Summary Sheet - Australian Commission on Safety and Quality in
advertisement
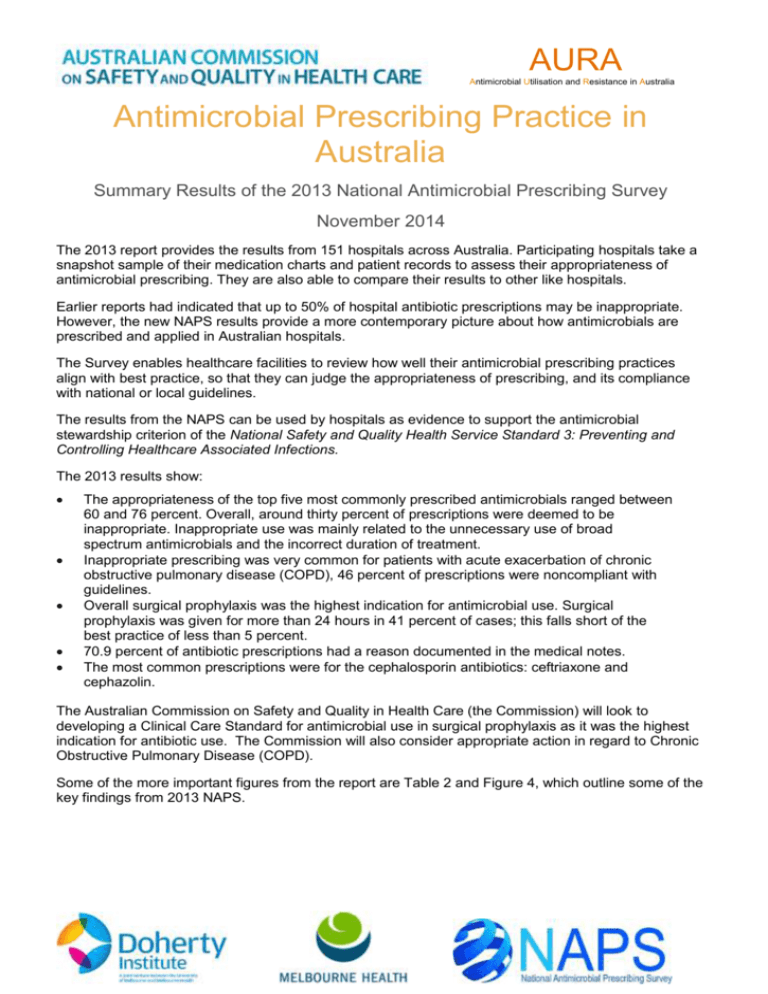
AURA Antimicrobial Utilisation and Resistance in Australia Antimicrobial Prescribing Practice in Australia Summary Results of the 2013 National Antimicrobial Prescribing Survey November 2014 The 2013 report provides the results from 151 hospitals across Australia. Participating hospitals take a snapshot sample of their medication charts and patient records to assess their appropriateness of antimicrobial prescribing. They are also able to compare their results to other like hospitals. Earlier reports had indicated that up to 50% of hospital antibiotic prescriptions may be inappropriate. However, the new NAPS results provide a more contemporary picture about how antimicrobials are prescribed and applied in Australian hospitals. The Survey enables healthcare facilities to review how well their antimicrobial prescribing practices align with best practice, so that they can judge the appropriateness of prescribing, and its compliance with national or local guidelines. The results from the NAPS can be used by hospitals as evidence to support the antimicrobial stewardship criterion of the National Safety and Quality Health Service Standard 3: Preventing and Controlling Healthcare Associated Infections. The 2013 results show: The appropriateness of the top five most commonly prescribed antimicrobials ranged between 60 and 76 percent. Overall, around thirty percent of prescriptions were deemed to be inappropriate. Inappropriate use was mainly related to the unnecessary use of broad spectrum antimicrobials and the incorrect duration of treatment. Inappropriate prescribing was very common for patients with acute exacerbation of chronic obstructive pulmonary disease (COPD), 46 percent of prescriptions were noncompliant with guidelines. Overall surgical prophylaxis was the highest indication for antimicrobial use. Surgical prophylaxis was given for more than 24 hours in 41 percent of cases; this falls short of the best practice of less than 5 percent. 70.9 percent of antibiotic prescriptions had a reason documented in the medical notes. The most common prescriptions were for the cephalosporin antibiotics: ceftriaxone and cephazolin. The Australian Commission on Safety and Quality in Health Care (the Commission) will look to developing a Clinical Care Standard for antimicrobial use in surgical prophylaxis as it was the highest indication for antibiotic use. The Commission will also consider appropriate action in regard to Chronic Obstructive Pulmonary Disease (COPD). Some of the more important figures from the report are Table 2 and Figure 4, which outline some of the key findings from 2013 NAPS. AURA Antimicrobial Utilisation and Resistance in Australia Figure 5 Top 20 most common indications Table 2 Results of key indicators for all contributing hospitals Key indicator % of total prescriptions % of total assessable prescriptionsa Indication documented in medical notes (best practice >95%) 70.9 – Surgical prophylaxis given for >24 hours (best practice <5%) 41.5b – Compliance with guidelines: Compliant with Therapeutic Guidelines: Antibiotic or endorsed local guidelines 59.7 72.2 Compliance with guidelines: Noncompliant 23.0 27.8 Compliance with guidelines: No guideline available 11.0 – Compliance with guidelines: Not assessable 6.3 – Appropriateness: Appropriate (optimal + adequate) 70.8 75.6 Appropriateness: Inappropriate (suboptimal + inadequate) 22.9 24.4 Appropriateness: Not assessable 6.3 – For the full Report, please visit http://www.safetyandquality.gov.au.