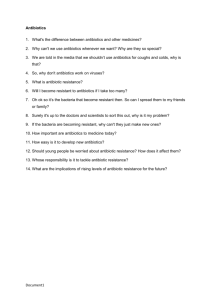
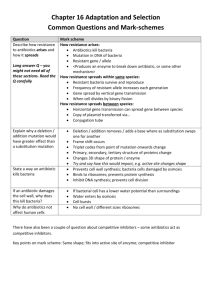
Antimicrobial Use and Resistence/Vaccination
advertisement

Antibiotic Resistance And Vaccines Marilyn C. Roberts PhD Professor marilynr@u.washington.edu Antibiotic Resistant Microbes Become an issue over the last 30 years Alternatives Prior to Antibiotics (pre-1950) 1. Vaccines 2. Antisera therapy 3. Phage therapy 4. Surgery (M. tuberculosis) 5. Herbal medicine 6. Food (Chicken soup) 7. Behavioral changes (quarantine) 8. Probiotics- use living microbes to compete with the potential Pathogens; 1950’s neonatal wards painted belly buttons with nonpathogenic S. aureus to protect against virulent strains WHY ANTIBIOTIC THERAPY FAILS 1. Patient does not comply with therapy- longer therapy harder Mycobacterium diseases 2. Inappropriate antibiotic prescribed Antibiotics for viral infection; Gram-positive antibiotics for Gramnegative diseases 3. Antibiotic not given in correct dose or taken long enough 4*. Pathogen is resistant to therapy 5. Patient is immunocompromised-major issue in hospitals today 1. Antibiotic resistant bacteria is a product of antibiotic use over the last 50 years 2. Shortly after introduction of penicillin (1945) first resistant staphylococci cultured 3. Today some multi-drug resistant pathogens have few or no available antibiotics for use-return to “the pre-antibiotic age” a) Staphylococcus aureus - vancomycin b) Enterococcus spp. c) Streptococcus pneumoniae d) Plasmodium spp. [malaria] 4. Few new agents becoming available for clinical use - most are modification of current drugs not new classes of agents - easier and faster for bacteria to become resistant 5. “Simplest way to enhance a bacterial bioweapon is to make it resistant to antibiotics” Nature 411:232, 2001 6. Technology available for most biological agents of bioweapon potential 7. Russians reportedly made Y. pestis resistant to 16 different antibiotics doxycycline therapy of choice - naturally resistant strains have been isolated 8. Clostridium spp. (toxin producers) resistance genes to variety of drugs used for therapy already in the genus - easy to transfer to toxin producer(s) of interest Antibiotic Targets 1. Bacteria usually structurally different than man with different biological pathways, enzymes, and nutritional requirements 2. Biological pathways, enzymes and nutritional requirements may or may not be different in virus, fungi, yeast, parasite 3. Antibiotics (Bacteria) usually have minimal affect on host, while anti-infective for treatment of virus, fungi, yeast, parasites therapy may impact the host to varying degrees 4. Antibiotics and anti-infectives often work directly on the pathways which produce DNA, RNA, protein, cell wall, other microbial pathways 5. Bacteriostatic: inhibits bacterial growth without killing in vitro 6. Bactericidal: kills in vitro 7. In vivo antibiotics/anti-infectives work with the host immune system to stop infection CAN NOT CURE INFECTION ALONE Resistance: Organisms have acquired the ability to grow on high levels of drug to which it was originally susceptible a) Usually only some strains of a group are resistant not all members b) Early strains are susceptible, recent strains are resistant Innate Resistance: All members including strains isolated in 1940-50’s or 1800’s are resistant Reason for Resistance: a) Lack target - no cell wall; innately resistant to penicillin; lack pathway b) Target is modified to prevent antibiotic from working- A2058 is another base in 23S rRNA- innately resistant to macrolides; resistance to antiviral agents c) Innate efflux pumps; drug is blocked from entering cell or increased export of the drug so does not achieve adequate internal concentration Resistance 1. Virtually all pathogens (bacterial, viral, fungal, parasite and cancer) will develop resistance to therapies 2. All pathogens develop resistance by mutation of innate host machinery 3. Bacteria also develop resistance by acquisition of new genes on mobile elements (plasmids, transposons, conjugative transposons, integrons) or acquisition of pieces of genes to create mosaics a) Eukaryotic pathogens and man also carry mobile elements but these have not been associated with increased drug resistance 4. Most bacterial resistance of clinical significance is due to acquisition a) Lateral DNA exchange is why resistance is able to move quickly