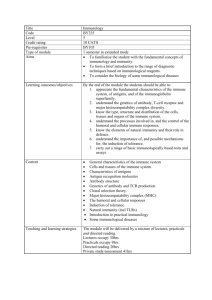
Immune System in Health and Disease
advertisement

IMMUNOLOGY AND PUBLIC HEALTH Background notes Introduction Mammals have well-developed immune systems. As a consequence of living in densely populated groups humans are particularly liable to transmitted diseases. To manage these hazards humans have developed public health measures and immunisation programmes. A key function of the immune system is to recogni se pathogens, some toxins and cancer cells as foreign and to create a response to them. The immune system may also produce allergic responses to harmless foreign materials. Defence responses include general non-cellular and cellular responses, including phagocytosis and natural killer cells. Key aspects of the specific cellular immune response include immune surveillance and clonal selection theory. Emphasis should be placed on the role of cytokines, antigenpresenting cells and memory cells in the function of T - and B-lymphocytes. Emphasis is placed on the control of infectious disease by public health measures. Control of transmission of infectious diseases depends on an understanding of disease biology and the epidemiology of disease. The principles of active immunisation and vaccination should be considered , using appropriate examples. A study of clinical trials for vaccines should be used to consider the design of such trials to ensure the elimination of bias, valid comparisons and minimisation of experimental error by using randomised, double-blind, placebo-controlled protocols. A study of herd immunity and public health policy allows aspects of population biology to be considered. Students should have the opportunity to consider evidence-based decision making on public health policy issues related to the challenges to disease control presented by antigenic variation (eg annual influenza vaccination programme) and pathogens that attack the immune system (eg HIV and tuberculosis). Students should already have a clear understanding of the following areas of content: defences against disease (phagocytosis, antibodies, vaccination) diseases (viruses, bacteria, fungi, parasit es) hygiene (personal, sexual, food, water). IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 1 IMMUNOLOGY AND PUBLIC HEALTH To introduce this topic, see the suggested activities in Lesson plan 1. Immune system in health and disease The human body has the capacity to protect itself against pathogens, some toxins and cancer cells through the immune system. (a) Non-specific defences (i) Physical and chemical defences Epithelial cells on the body surface and cavity linings form a physical barrier and produce secretions that defend against infection . The body’s first lines of defence against microbes are the barriers offered by surfaces exposed to the external environment. Very few microorganisms can penetrate the intact skin, and the various skin glands and tear glands all secrete antimicrobial chemicals. The mucus secreted by the epithelial linings of the respiratory and upper gastrointestinal tracts also contains antimicrobial chemicals, but more importantly, mucus is sticky. Particles that adhere to it are prevented from entering the blood. They are either swept by ciliary act ion up into the pharynx and then swallowed (as occurs in the upper respiratory tract) or phagocytised by macrophages in the various linings. Other specialised surface defences are the hairs at the entrance to the nose, the cough and sneeze reflexes, and the acid secretions of the stomach and uterus, which kill microbes. Finally, a major defence against infection is the many relatively innocuous microbes normally found on the skin and other linings exposed to the external environment. Through a variety of mechanisms, these microbes suppress the growth of other potentially more dangerous ones. Suggested activities – see Lesson plan 2. (ii) Inflammatory response Release of histamine by mast cells causes vasodilation and increased capillary permeability. The increased blood flow and the secretion of cytokines result in the accumulation of phagocytes and the delivery of antimicrobial proteins and clotting elements to the site of infection. 2 IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 IMMUNOLOGY AND PUBLIC HEALTH Inflammation is the body’s local response to infection or injury. Th e functions of inflammation are to destroy or inactivate foreign invaders and to set the stage for tissue repair. The steps and cells involved are detailed below: Mast cells Mast cells are part of a group of cells called leukocytes (white blood cells) that are found in almost all tissues and organs. Once activated , mast cells produce large quantities of histamine. Histamine dilates the surrounding capillaries and increases their permeability. Vasodilation and increased capillary permeability Vasodilation results in increased blood flow to the site of infection (accounting for the redness and heat associated with inflammation). The increased blood flow brings an increased number of leukocytes and proteins to the area. Increased permeability allows