Prudent use of antimicrobials is essential in the control of
advertisement
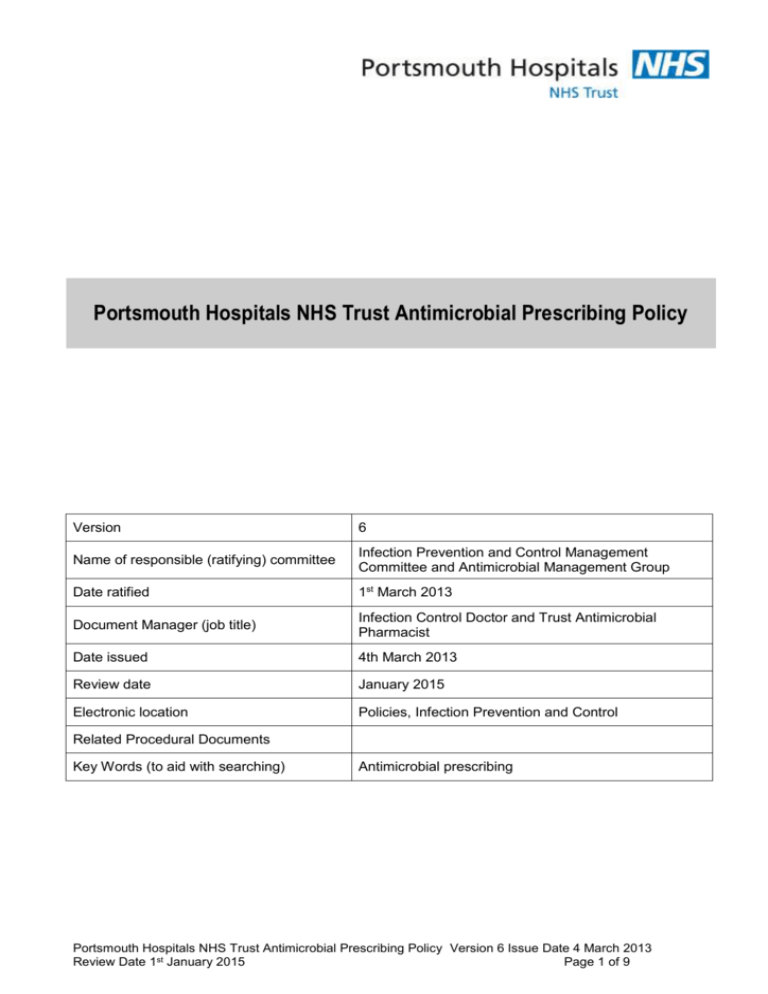
Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Name of responsible (ratifying) committee Infection Prevention and Control Management Committee and Antimicrobial Management Group Date ratified 1st March 2013 Document Manager (job title) Infection Control Doctor and Trust Antimicrobial Pharmacist Date issued 4th March 2013 Review date January 2015 Electronic location Policies, Infection Prevention and Control Related Procedural Documents Key Words (to aid with searching) Antimicrobial prescribing Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 1 of 9 CONTENTS 1. 2. 3. 4. 5. 6. 7. 8. 9. QUICK REFERENCE GUIDE....................................................................................................... 3 INTRODUCTION.......................................................................................................................... 4 PURPOSE ................................................................................................................................... 4 SCOPE ........................................................................................................................................ 4 DEFINITIONS .............................................................................................................................. 5 DUTIES AND RESPONSIBILITIES .............................................................................................. 6 PROCESS ................................................................................................................................... 6 TRAINING REQUIREMENTS ...................................................................................................... 8 REFERENCES AND ASSOCIATED DOCUMENTATION ............................................................ 8 MONITORING COMPLIANCE WITH, AND THE EFFECTIVENESS OF, PROCEDURAL DOCUMENTS .............................................................................................................................. 8 Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 2 of 9 QUICK REFERENCE GUIDE For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. 1. All antimicrobial prescribing should be rational, appropriate and safe 2. Antimicrobial therapy should only be started with clear clinical justification which should be documented in the patient’s clinical notes. The prescription should be compliant with Trust empirical guidance ie “start smart” 3. Always culture (blood, sputum, urine etc) as appropriate prior to commencing or changing antibiotics 4. Antimicrobials should be started promptly on suspicion of infection, and within one hour of diagnosis of severe sepsis and potentially life-threatening infection 5. Review antimicrobial therapy daily with culture results and clinical progress 6. Switch intavenous therapy to oral as soon as possible based on clinical response 7. Stop antibiotics as soon as possible based on clinical response and culture results 8. After 48 hours a clear plan of action should be made. The five “Antimicrobial prescribing decisions” are to stop, switch, change, continue or OPAT 9. Always check antimicrobial dosage in presence of renal or hepatic dysfunction and compatibility with other medication in the current edition of the British National Formulary 10. For all patients labeled as penicillin allergic, establish history and assess risk. Cephalosporins and Carbapenems may be given if minor allergy e.g. rash but not for patients with documented anaphylactic response 11. Support for antimicrobial prescribing is available from the antimicrobial pharmacist on bleep 1973 or from microbiology ext 1718. A consultant-led microbiology service is available 24 hours a day, 7 days a week. Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 3 of 9 INTRODUCTION Appropriate use of antimicrobials may be life-saving, but unnecessary overuse may be fatal and is contributing to the ever-increasing burden of antimicrobial resistance. Many healthcare-associated infections are precipitated by inappropriate antibiotic use e.g. Clostridium difficile, the leading cause of nosocomial diarrhoea. Inappropriate antibiotic prescribing has been shown to contribute to MRSA acquisition. Prudent use of antimicrobials is essential in the control of development of antimicrobial resistance and in the control of healthcare associated infections. Antibiotic resistant organisms are more difficult to treat (and may be untreatable), they prolong hospital admission and often cause increased morbidity and mortality. The World Health Organisation and many countries worldwide including the UK have produced strategies for the containment of antimicrobial resistance. Prudent antimicrobial use, along with infection control and improved cleanliness, surveillance of antimicrobial resistance with feedback to providers, education of professionals and the public, and making healthcare associated infection a key feature of quality and patient safety programs are all key areas for the prevention and containment of antimicrobial resistance. This document sets out the aims for antimicrobial prescribing within PHT. This policy has the full support of microbiology, pharmacy and infection prevention and control. 