through a bacterial population b) Allows unrelated bacteria to acquire resistance genes c) Allows multiple resistance genes and /or others genes [toxins, virulence factors, heavy metal resistance] packaged and move as a single unit Antibiotic Resistant Bacteria Treatment of multidrug resistant MDRTB: 10 times more costly vs susceptible NY City spent ~$1 billion MDRTB control during the 1990’s Multidrug resistant TB [MDRTB] Short course 1st therapy cure rates 5%-60% 2nd therapy cure rates 48%->80%: death rates: 0-37%, < 89% for HIV + pts Hospital stays; MRSA disease 1.3 times longer Treatment of MRSA $6,000-$30,000 more than treatment of MSSA Treatment of multidrug resistant Gram-negative infections 2.7 times more costly vs susceptible Hospital stays; resistant Gram-negative disease 1.7-2.6 times longer than susceptible disease Generally resistant bacteria are not more virulent but disease course acts as though no therapy provided when antibiotics are used that the microbe is resistant to Plasmids, Transposons, Conjugative transposons, Integrons 1. These elements can exchange genes resulting in antibiotic resistance gene reassortment and linkages a) One plasmid can carry multiple different antibiotic resistances genes in various combinations, toxins and virulence factors b) Same is true for transposons, conjugative transposons & integrons c) Many have hotspot for recombination so collect these genes d) Allow resistance genes to be maintained in a population Still see resistance to chloramphenicol when the antibiotic has not been used in the US for 30 years e) Join virulence factors and antibiotic resistance genes in 1 element create “super bug” JAMA Oct 2007 15:1763; estimate 94,360 MRSA infections in 2005 in USA with 13.7% community associated; number of deaths ~18,000 more than AIDS death in US for 2005: MRSA is now in both the hospital and the community Community MRSA has more virulence factors so is able to infect all ages groups regardless of their medical status The same class of antibiotics are used for food production and human medicine in N. America Share resistant bacteria and resistance genes between food animals and man Antibiotic resistant bacteria develop, both potential pathogens and commensals, in the animal/plants, local environment surrounding community, and can contaminate human and animal food in multiple ways Transgenic plants may carry viable antibiotic resistance genes which could possibly transfer to human/animal bacteria Once an antibiotic resistance gene is acquired by a bacterium it has the potential to transferred throughout the bacterial world What antibiotics are used in food production? Penicillins Tetracyclines Macrolides Lincomycins Bacitracin Virginiamycin Aminoglycosides Sulfonamides Streptomycins Many of these drugs can not be easily washed off by the consumer Apples from Mexico have gentamicin impossible to wash off and the flesh is contaminated as the skin is peeled Prawns from SE Asia grown in soup of antibiotics: prawns often have antibiotics in their flesh which may be destroyed with cooking Potential Spread from Food to Man Some probiotic Lactobacillus spp. used in food production and starter cultures are antibiotic resistant and carry acquired genes that are on mobile elements Various studies have shown that resistant animal bacteria such as VRE can become established in man and/or the complete mobile elements and/or the antibiotic resistance genes can become established in human isolates Antibiotic residues on food may select for resistant bacteria directly in man Commensal and environmental bacteria exposed to antibiotics will acquire resistance genes; become a reservoir for these genes and transfer them to pathogens/opportunists in their ecosystem Commensal and environmental population become stably resistant: common in environments that continually use antibiotics Commensal and environmental population may maintain antibiotic resistant population even when antibiotics are removed Bacterial populations exposed to antibiotics for extended time and then removed rarely return to baseline susceptibility: multiple reasons FUTURE 1. If there is no change we will have diseases which are no longer treatable with available antibiotics a) Already happens in much of developing world because of cost b) In US occurs if patient is poor, may not be able to get therapy needed 2. Education of