plasma proteins to gain entry from the blood to the site of infection. Secretion of cytokines The leukocytes that arrive at the site of infection secrete cytokines , which act as chemoattractants (chemotaxins). Chemotaxins stimulate the movement of phagocytes to the infected area. Phagocytosis Phagocytes arrive and begin to rid the area of bacteria. The phagocyte engulfs the bacterium in a process known as endocytosis. The bacterium is contained within an intracellular vesicle. The vesicle fuses with a lysosome and powerful enzymes digest the bacterium. The end products are then used by the cell or released by exocytosis. Complement Complement proteins are activated in response to infection. Activation of the first protein results in activation of a second prote in and so on in a cascade. The complement system consists of at least 30 distinct proteins and is extremely complex. Activation of the complement system amplifies the immune response – complement proteins can help to kill the microbe, stimulate vasodilation, increase permeability and aid phagocytosis. Tissue repair The final stage of inflammation is tissue repai r. Platelets form a plug to seal off the site of injury and clotting elements trigger the coagulation cascade, which strengthens the platelet plug. Finally, remodelling takes place as the healing process winds down. The final repair may be imperfect – this results in a scar. IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 3 IMMUNOLOGY AND PUBLIC HEALTH Suggested activities – see Lesson plan 3. (iii) Non-specific cellular responses A variety of specialised white blood cells provide protection against pathogens. Phagocytes recognise surface antigen molecules on pathogens and destroy them by phagocytosis. Natural killer (NK) cells induce the pathogen to produce self-destructive DNA enzymes in apoptosis. Phagocytes and NK cells release cytokines, which stimulate the specific immune response. On rare occasions pathogens break through the host’s physical and chemical defence mechanisms. The pathogen can then invade host tissues and begin to colonise and infect the host. It is at this point the immune system must become mobilised. The starting point for immunity (whether it is specific, non -specific, humoral or cell-mediated) is contact of a pathogen with a phagocyte. The primary function of a phagocyte is to engulf and destroy pat hogens and digest their remains. Phagocytes Phagocytes are found in the blood and in the tissues and they are motile. The phagoctyte recognises antigens on the surface of the pathogen, to which it then adheres. The membrane of the phagocyte engulfs the pathogen and pinches off to form an intracellular vesicle. This vesicle then fuses with a lysosome (a granular inclusion containing bactericidal substances such as lysozyme, hydrogen peroxide, proteases, phosphatases, nucleases and lipases). The toxic substances inside the lysosome are capable of killing and digesting the engulfed pathogen. Following digestion of the pathogen, the phagocyte releases a number of inflammatory mediators, some of which include cytokines. This results in a positive feedback loop, the cytokines recruiting more phagocytes to the area. Natural killer cells NK cells bind to virus-infected and cancer cells without specific recognition and kill them directly. They participate in antibody-dependent cellular cytotoxicity. NK cells constitute a distinct class of lymphocytes. Their major targets are virus-infected cells and cancer cells. They attack and kill these cells directly. NK cells are not specific – they are able to attack cells without any recognition of the specific pathogen involved. NK cells recognise ‘normal’ cells through their expression of Major Histocompatibility Complex (MHC) class 1 proteins. They recognise foreign cells by the absence of these proteins. The exact nature of NK cells and their method of action is unknown. 4 IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 IMMUNOLOGY AND PUBLIC HEALTH However, it is known that they kill cells by releasing small cytoplasmic granules of proteins called perforin and granzyme that cause the target cell to die by apoptosis (programmed cell death). The perforin is released in close proximity to the target cell and forms pores in the cell membrane, allowing granzymes to enter the cell. The granzymes stimulate the cell to produce enzymes that degrade the DNA of the cell, inducing apoptosis. As well as their role in non-specific immunity, phagocytes and NK cells also help to initiate the specific immune response. Following their action against the pathogen they secrete interleukins – cytokines that serve to stimulate the specific immune response through the activation of T cells. Suggested activities – see Lesson plan 4. (b) Specific cellular defences (i) Immune surveillance A range of types of white blood cell constantly circulate , monitoring the tissues. If tissues become damaged or invaded, a variety of cells release cytokines, which recruit specific white blood cells to the site of infection or tissue damage. Leukocytes (white blood cells) are the