Pharmacy Department – Medication Management
advertisement

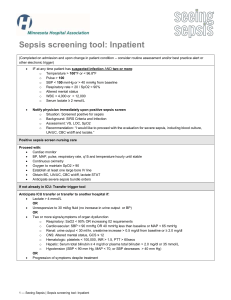
POLICY TITLE: Sepsis Bundle POLICY NUMBER: MANUAL NAME: Clinical Operations Addendum to Corporate Policy Form Available In I-REPP System SECTION (as applicable): Corporate Policies POLICY OWNER: Vice President Quality ORIGINATION DATE: 11/18/2015 FINAL APPROVAL DATE: 12/10/2015 POLICY: Early recognition and treatment for sepsis, severe sepsis and septic shock shall be accomplished through active surveillance screening using the protocols defined in this Sepsis Bundle. Treatment guidelines follow recommendations by the Surviving Sepsis Campaign, a workgroup of the Society for Critical Care Medicine and the European Society of Intensive Care Medicine. SCOPE: This sepsis bundle applies to all acute care facilities, for adult patients 18 years and older. DEFINITIONS: Surviving Sepsis Campaign: An international collaborative recommending resuscitation and management care bundles for the recognition and treatment of severe sepsis/septic shock. SIRS (Systemic inflammatory response syndrome): The clinical syndrome that results from a deregulated inflammatory response or to a noninfectious insult. Sepsis: SIRS that is secondary to infection that has been diagnosed clinically. Positive cultures add to the validity but are not required for the diagnosis. Severe Sepsis: Sepsis plus at least one sign of hypoperfusion or organ dysfunction, that is new, and not explained by other known etiology of organ dysfunction. Septic Shock: Severe sepsis associated with refractory hypotension (SBP<90) despite adequate fluid resuscitation and/or a serum lactate level > 4.0 mmol/L. Page 1 of 5 The electronic version of this policy is considered to be the controlled version. Printed copies are considered uncontrolled documents. Before using a printed copy, verify that it is the current version. Rapid Response Team: A team of qualified clinicians that respond to a perceived change in, or deterioration of, the condition of patients by bringing critical care expertise to the bedside. Presentation Time: Initial time of recognition of severe sepsis (SIRS and organ dysfunction). Emergency Department presentation is judged to be a patient’s triage time unless clinically evidenced otherwise. All other presentations rely on a time at which signs, symptoms, and laboratory findings are first consistent with the above definitions of severe sepsis/septic shock. PROCEDURE: I. Recognition A. Criteria: Adult Adult screening criteria and protocols are applied to patients admitted to adult inpatient units. Sepsis is defined as at least two of the following signs and symptoms, of the clinical syndrome referred to as Systemic Inflammatory Response Syndrome (SIRS) that are both present and new to the patient and there is suspicion of a new infection, but may not be limited to: 1. 2. 3. 4. 5. Hyperthermia >38.3°C (100.9° F) or Hypothermia <36°C (96.8° F) Acutely Altered Mental Status Tachycardia >90 beats per minute Tachypnea >20 breaths per minute Leukocytosis (>12,000 μL-1) or Leukopenia (<4,000 μL-1) or >10% bands on differential 6. Hyperglycemia (>140 mg/dl) in the absence of diabetes Severe Sepsis includes SIRS (from the list referenced under Sepsis above) and at least one of the following signs of hypoperfusion or organ dysfunction from the list below that is new and not explained by other known etiology of organ dysfunction, but may not be limited to: 1. 2. 3. 4. 5. 6. 7. 8. 9. Hypotension (SBP <90 or MAP <65), or a SBP decrease >40mmHg from baseline BP Lactate >2 mmol/L Areas of mottled skin or capillary refill >3 seconds Creatinine >2.0 mg/dl Platelet count <100,000/mm3 Acute renal failure or urine output <0.5 mL/kg/hr for at least 2 hours Hepatic dysfunction as evidenced by Bilirubin >2 mg/dL INR > 1.5 or a PTT / 60 sec. Acute lung injury in the absence of pneumonia as an infection source or ARDS in the presence of pneumonia Septic Shock is defined as severe sepsis associated with refractory hypotension (SBP<90) despite adequate fluid resuscitation and/or a serum lactate level >=4.0 mmol/L. Page 2 of 5 The electronic version of this policy is considered to be the controlled version. Printed copies are considered uncontrolled documents. Before using a printed copy, verify that it is the current version. II. Screening Process 1. In the Emergency Department: a. The Triage nurse shall assess all patients for possible sepsis and the sepsis screening tool shall be completed in the Electronic Medical Record (EMR). In addition to the documentation of the sepsis screening, the physician receives notification of a positive triage sepsis screen via the electronic triage note. 2. In the inpatient Units: a. Patients are screened for the risk of sepsis (including sepsis/severe sepsis) upon admission and every shift thereafter. Documentation of the sepsis screen shall be documented in the electronic medical record. b. If the patient meets criteria, the physician shall be notified of new findings and/or change in condition, as appropriate. c. The Rapid Response Team maybe initiated, as appropriate, for the evaluation for severe sepsis, and may evaluate for severe sepsis with other rapid response calls. III. Treatment A. Resuscitation: Three (3) Hour Bundle – The below actions are recommended by evidenced based practice to be taken within the first 3 hours of resuscitation upon initial recognition for adults. The clinician’s judgement shall determine the patient’s treatment plan. 1. Serum lactate measured within 3 hours of presentation. 