the public and clinicians on appropriate use a) This summer a virus went around many got antibiotics needlessly b) Reduce use in pediatric population c) Reduce inappropriate use in hospital, community and agriculture - all 3 are linked 3. Cost issues with newest antibiotics - need to be affordable in all parts of the world Immunization/ Vaccines Principle of Vaccination Immunization [Vaccination] is a way to trigger the immune system and prevent serious, life-threatening diseases Mimics protection that occurs during natural disease without risk of disease Aim: Individual will develop immunity and immunologic memory similar to natural infection without risk of infection Antigen: A live microbe or inactive substance from microbe (protein, polysaccharide capsule) capable of trigger immune system Live attenuated (reduced virulence) bacteria/virus Inactivated whole [bacteria/virus]; specific component [protein-based sub-unit, or inactive toxin (toxoid); polysaccharide-based] Antibody: Protein molecules (immunoglobulin) produced by B lymphocytes in response to antigen in the vaccine Disadvantages of live attenuated vaccines Severe reactions possible Interference from circulating antibody Unstable, may have to be stored cold May cause disease (live polio vaccine) May gave false positive test (BCG vaccination; + skin TB test) Disadvantages of component vaccines Generally not as effective as live vaccines Generally require 3-5 doses Antibody titer diminishes with time Possibly variation of antigen with each batch of vaccine made Polysaccharide vaccines are not consistently immunogenic in children <2 years of age Some polysaccharides have proven impossible to use as antigen No available vaccine for N. meningitidis type B after 30 years of work Polysaccharide vaccines usually mixed with protein to increase immunogenic properties Types of Immunity Active Immunity Passive Immunity Protection by persons’ own immune system Protection transferred from from another person/animal Transplacental from mom to fetus Usually permanent Temporary protection May wane in old age Used for prevention after exposure to disease tetanus, rabies Current Vaccines Available Viral Diseases Bacterial Diseases Measles Mumps Rubella (German measles) Polio Pertussis* (whooping cough) Diphtheria* Tetanus* Haemophilus influenzae type b [Hib] Pneumococcal (S. pneumoniae) Influenza (flu) Hepatitis A, B Varicella (chickenpox) Human papillomavirus (HPV) * Rotavirus toxin disease No Vaccines Available Viral Diseases Bacterial Diseases HIV Hepatitis C Staphylococcus aureus MRSA E. coli O157:H7 Sexually transmitted diseases Today From 0-5 years of age ~150 vaccine shots given In addition to the antigen vaccines have preservatives (ethylmercury) to keep the vaccine sterile; stabilizers to protect composition of the vaccine and adjuvants which increase the ability to respond to the vaccine Some additives can cause redness and/or soreness on the skin where the vaccination has been given Today, with the exception of some flu vaccines, no vaccines used in the U.S. to protect preschool-aged children against 12 infectious diseases contain ethylmercury (thimerosal) as a preservative Controversy over whether ethylmercury in the MMR measles, mumps rubella) vaccine causes autism: No scientific data to support this claim Some people are not vaccinating their children because of this concern or for religious reasons Takes a long time once new vaccine is put in place to find out if There are side effects and/or if immunity is life long Disease 2000 % change 31,054 1 -99 Measles 390,852 86 -99 Mumps 21,342 338 -99 Pertussis 117,998 7,867 -93 Polio (wild) 4,953 0 -100 Rubella 9,941 176 -98 Cong. Rubella Synd. 19,177 9 -99 1,314 35 -97 24,856 112 -99 566,706 8,624 -98 Diphtheria Tetanus Invasive Hib Disease Total Pre-vaccine Era* Vaccine Adverse Events 0 13,497 What We As Individuals Can Do 1. Stress good hygiene at all times, home, work, community 2. Hand washing, appropriate food preparation, stay home when sick 3. Comply with prescription when provided 4. Do not ask for antibiotics 5. Check where food is coming from- do not buy if antibiotics are being used: much of the imported shell fish and fish use lots of antibiotics Domestic animal production antibiotics use-varies by state 6. Become an educated consumer 7. Get your vaccines, as well as, your children and pets as recommended