1. PURPOSE This policy defines the processes to ensure that antimicrobial prescribing within PHT is prudent, appropriate and safe. Proposed outcomes By adhering to this policy, antimicrobial prescribing within the Trust will be prudent, safe and appropriate, and based on the antibiotic susceptibility of diagnosed or likely pathogens. Prescribing and education on the diagnosis, management and treatment of infection will be supported by microbiology / infection experts in liaison with pharmacy and infection prevention and control. Use of intravenous antimicrobials will be minimised thereby minimising cannula-related infections including nosocomial bacteraemias. Use of antimicrobials especially broad spectrum antibacterials will be minimised thereby reducing the selection pressure for the development of resistant pathogens and for the development of antibioticassociated diarrhoea, particularly C difficile. Antimicrobial prescribing practice will be supported by active surveillance and education provided by microbiology and infection control in liaison with pharmacy. 2. SCOPE This policy applies to all prescribers of antimicrobial agents within PHT. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 4 of 9 3. DEFINITIONS Antibacterial agent A substance which selectively inhibits the growth of bacteria (bacteriostatic) or selectively kills bacteria (bacteriocidal) Antibiotic A substance produced by a micro-organism which is antagonistic to the growth or life of others in high dilution. Many antimicrobial agents are now synthetically or semi-synthetically synthesized and are thus not true antibiotics. Nevertheless the term antibiotic is widely used to refer to an antimicrobial. Antimicrobial agent A drug which is antagonistic to the growth or life of infectious pathogens, whether these are bacteria, viruses, fungi or parasites Audit The process of assessing current practices in comparison to a recognised standard Health Protection Agency Formerly the Public Health Laboratory Service, a national agency whose role is to protect the public from infection and other hazards. Hospital-acquired, healthcare associated or nosocomial infection Infection acquired in healthcare institutions. Infection Prevention and Control Team (IPCT) A group of experienced staff responsible for advising on hospital infection prevention and control. The IPCT has direct access to the Director of Infection Prevention and Control and is responsible to the Infection Prevention and Control Management Committee (IPCMC) Microbiology The study of micro-organisms Microbiologist A medical doctor qualified in the diagnosis, management and prevention of infection Microbiology ward round Also known as an antimicrobial ward round. This is a regular multi-disciplinary ward round undertaken by a microbiologist or infection specialist and a pharmacist and with a clinician who has responsibility for the patient. A member of the infection control team or a trainee microbiologist or pharmacist may also be present. The purpose of the ward round is to clinically assess the appropriateness of the antimicrobials prescribed for individual patients. All assessments take into account the current clinical situation and investigation results including any microbiology findings. Any recommendation to change the antimicrobials prescribed is discussed with the clinical staff on the wards and documented in the medical notes. The prescription chart may be actively changed by the microbiologist. Out-patient Antimicrobial Therapy (OPAT) A service provided by infection specialists to provide out-patient intravenous antimicrobial therapy Pharmacist Person qualified in the delivery, action and side-effects of medicinal drugs Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 5 of 9 4. DUTIES AND RESPONSIBILITIES All prescribers have a duty to comply with current antimicrobial prescribing guidance available on the intranet and in the British National Formulary. All prescribers should carry the empirical antimicrobial prescribing guide behind their Trust ID badge All prescribers must assess the