most numerous cells of the immune system. They are produced in the bone marrow and use the blood to transport themselves around the body – they are constantly on the lookout for microbes, pathogens, antigens etc. Leukocytes can leave the circulatory system and enter the tissues, where they function. If the tissues become damaged or invaded, leukocytes are capable of secreting over 100 different protein messengers known collectively as cytokines. Cytokines regulate host cell growth and function in both specific and non specific defences. Secretion of cytokines can trigger a number of responses. Some cytokines are chemokines (chemoattractants). Once secreted these chemokines attract phagocytes (non-specific) and T cells (specific) to the site of injury. This stimulates an inflammatory response as well as an immune response. Suggested activities – see Lesson plans 5 and 6. IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 5 IMMUNOLOGY AND PUBLIC HEALTH (ii) Clonal selection theory The body has a vast array of lymphocytes, each with a single type of membrane receptor specific for one antigen. When a receptor is activated by the binding of an antigen, the lymphocyte repeatedly divides , resulting in a clonal population of lymphocytes. Clonal selection theory states that each antigen-reactive B cell or T cell has only a single type of antigen-specific receptor on its surface. When stimulated by interaction with a specific antigen, each cell is capable of dividing, making a copy of itself. The anti gen-driven B and T cells continue to divide, resulting in multiple copies (or clones). Because of the infinite variety of antigens available, a large number of antigen -reactive cells are available in the body and each cell is capable of expanding into an a ntigenreactive clone. However, antigen-reactive cells must avoid interactions and subsequent immune reactions with self-antigens in the host. Suggested activities – see Lesson plan 7. (iii) T and B lymphocytes Lymphocytes respond specifically to antigens on foreign cells, cells infected by pathogens and toxins released by pathogens. Lymphocytes are the essential cells in specific immune defences. Lymphocytes must recognise the specific foreign matter to be attacked. Any foreign molecule that can trigger a specific immune response against itself or the cell bearing it is termed an antigen. T lymphocytes One group of T lymphocytes destroy infected cells by inducing apoptosis. Another group of T lymphocytes secrete cytokines that activate B lymphocytes and phagocytes. T lymphocytes mature in the thymus. T cells consist of two major subsets : cytotoxic T cells and helper T cells. Cytotoxic T cells are attack cells. They travel to the location of their target, bind to them via antigens on the target and, following activation, they directly kill the target via secreted chemicals. Responses mediated by cytotoxic T cells are directed against the body’s own cells , where these have become cancerous or infected. There are several mechanisms of target cell killing by activated cytotoxic T cells. One of the most important is by apoptosis. Apoptosis is programmed cell death – the infected cell is instructed to kill itself. Within the infected cell, endogenous enzymes are 6 IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 IMMUNOLOGY AND PUBLIC HEALTH activated that break down the cell nucleus and its DNA, as well as other cell organelles. Importantly, the cell membrane is not destroyed, so when the cell dies its contents are not dispersed. Instead the cell sends out chemical messengers that attract neighbouring phagocytic cells to engulf and d igest the dying cell. Helper T cells facilitate the activation of both B cells and cytotoxic T cells. Helper T cells must combine with an antigen and become activated. Once activated they secrete cytokines that act on B cells and cytotoxic T cells that have also bound to antigens. B cells and cytotoxic T cells cannot function properly unless they are stimulated by cytokines produced by helper T cells . B lymphocytes Each B lymphocyte clone produces a specific antibody molecule that will recognise a specific antigen surface molecule on a pathogen or a toxin. Antigen–antibody complexes may inactivate a pathogen or toxin or render it more susceptible to phagocytosis. In other cases the antigen–antibody complex stimulates a response that results in cell lysis. B cells mature in the bone marrow. All new generations of B cells are derived from and are identical to their parent cells – hence they are all clones. On activation, B cells differentiate into plasma cells, which secrete antibodies. The antibodies combine with a specific antigen and guide an attack that eliminates the antigens or the cells bearing them. The antibodies bind to the antigen on the surface of the cell, but they do not directly kill the cell . Instead, they link the target cell to the actual ki lling mechanism. Antibodies can act as opsonins – they can link a phagocyte to an antigen, which then triggers phagocytosis. In other cases, antibodies can activate the classical complement