the past, and such a role is really only possible if a true partnership relationship has been established (UKDepartment of Health, 2001). Successful partnership assures that self-care activity is informed, monitored, tailored, and modified as necessary. If the partnership is successful, the benefits of self-management can be realized and patients' overall care can be optimized. Self-management of health care: Adherence. Since repeated studies of the topic of adherence to medical regimens have been unable to identify consistent predictors of non-adherence, it is probably safest and most practical to assume that all patients need some combination of special interventions to increase the likelihood of adherence (Clark, 2003; Kutner, 2001; Morgan, 2000). Selfmanagement pioneer Kate Lorig (2002) suggests that patients are the best judges of what is actually possible for them and may be non-adherent if the expectations of their health care professionals are not realistic for their circumstances. This observation once again illustrates the interdependence of the various dimensions of self-management. If communication is effective and a partnership relationship is in place, adherence will be more likely. This is the case because good communication in the partnership context allows for feedback to be given and received and for appropriate goals for patients' health activities and behaviors to be negotiated rather than "imposed." For patients with ESRD, adherence to the treatment regimen is both particularly important and particularly difficult. For example, patients on dialysis must have regular dialysis sessions that are time consuming and sometimes uncomfortable. Non-adherence to dialysis prescriptions is associated with an increased risk of mortality and morbidity (Bernardini, Nagy, & Piraino, 2000; Leggat et al, 1998). Additionally, virtually all patients with ESRD are likely to be required to monitor diet and fluid intake and to take multiple medications - in addition to following a generally healthy lifestyle overall with regard to smoking, alcohoi, weight maintenance, regular exercise, etc. Although specific strategies to improve adherence among patients requiring dialysis and transplant have not been systematically examined, the principles subsumed under the rubric of selfmanagement (i.e., self-care, partnership in care, improved communication, and increased self-efficacy) seem a most likely route to increased adherence (Kutner, 2001; Loghman-Adham, 2003). Self-management of health care: Self-care activity. In the recent past, the terms self-care and self-management have been used interchangeably (Curtin & Mapes, 2001; Lorig & Holman, 2003). It is only as our understanding of the concept of self-management has matured over the past several years that it has become increasingly apparent that self-care is just one of several dimensions of the self-management domain (Curtin, Johnson et al., 2004). As its name implies, self-care is the "action" dimension of self-management in health care and it derives in part from a patient empowerment approach. Patient empowerment has been defined as a philosophy of health care that proceeds from the perspective that optimal outcomes of health care are achieved when patients become active participants in the health care process (Brennan & Safran, 2003). Without a doubt, being active in health care includes performing at least some aspects of physical care. As such, self-care behaviors, such as measuring fluid intake or blood pressure or checking access bruit are included (Curtin, Bultman Sitter, & Schatell, 2004). However, more general health care related action steps are also subsumed in the dimension of self-care, including interacting with health care professionals, goalsetting, contacting resources, negotiating for and choosing treatments, decision making, information-seeking, responsibility for consequences, symptom reporting, wellness behaviors, etc. For patients with ESRD, the level of self-care activity required may vary by modality and from patient to patient. However, every ESRD patient must make decisions on a daily basis about positive and negative health-related behaviors and must perform a whole host of specific health-related self-care activities as well. The empowerment perspective suggests that patients can acquire the knowledge, skills, and responsibility to take action and effect changes that can improve their health care and promote their overall health status (Anderson et al., 1995; Feste & Anderson, 1995; Funnell et al., 1991). Because of its broad applicability to people with chronic illnesses, self-care, as it is viewed in the empowerment perspective is an integral part of overall self-management of health care. Self-management of health care: Self-care self-efficacy. Self-care self-efficacy is another important dimension of overall self-management. Ongoing qualitative research has consistently verified the important role that "feeling in control" plays in individuals' self-described quality of life and successful adaptation to life with a chronic disease (Curtin, Johnson et al., 2004; Curtin, Mapes et al., 2002; Lenker, Lorig, & Gallagher, 1984). In