patient’s current clinical condition and current medications, their renal and liver function and any history of allergy before prescribing an antimicrobial agent All prescribers must review their prescriptions on a regular (preferably daily) basis and rationalise any antimicrobial prescription according to the clinical state of the patient and the microbiology results Pharmacists will review all prescription charts on a regular, mostly daily, basis The antimicrobial pharmacist will coordinate the antimicrobial / microbiology ward rounds, liaise with microbiology and the infection prevention and control team with regards most appropriate treatment of infection and coordinate audits to assess compliance with the policy and Trust prescribing guidelines The microbiologists will carry out regular multi-disciplinary ward rounds with pharmacy with the aim of improving antimicrobial prescribing and providing interactive education on the wards The microbiology laboratory will deliver a timely, accurate, appropriate and efficient service The IPCT will work with Matrons, Clinical Directors, clinical leads, heads of specialties and infection control link persons to improve adherence to infection prevention and control guidelines and policies Results and actions from any audit of antimicrobial prescribing will be reported to the Director of Infection Prevention and Control via the Infection Prevention and Control Management Committee and Antimicrobial Management Group All staff have a duty of care to the patients and themselves to ensure they deliver high standards of infection control practice including antimicrobial prescribing practice at all times. Wherever there is deficiency in their knowledge or experience this must be highlighted to the department/ward manager who is responsible for ensuring the member of staff receives the appropriate training, education or advice Matron, Clinical Directors, clinical leads and heads of specialties have a duty of care to ensure that staff receive education on all aspects of infection prevention and control which relate to their workforce’s job 5. PROCESS 1. PATIENT SAFETY Antimicrobial prescribing within PHT is prudent, appropriate and safe for both the patient and the environment. Antimicrobials will be used wisely. Patients will not be exposed to unnecessary antimicrobial therapy. Antibiotics must not be started in the absence of clinical evidence of bacterial infection. 2. DOCUMENTATION OF CLINICAL NEED TO PRESCRIBE ANTIMICROBIALS The clinical indication, duration or review date, route of administration and dose all need to be clearly documented on the prescription chart and in the medical notes 3. CORRECT DOSING AND ADMINISTRATION Antimicrobials will be administered at the most appropriate dose for treatment of infection taking into account modifications required for renal and/or liver dysfunction. Antibacterials must be started within one hour if a patient is suspected as having severe sepsis or septic shock or neutropaenic sepsis. All aminoglycoside and glycopeptide antimicrobials will be administered and monitored according to local Trust guidelines. Antimicrobials will be administered via the most appropriate route for the clinical presentation. 4. MICROBIOLOGY SUPPORT FOR ANTIMICROBIAL PRESCRIBING Appropriate microbiological samples will be taken prior to the commencement of antimicrobial therapy. The results of these cultures will be used to rationalise the empirical prescription in the individual, to guide future empirical therapy advice and for surveillance purposes. Appropriate antimicrobial sensitivity testing will be Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 6 of 9 carried out by the laboratory on clinical specimens received. A range of sensitivities will be released allowing the clinician a reasonable choice of targeted antibiotic treatments. 5. REVIEW OF ANTIMICROBIAL PRESCRIPTIONS WITH CLEAR PRESCRIBING PLAN BY 48 HOURS By 48 hours a clear antimicrobial prescribing plan should document whether antimicrobial therapy is to continue, change, stop, switch or be delivered by OPAT, i.e. an antimicrobial prescribing decision must be made and documented in the clinical notes by 48 hours. This plan will be guided by clinical progress and results of investigations including blood and culture results. Intravenous to oral switch must be considered wherever possible so avoiding the risks associated with intravenous cannulation including iatrogenic bloodstream infection and thrombosis. 6. PREFERENTIAL USE OF NARROW SPECTRUM ANTIMICROBIALS Antimicrobial therapy should be targeted to treat the specific infection using as narrow-spectrum an antimicrobial agent as is possible. Certain broad spectrum or tertiary antibacterials will only be prescribed with microbiology approval (see appendix 1; Restricted antimicrobial agents). 