pathway. This results in the production of chemicals that make the cell membrane ‘leaky’, causing cell lysis. Antibody-mediated responses are the major defence against bacteria, viruses and other microbes in the extracellular fluid, and against toxic molecules . Suggested activities – see Lesson plans 8 and 9. Recognition of self and non-self T lymphocytes have specific surface proteins that allow them to distinguish between the surface molecules of the body’s own cells and cells with foreign molecules on their surface. Failure in regulation of the immune system leads to an immune response to self cells (autoimmune disease). Allergy is a hypersensitive response to an antigen that is normally harmless. IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 7 IMMUNOLOGY AND PUBLIC HEALTH While T cells are maturing, their antigen receptors are tested for potential self-reactivity. For the most part, T lymphocytes bearing receptors for molecules already present in the body are either rendered non -functional or are destroyed by apoptosis – thus the body normally has no mature lymphocytes that react against self components. The immune system exhibits self-tolerance. Failure of self-tolerance can lead to autoimmune disease. Major histocompatibility complex (MHC) are molecules that mark body cells as ‘self’. T lymphocytes have specific receptors that can recognise MHC and therefore recognise cells that belong to the body. Sometimes the body loses tolerance for self, this then leads to autoimmune disease. Autoimmune disease is caused by an inappropriate immune attack triggered by the body’s own proteins acting as antigens. The immune attack, mediated by auto-antibodies and self-reactive T cells, is directed specifically against the body’s own cells that contain these proteins. Allergy refers to diseases in which immune responses to environmental antigens cause inflammation and damage to the body itself. Antigens that cause allergies are called allergens. Most allergens are relatively or completely harmless: it is the immune response to them that causes damage. Allergy is a result of the immune system going wrong. Suggested activities – see Lesson plan 10. Antigen-presenting cells When pathogens infect tissue, some phagocytes capture the pathogen and display fragments of its antigens on their surface. These antigen -presenting cells activate the production of clones of T lymphocytes, which move to the site of infection under the direction of cytokines. B lymphocytes activated by antigen-presenting cells and T lymphocytes produce clone s of B lymphocytes that secrete antibodies into the lymph and blood , from where they make their way to the infected area. After a microbe or other non-cellular antigen has been phagocytosed by a macrophage it is partially broken down into smaller fragments . These fragments bind to MHC class II proteins, which are then transported to and displayed on the plasma membrane. The antigen fragments are presented to T lymphocytes (antigen presentation). The antigenic binding of the antigen presenting cell (APC) to the T lymphocyte causes the T lymphocyte to proliferate and differentiate into a clone of activated helper T cells . These secrete cytokines, which recruit more lymphocytes to the area of infection. The arriving lymphocytes secrete more cytokines which stimulate B lymphocytes to produce large quantities B lymphocyte clones, which produce 8 IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 IMMUNOLOGY AND PUBLIC HEALTH antibodies that are then secreted into the lymph and blood, making their way to the infected area. Memory cells (immunological memory) Some T and B lymphocytes produced in response to antigens by clonal selection survive long term as memory cells. A secondary exposure to the same antigen rapidly gives rise to a new clone of lymphocytes, producing a rapid and greater immunological response. Once a lymphocyte is activated to divide and differentiate it forms two clones of cells. One clone contains a large number of effector cells – short-lived cells that combat the antigen. The other clone consists of memory cells, long lived cells bearing receptors specific for the same antigen. This antigen driven cloning of lymphocytes is called clonal selection (see earlier). The primary immune response (the first time the body is exposed to an antigen) takes 10–17 days from initial exposure until selected lymphocytes generate the maximum effector cell response. During this time the effected individual may become ill. On re-exposure to the same antigen some time later , it takes only 2–7 days to produce a response of greater magnitude and which lasts for a prolonged period of time – this is the secondary immune response. Memory cells are poised to proliferate and differentiate rapidly when they meet the same antigen. The antibodies produced during the secondary immune response have a greater affinity for the antigen compared to those produced in the primary immune response. Suggested activities – see Lesson plan 11. IMMUNOLOGY AND PUBLIC HEALTH (H, HUMAN BIOLOGY) © Learning and Teaching Scotland 2011 9