an effort to further explore and understand such findings, Lorig and her associates operationalized the concept of control or empowerment as self-efficacy and then examined it in the context of selfmanagement activities and outcomes (Lorig SL Holman, 2003). The investigations yielded the expected results: Increased self-efficacy is associated with positive changes in health care behaviors as well as in health status (Lorig, Gonzalez, & Ritter, 1999; Lorig & Holman, 2003; Lorig, Sobel et al., 1999). In practice, perceived self-efficacy means that individuals are confident that they can perform certain actions to achieve desired outcomes, and are also secure in the belief that the actions they take will produce the outcomes they seek (Bandura, 1997). With regard to ESRD, research has verified the relationship between the self-efficacy of patients on HD and their interdialytic weight gain, serum potassium levels, "favorable" compliance attitudes, and better relationships with staff (Zrinyi et al., 2003). Other research has suggested a relationship between selfefficacy and positive mood states, health status, and improved adherence to fluid limits (Lev & Owen, 1998). Evidence is growing that building confidence around a self-care or treatment regimen behavior as part of a clinician-patient communication or an educational program may increase the likelihood of that behavior (Clark & Dodge, 1999). Certainly, selfcare principles must be taught and self-care skills developed as well. However, building patients' confidence in their ability to affect the outcomes they have targeted seems to be another positive way to encourage successful selfmanagement among people with chronic illness. The second Domain Self-management of everyday life: Achieving or maintaining "normality." The second major domain of overall self-management is self-management of everyday life. This domain is embodied in the single dimension of normality (i.e., individuals' ability to achieve or maintain what is perceived as "normal" in as many aspects of everyday living as is possible). In acute illnesses, patients suspend their normal lives until they can recover from their illness. Once recovered, they expect to be able to resume those same lives and occupy the same roles (Curtin & Mapes, 2001). The situation is very different with the diagnosis of a chronic illness. Because chronic disease is life-long, patients are required to make adjustments to their "normal" ways of living. A first step in this process is taking stock of the nature and scope of the constraints imposed by the illness and then learning to live within them (Morse, 1997). Either old role repertoires must be adapted to fit the constraints of the condition, or new role repertoires must be developed (Curtin, Mapes, Petillo & Oberley, 2002). Additionally, patients must address the emotional ramifications of having a chronic condition, a reality which necessarily alters their overall views of life, their goals, and their aspirations (Corbin & Strauss, 1988; Morse, 1997). The desire for as near "normal" a life as possible is commonly reported by patients on dialysis. In one qualitative study of patients on PD, a pervasive "wish for independence and normality" was identified (Lindqvist et al., 2000). In another qualitative study, efforts to "sustain the current self" included personal choices that supported the maintenance of "normal" lives and roles (KellyPowell, 1997). Finally, a recent qualitative study found that patients on PD attempted to achieve normality by using treatment flexibility as an opportunity to preserve current role repertoires or to create new ones, by facing changes in body image directly and reinterpreting new body images in as optimistic and practical a manner as possible, and by reframing diagnoses/prognoses in a positive light without denying their reality (Curtin, Johnson et al., 2004). In practice, achieving normality involves grappling with the primary areas of concern that have been identified among patients with ESRD on dialysis, including continuing symptoms, limitations resulting from dialysis treatments, relentlessness and uncertainty of life on dialysis, and an altered relationship between autonomy and dependence that is inherent in life on dialysis (Curtin, Mapes et al, 2002; Polaschek, 2003). The definitions presented earlier specified that self-management of everyday life would require that patients with chronic illness manage the effects of illness on functioning, emotions, and interpersonal relationships, and minimize the intrusion of the disease into their preferred lifestyles. Patients are seemingly able to accomplish this difficult task by preserving normality in their new lives with chronic disease. Conclusion Since there is no primary prevention or cure for most chronic diseases, the goal of chronic disease management is to achieve the highest level of functioning and the lowest level of symptoms possible, given the severity of the disease (Clark, 2003). Patient self-management of both the health care-related aspects of life and the everyday aspects of life affected by the disease seems to be the most promising route for achieving