7. APPROPRIATE DURATION OF THERAPY Antimicrobials will be prescribed for as short a time period as possible. The duration of antimicrobial therapy depends on the infecting organism(s), the site of the infection, the patient’s own immune response and other additional features such as surgical and medical interventions. Each antimicrobial prescription needs to be assessed on a daily basis and the review documented in the clinical notes. 8. AVAILABLE GUIDANCE FOR ANTIMICROBIAL PRESCRIBING Antimicrobials will be prescribed following referenced guidelines which are available to the prescriber at the point of care in electronic format. These guidelines will be evidence based and written by a clinician with expertise in the area with local epidemiological knowledge. Current guidelines available on the PHT intranet are listed in appendix 2. Each registered prescriber will be issued with a pocket guide for empirical antimicrobial prescribing at Trust induction or at mandatory annual Infection Prevention and Control updates, (see appendix 3). Further advice on antimicrobial prescribing can be obtained from the British National Formulary. 9. SUPPORT AND EDUCATION FOR MANAGEMENT OF INFECTION Antimicrobial prescribing is supported by regular (usually weekly) antimicrobial ward rounds carried out by microbiology in liaison with pharmacy across all acute clinical areas. Education to the junior doctors will be provided on these ward rounds. A regular program of infection updates is included in the F1/F2 junior doctor’s training. Education to senior clinicians will take place via core training programs and annual infection control updates. In addition, infection advice is available from a consultant microbiologist 24 hours a day, 7 days a week. Requirements for fulfilment of policy Sufficient numbers of qualified pharmacists to allow all prescription charts to be reviewed on a regular basis 1.0 WTE band 8a pharmacist(s) acting as the lead antimicrobial pharmacist(s) for the Trust Adequately resourced microbiology laboratory with quality assurance procedures in place. Sufficient numbers of microbiologists or infection specialists to allow regular antimicrobial ward rounds. Royal College of Pathologists guidance from 2001 states that for our current population (520,000) and renal specialist services there should be 4.0 WTE consultant microbiologists. This guidance predates the expansion of Infection Prevention targets. There are currently 3.45 WTE consultant microbiologists Adequately resourced infection prevention and control team to support education and surveillance on antimicrobial resistance and nosocomial infection. Access for all staff in all clinical areas to computer-based and paper-based up-to-date guidelines and current copies of the British National Formulary. Senior clinical support in all clinical areas to allow regular (mostly daily) review of all antimicrobial therapy Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 7 of 9 6. TRAINING REQUIREMENTS All antimicrobial prescribers need to familiarize themselves with the Antimicrobial prescribing guidelines available on the intranet at http://pharmweb/MedicinesInformation/Guidelines/alpha.aspx All new medical staff will receive antimicrobial prescribing guidance from the Trust’s antimicrobial pharmacists at induction and will be given an empirical antimicrobial prescribing guide as laminated card. All medical staff need to complete an annual update on infection prevention and control which includes emphasis on appropriate antimicrobial prescribing There is an electronic antimicrobial prescribing update available for all prescribers and all new medical staff. Anyone who fails to complete the mandatory training will be managed by their line manager in liaison with Human Resources using the Trust Capability Policy 7. REFERENCES AND ASSOCIATED DOCUMENTATION 1. Livermore DM. Has the era of untreatable infections arrived? J Antimicrob Chemother. 2009;64(Suppl 1):29-36 2. Hawkey, P., Jones, A. The Changing Epidemiology of Resistance. J Antimicrob Chemother. 2009; 64:Suppl 1:i3–10 3. Department of Health’s advisory committee on Antimicrobial Resistance and Healthcare associated Infection (ARHAI), Antimicrobial stewardship “Start smart, then focus”, November 2011 4. Davey, P., E. Brown, L. Fenelon, R. Finch, I. Gould, G. Hartman, A. Holmes, C. Ramsay, E. Taylor, M. Wilcox, and P. Wiffen. 2005. Interventions to improve antibiotic prescribing practices for hospital inpatients. Cochrane Database Syst. Rev.19:CD003543 5. Dellit TH, Owens RC, McGowan JE et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America Guidelines for Developing an Institutional Program to Enhance Antimicrobial Stewardship. Clin Infect Dis. 2007;44:159-77. 