2. Blood Cultures obtained prior to antibiotic administration to determine all potential site and source of infection. 3. Early and appropriate broad-spectrum antibiotic administration. (Timely reevaluation of antibiotic therapy based on causative agent and susceptibilities is recommended after initial administration of broad-spectrum antibiotics) 4. Initial fluid administration of 30 ml/kg crystalloid (0.9 Normal Saline Solution or Ringer’s Lactate (LR)for hypotension or lactate > 4 mmol/L. Six (6) Hour Bundle – The actions below are to be taken within the first 6 hours of resuscitation upon initial recognition for adults. Treatment will follow one of two tracks, invasive or non-invasive, based on the criticality and initial response to hemodynamic measures. The recommended bundle elements include: 1. Vasopressor therapy for hypotension that does not respond to initial fluid resuscitation, to maintain a mean arterial pressure (MAP) > 65 mmHg. 2. In the event of persistent hypotension after initial fluid administration (MAP < 65 mmHg) or if initial lactate was > 4 mmol/L, reassess volume status and tissue perfusion. 3. Document reassessment of volume status and tissue perfusion with either: a. Repeat focused exam (after initial fluid resuscitation) by a licensed independent practitioner including vital signs (including temperature), Page 3 of 5 The electronic version of this policy is considered to be the controlled version. Printed copies are considered uncontrolled documents. Before using a printed copy, verify that it is the current version. cardiopulmonary, capillary refill, peripheral pulse, and skin findings (color); b. Or two of the following: i. Measure CVP ii. Measure ScvO2 iii. Bedside cardiovascular ultrasound iv. Dynamic assessment of fluid responsiveness with passive leg raise or fluid challenge (documented by a licensed independent practitioner) 4. Re-measure lactate if initial lactate is elevated. B. Criteria for Invasive versus Noninvasive Protocol: 1. Invasive a. A central venous catheter capable of hemodynamic measuring may be inserted in a severely septic/septic shock patient in the first 6 hours after presentation if one or more of the below conditions are met*: 1. Patient exhibits persistent hypotension despite fluid resuscitation 2. Patient requires vasopressor therapy for hypotension 3. Inability to obtain adequate peripheral access in patient for fluid resuscitation, blood products, or medications. *For massive fluid resuscitation consider cordis. 2. Non-invasive a. Contraindications to the above criteria may include: 1. Patient is receiving comfort measures only 2. Patient refuses to give consent b. The trending of lactate levels to gauge fluid response is used with critical value alerts for lactates resulting >4 mmol/L. Serial trending (lactate clearance) within 2 hours of this critical result is suggested. IV. Education The stages of epsis/severe sepsis recognition and treatment training shall be provided in clinical (licensed personnel) orientation and annually, as needed. FORM REFERENCES: N/A REFERENCES: A randomized trial of protocol-based care for early septic shock. (2014). The New England Journal of Medicine, 370(18), 1683-1693. Retrieved from http://search.proquest.com/docview/1520423050?accountid=458 Dellinger, R. Phillip et al, Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Critical Care Medicine, Feb.2013, 41(2). Page 4 of 5 The electronic version of this policy is considered to be the controlled version. Printed copies are considered uncontrolled documents. Before using a printed copy, verify that it is the current version. Kumar, A. et al, Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock.Critical Care Medicine, June 2006, 34(6). Goal-directed resuscitation for patients with early septic shock. (2014). The New England Journal of Medicine, 371(16), 1496-1506. Retrieved from http://search.proquest.com/docview/1613090285?accountid=458 Goldstein, Brahm et al, International pediatric sepsis consensus conference: Definitions for sepsis and organ dysfunction in pediatrics. Pediatric Critical Care Medicine, 2005, 6(1). No.1. Mouncey, P. R., Osborn, T. M., Power, G. S., Harrison, D. A., Sadique, M. Z., Grieve, R. D., . . . Rowan, K. M. (2015). Trial of early, goal-directed resuscitation for septic shock. The New England Journal of Medicine, 372(14), 1301-1311. Retrieved from http://search.proquest.com/docview/1669475971?accountid=458 Rivers, E., Nguyen, B., Havstad, S., et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345:1368-1377 Surviving Sepsis Campaign; Updated Bundles in Response to New Evidence. 2015. www.survivingsepsis.org/sitecollectiondocuments/ss_bundle.pdf Review/Revised Date: Title: Description of Change or Location of Change in Document: 11/18/2015 VP Quality New sepsis bundle. Page 5 of 5 The electronic version of this policy is considered to be the controlled version. Printed copies are considered uncontrolled documents. Before using a printed copy, verify that it is the current version.