that goal. Moreover, there is substantial evidence in the literature suggesting that self-management skills can be taught, self-management efforts can be supported, and self-management activities can contribute to positive health outcomes (Lorig, Gonzalez et al., 1999; Lorig & Holman, 2003; Lorig, Sobel et al., 1999). In spite of the overall practicality of this approach and the mounting evidence for its success, self-management programming has been slow to be established on any sort of large scale or systematic basis in the US. However, the Stanford Patient Education Center, under the leadership of Kate Lorig, has enjoyed great success and has had significant impact. This center has developed and tested both condition-specific programs and also a program applicable across disease entities. Lorig and Holman (2003) reported that the latter program, the Chronic Disease Self-Management Program (CDSMP) has now been adopted by three major HMOs and 150 smaller HMOs across the U.S. Additionally, the National Health Service in the United Kingdom has initiated an Expert Patient initiative based on the principles of self-management and using both the CDSMP and ongoing consultation with Lorig as integral parts of its planning (UK-Department of Health, 2001). Although the implementation of these programs represents an enormous step forward, there is still a long way to go toward the goal of making self-management an accepted and expected part of health care. Unfortunately, there is an especially long way to go in ESRD since a comprehensive, systematic, disease-specific self-management program for patients with ESRD has yet to be designed and tested. End stage renal disease, with its associated complications, multiple symptoms, and complex treatment requirements is a chronic disease for which patient selfmanagement seems particularly appropriate. Unfortunately, there is relatively little information in the literature about self-management programming for patients with ESRD. The Life Options Rehabilitation Program has been championing self-management for patients with kidney disease, including patients with ESRD for the past 11 years, most recently through its on-line selfmanagement curriculum called Kidney School(TM) (www.kidneyschool.org). Additionally, Life Options produced a series of newsletters devoted to the topic of self-management for patients with kidney disease (Life Option Rehabilitation Program, 2001; Life Options Rehabilitation Program, 2000 a-d). Based on such information, there is reason to hope that some inroads have been developed. However, to date, the self-management efforts reported in the ESRD field have tended to be intermittent initiatives rather than long-term, programmatic interventions. The successful management of illness and treatment and the simultaneous maximization of overall quality of life are important agendas for individuals with chronic disease. Helping patients with ESRD realize these goals should be a primary responsibility of the health care professionals who provide their health care. The principles and tenets surrounding the concept of self-management seem to represent the best avenue for making such goals a reality for individuals with ESRD. If institutional level changes are slow in coming, there are nevertheless many opportunities in the practice of nephrology for encouraging self-management on a case-by-case basis. For example, nephrologists, nephrology nurses, social workers, and dietitians are all in the position to help patients with ESRD to be successful self-managers. Because nephrology nurses have contact with patients as modality decisions are being made, as the dialysis process is being learned, and as understanding of the ramifications of ESRD is beginning to occur in patients, they can be involved both in teaching patients about the value of self-management and in supporting patients in their early efforts to partner in their own care. Nephrology nurses can consistently strive for improved communication and can actively pursue the concordance that precedes patient adherence to prescribed regimens. Nurses can seek to transmit the information that patients require for making decisions regarding their own care and can help patients gain confidence that the actions they (patients) take will lead to the positive outcomes they desire. Additionally, nephrology nurses can guide and encourage patients as the patients begin to explore how they will adapt their everyday lives to the new life state in which they find themselves. Over time, even such individual level interventions will likely have a significant positive effect and will contribute to the understanding and application of the concepts of self-management for patients with ESRD. In this manner, given enough time and sufficient instances, self-management education and support might be incorporated into routine care for patients with ESRD. Additional research into the impact of self-management on the outcomes of patients with ESRD should also be a priority. Because ESRD is a chronic disease with many unique requirements, restrictions, medications, and complications, as a first step to such research, a systematic