6. Department of Health Chief Medical Officer. Winning ways: Working together to reduce healthcare associated infection in England. London: Department of health, 2003. 7. World Health Organisation (2001). WHO Global Strategy for containment of antimicrobial resistance. WHO, Geneva, Switzerland. 8. Surviving Sepsis Campaign: International Guidelines for the Management of Severe Sepsis and Septic Shock 2012. Dellinger RP et al. and the surviving sepsis campaign guideline committee including the paediatric subgroup. Critical Care Medicine 2013; 41(2): 580-637 8. MONITORING COMPLIANCE WITH, AND THE EFFECTIVENESS OF, PROCEDURAL DOCUMENTS A minimum of 2 antimicrobial prescribing audits will be carried out each year under the supervision of the antibiotic pharmacist and the Consultant Microbiologists. Results of these audits will be reported to the Trust via the Infection Prevention and Control Management Committee and the Antimicrobial Management Group. An annual Trust wide point prevalence audit will be carried out by microbiology and pharmacy. Suggested audit targets are outlined below. 90-100% of antimicrobials prescribed are clinically warranted 90-100% of antimicrobial use is documented in the patient’s notes 90-100% of antimicrobial prescribing is in accordance with local guidelines 90-100% of antimicrobials prescribed are prescribed at the correct dose 90-100% of antimicrobials prescribed are prescribed via the most appropriate route with intravenous to oral switch following local guidance 90-100% of antimicrobials prescribed which require blood levels are monitored appropriately 0-10% of antimicrobials are prescribed for longer than is necessary 90-100% of patients and their prescription charts are reviewed daily by the clinical team 90-100% of health care workers have an annual infection control update including antimicrobial prescribing Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 8 of 9 Appendix 1: Antimicrobial agents restricted for consultant physician approval (within 24 hours) Ciprofloxacin (intravenous or oral) Ertapenem Meropenem Antimicrobial agents restricted for consultant microbiologist approval only Daptomycin Linezolid Temocillin Tigecycline Voriconazole Appendix 2: Current (2013) Portsmouth Hospitals NHS Trust antimicrobial therapy guidelines available on the intranet Antibiotic prophylaxis in surgery Antimicrobial guidance for the Intensive Care Unit Cellulitis and erysipelas Clostridium difficile management guideline Diabetic foot infection guidance Head and neck empirical antimicrobial guidelines for adults Infective endocarditis treatment in adults Intravenous vancomycin IV to oral switch Metronidazole compatibility with other IV antibiotics Neutropaenic sepsis in adults Once daily gentamicin administration in adults Pneumonia, community acquired Pneumonia, hospital acquired Pregnancy sepsis screening tool Prevention of sepsis in asplenic and hyposplenic adult patients Treatment of cellulitis Urinary tract infections Appendix 3: PHT empirical antimicrobial prescribing guide for adults admitted to general medical and surgical wards PHT empirical antimicrobial prescribing guideline for adults UTI Trimethoprim 200mg bd po (add once daily gentamicin if septic) Inf exac COPD Doxycycline 200mg od (2nd line amox 500mg tds po) CAP (mild-moderate) Amoxicillin 500mg-1g tds po OR Clarithromycin 500mg bd po CAP (severe, CURB-65 3) Benpen 2.4g stat then 1.2-2.4g qds iv + Doxycycline 200mg stat then od po/ ng OR Benpen 2.4g stat then 1.2-2.4g qds iv + iv Clarithromycin 500mg bd If penicillin allergic: Chloramphenicol iv 12.5mg/kg qds iv (max 1g qds) for 5/7 HAP (severe) Piperacillin/taz 4.5g tds iv OR Chloramphenicol*12.5mg/kg qds iv (max 1g qds) for 5/7 Cellulitis (severe) Fluclox 1g qds iv, (clindamycin* 300mg qds) Vancomycin if known MRSA +ve Bone / joint Flucloxacillin 2g qds iv OR (cefuroxime 1.5g tds iv)* GI / biliary sepsis Co-amoxiclav po/iv OR (cefuroxime 750mg tds iv +/- metronidazole 500mg tds*) iv C difficile Severe - vancomycin 125mg qds po. Non severe - metronidazole 400mg tds po Neutropenic sepsis Piperacillin/tazobactam 4.5g tds iv (Ceftazidime 1-2g tds iv*) Meningitis Ceftriaxone* 2g bd iv (+ aciclovir 10mg/kg tds iv if HSV encephalitis) SBP Piperacillin/taz 4.5g tds iv, (if pen allergic* use Cefotaxime 2g tds iv) *recommended for penicillin allergic patients, if severe or anaphylactic response contact micro. Portsmouth Hospitals NHS Trust Antimicrobial Prescribing Policy Version 6 Issue Date 4 March 2013 Review Date 1st January 2015 Page 9 of 9