program for faceto-face teaching of self-management to patients with ESRD would have to be devised. Presumably such a program could be based on the model of Lorig's Chronic Disease Self-Management Program (CDSMP). With the established model of the CDSMP disease-specific programs as a guide, the necessary educational materials, activities and interventions might be fairly easily adapted to ESRD. Once a program was established, research in the form of modified controlled clinical trials or demonstration projects could be implemented. A wide range of patient outcomes have been considered in past research on selfmanagement, including symptom distress, adherence, self-efficacy, depression, health care utilization, functional status, quality of life, and morbidity (Anderson et al., 1995; Bodenheimer et al, 2002; Janson et al., 2003; Eev et al., 2001; Lorig, Sobel et al, 1999). Measurement of a selection of these same outcomes in a study of the impact of a self-management program for patients with ESRD would allow not only comparison between the intervention (self-management) and control groups, but would also allow comparison across disease conditions based on past research. More importantly, it would provide valuable insight into the real impact of the ESRD-specific self-management program on patient outcomes. Should the outcomes of patients with ESRD be positively affected, as were the outcomes of the patients in previous research, broader acceptance and greater appreciation of the value of self-management in the ESRD condition would likely result. As understanding of the components and requirements of self-management becomes more widespread, patients and clinicians may be increasingly motivated to adopt this valuable approach, to enter the mutual relationship it requires, and to achieve maximization of positive outcomes for patients with ESRD - thereby transforming self-management from an academic construct into a lived reality. [Reference] References Anderson, R.M., Funnell, M.M., Butler, P.M., Arnold, M.S., Fitzgerald, J.T., & Feste, C.C. (1995). Patient empowerment. Results of a randomized controlled trial. Diabetes Care, 18(7), 943-949. Bandura, A. (1997). Self-efficacy: The exercise of control. New York: Freeman. Bernardini, J., Nagy, M., & Piraino, B. (2000). Pattern of noncompliance with dialysis exchanges in peritoneal dialysis patients. American Journal of Kidney Diseases, 35(6), 1104-1110. Bodenheimer, T., Lorig, K., Holman, H., & Grumbach, K. (2002). Patient selfmanagement of chronic disease in primary care. Journal of the American Medical Association, 288(19), 2469-2475. Brennan, P., & Safran, C. (2008). Report of conference track 3: Patient empowerment. International Journal of Medical Informatics, 69(2-3), 301-304. Clark, N.M. (2003). Management of chronic disease by patients. Annual Review of Public Health, 24, 289-313. Clark, N.M., & Dodge, J.A. (1999). Exploring self-efficacy as a predictor of disease management. Health Education & Behavior, 26(1), 72-89. Corbin, J.M., & Strauss, A. (1988). Unending work and care: Managing chronic illness at home. San Francisco: Jossey-Bass Publishers. Curtin, R.B., Bultman Sitter, D.C., & Schatell, D. (2004). Self-management, knowledge, and functioning and well-being of patients on hemodialysis. Nephrology Nursing Journal, 31(4), 378-386. Curtin, R.B., Bultman, B.C., Thomas-Hawkins, C., Walters, B.A., & Schatell, D. (2002). Hemodialysis patients' symptom experiences: Effects on physical and mental functioning. Nephrology Nursing Journal, 25(6), 562- 574. Curtin, R.B., Johnson, H.K., & Schatell, D. (2004). The peritoneal dialysis experience: Insights from long-term patients. Nephrology Nursing Journal, 31(6), 615-624. Curtin, R.B., & Mapes, D.L. (2001). Health care management strategies of long-term dialysis survivors. Nephrology Nursing Journal, 28(4), 385-392. Curtin, R.B., Mapes, D., Petillo, M., & Oberley, E. (2002). Long-term dialysis survivors: A transformational experience. Qualitative Health Research, 12(5), 609-624. Epstein, R.M., Alper, B.S., & Quill, T.E. (2004). Communicating evidence for participatory decision making. Journal of the American Medical Association, 257(19), 2359-2366. Feste, C., & Anderson, R.M. (1995). Empowerment: From philosophy to practice. Patient Education and Counseling, 25(1-3), 139-144. Funnell, M.M., Anderson, R.M., Arnold, M.S., Barr, P.A., Donnelly, M., Johnson, P.O., et al. (1991). Empowerment: An idea whose time has come in diabetes education. Diabetes Education, 77(1), 37-41. Gruman, J., & Von Korff, M. (1996). Indexed bibliography on self-management for people with chronic disease. Washington, DC: Center for Advancement in Health. Holman, H., & Lorig, K. (2000). Patients as partners in managing chronic disease. Partnership is a prerequisite for effective and efficient health care. British Medical Journal, 320(7234), 526-527. Institute of Medicine (IOM). (2003). Formulating new rules to redesign and improve care. In Crossing the quality chasm: A new health system for the 27st century, pp. 6168. Washington, DC: National Academy Press. Janson, S.L., Fahy, J.V., Covington, J.K., Paul, S.M., Gold, W.M., & Boushey, H.A. (2003). Effects of individual self-management education on clinical, biological, and adherence outcomes in asthma. American Journal of Medicine, 115(8), 620-626. Kelly-Powell, M.L. (1997). Personalizing choices: Patients' experiences with making treatment decisions. Research in Nursing and Health, 20(3), 219-227. Kutner, N.G. (2001). Improving compliance in dialysis patients: Does anything work? Seminars in Dialysis, 14(5), 324-327. Leggat, J.E., Orzol, S.M., HulbertShearon, T.E., Golper, T.A., Jones, C.A., Held, P.J., et al. (1998). Noncompliance in hemodialysis: Predictors and survival analysis. American Journal of Kidney Diseases, 32(1), 139-145. Lenker, S., Lorig, K., & Gallagher, D. (1984). Reason for lack of association between changes in health behavior and improved health status: An explanatory study. Patient Education and Counseling, 6(2), 69-72. Lev, E.L., & Owen, S.V. (1998). A prospective study of adjustment to hemodialysis. American Nephrology Nurses' Association Journal, 25(5), 495-504. Lev, E.L, Daley, K.M., Connor, N.E., Reith, M., Fernandez, C., & Owen, S.V. (2001). An intervention to increase quality of life and self-care self-efficacy and decrease symptoms in breast cancer patients. Scholarly Inquiry for Nursing Practice, 75(3), 277294. Life Options Rehabilitation Program. (2001). Affirming the "self" amidst challenge and change. Renal Rehabilitation Report, 5(3). Retrieved from www.lifeoptions.org/RRR.nr_fall_or.pdf. Life Options Rehabilitation Program. (2000a). Affirming the "self" amidst challenge and change. Renal Rehabilitation Report, 8(4}. Retrieved from www.lifeoptions.org/pdfs/rrr/rrrwn00.pdf. Life Options Rehabilitation Program. (2000b). Affirming the "self" amidst challenge and change. Renal Rehabilitation Report, 8(3), www.lifeoptions.org/pdfs/rrr/rrrsu00.pdf. Life Options Rehabilitation Program. (2000c). Affirming the "self" amidst challenge and change. Renal Rehabilitation Report, 8(2). Retrieved from www.lifeoptions.org/pdfs/rrr/rrr0300.pdf. Life Options Rehabilitation Program. (2000d). Affirming the "self" amidst challenge and change. Renal Rehabilitation Report, 8(1). Retrieved from www.lifeoptions.org/pdfs/rrr/rrr0100.pdf. Lindqvist, R., Carlsson, M., & Sjoden, P.O. (2000). Perceived consequences of being a renal failure patient. Nephrology Nursing Journal, 27(3), 291-297. Loghman-Adham, M. (2003). Medication noncompliance in patients with chronic disease: Issues in dialysis and renal transplantation. American Journal of Managed Care, 9(2), 155-171. Lorig, K. (2002). Partnerships between expert patients and physicians. Lancet, 359, 814-815. Lorig, K., Gonzalez, V., & Ritter, P. (1999). Community-based Spanish language arthritis education program: A randomized trial. Medical Care, 37(9), 957-963. Lorig, K., & Holman, H. (2003). Selfmanagement education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine, 26(1), 1-7. Lorig, K., Sobel, D., Stewart, A.L., Brown, B.W. Jr., Bandura, A., Hitter, P., et al. (1999). Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Medical Care, 37(1), 5-14. Meers, C., Singer, M.A., Toffelmire, E.B., Hopman, W., McMurray, M., Morton, A.R., et al. (1996). Selfdelivery of hemodialysis care: A therapy in itself. American Journal of Kidney Diseases, 27(6), 844-847. Morgan, E. (2000). A decade review: Methods to improve adherence to the treatment regimen among hemodialysis patients. Nephrology Nursing Journal, 27(3), 299-304. Morse, J. (1997). Responding to threats to integrity of self. Advanced Nursing Science, 75(4), 21-36. Polaschek, N. (2003). Living on dialysis: Concerns of clients in a renal setting. Journal of Advanced Nursing, 47(1), 44-52. UK-Department of Health. (1999). Saving lives: Our healthier nation. London: Department of Health. Retrieved from www.ohn.gov.uk. UK-Department of Health. (2001). The expert patient: A new approach to chronic disease management for the 21s' century. London: Department of Health. Retrieved from www.ohn.gov.uk/ohn/people/ep_report.pdf. Zrinyi, M.,Juhasz, M., Balla,J., Katona, E., Ben T., Kakuk, G., et al. (2003). Dietary self-efficacy: Determinant of compliance behaviours and biochemical outcomes in haemodialysis patients. Nephrology Dialysis Transplantation, 18(9), 1869-1873. [Author Affiliation] Roberta Braun Curtin, PhD, RN, is Research Director, Medical Education Institute, Madison, WI, and research consultant, Life Options Rehabilitation Program, and is a member of the Windy City chapter of ANNA. Donna Mapes, DNSc, MS, RN, is Adjunct Senior Researcher, URREA, Ann Arbor, Ml, and Adjunct Assistant Clinical Professor, University of California San Francisco, School of Nursing, and is a member of the Chumash chapter of ANNA. Dori Schatell, MS, is Executive Director, Medical Education Institute, Madison, WI, and Program Director, Life Options Rehabilitation Program, and is a member of the Badger chapter of ANNA. Sally Burrows-Hudson, MSN, RN, CNN, is Director, Medical Affairs for Bone Care International, and Assistant Clinical Professor, University of California at San Francisco, School of Nursing. She is a Past President of ANNA, and is currently a member of the Silicon Valley chapter of ANNA.