P72 IL-17-/- mice are protected from nephrotoxic nephritis and are
advertisement

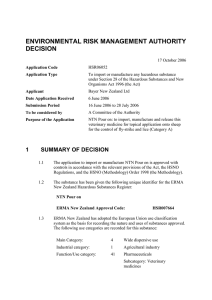
P72 IL-17-/- MICE ARE PROTECTED FROM NEPHROTOXIC NEPHRITIS AND ARE RESISTANT TO DISEASE INDUCTION BY ADOPTIVE CELL TRANSFER Hamour, S1, Cook, T1, Iwakura, Y2, Pusey, C1, Salama, A1 1 Imperial College Kidney and Transplant Institute, London, 2Centre for Experimental Medicine, University of Tokyo INTRODUCTION: Accelerated nephrotoxic nephritis (NTN) is a well-established animal model of immune-complex mediated glomerulonephritis. Th17 cells are a distinct lineage of CD4+ T-helper cells characterised by the production of IL-17, implicated in autoimmunity. This group and others have previously shown that IL-17-/- mice are protected from NTN. Here we show that IL-17-/- mice remain resistant to disease even following adoptive transfer with wild-type (WT) splenocytes or T cells. METHODS: Standard protocol for induction of accelerated NTN was followed. From WT or IL-17-/animals we isolated and transferred 8, 12 or 18 million splenocytes; 3 or 5 million purified T cells or 8 million non-T cells into WT and IL-17-/- animals undergoing induction of NTN. Cells were transferred on the same day as pre-immunisation with sheep IgG/CFA or following isolation from pre-immunised animals, two days prior to NTS injection. Purity of cell fractions was confirmed by FACS. Cell fractions were labelled with PKH26 red fluorescent dye for in vivo tracking. RESULTS: IL-17-/- mice were significantly protected from NTN as demonstrated by preserved renal function, minimal proteinuria(Figure) and diminished glomerular thrombosis. Following adoptive transfer of WT cells, PKH26-labelled cells were demonstrable in the kidney of IL-17-/- mice 2 weeks after cell transfer confirming that cells were viable and had trafficked to the kidney. Despite high numbers of cells transferred, IL-17-/- animals remained significantly resistant to NTN with preserved renal function, less proteinuria (Figure) and less glomerular thrombosis than WT animals receiving similar WT cell transfer. Moreover, transfer of 3x106 IL-17-/- T cells into WT animals conferred no protection from disease, suggesting that a regulatory T cell population was not responsible. 45 40 35 30 25 20 15 10 5 0 10.0 serum urea mmol/L 7.5 5.0 2.5 *** 0.0 WT IL-17-/- n=7 n=9 * * 6 5 4 3 2 1 20 10 /ls to to IL -1 7- IL -1 7/- IL -1 7/to ce l no nT T T ce lls W T T W W en oc yt es sp le T W W T W no n T T T ce no cy t lls es to to IL 17 W T -/- -/IL 17 to ce l te s oc y sp le n T W ls to te s to IL 17 W -/- T 0 oc y sp le n T IL17-/- n=10 30 0 W WT n=8 40 serum urea mmol/24h proteinuria mg/24h 7 ** sp l Proteinuria mg/24hrs 12.5 CONCLUSIONS: IL-17-/- mice are resistant to induction of NTN and remain protected despite adoptive transfer of WT splenocytes, purified WT T cells or non-T cell fractions. These data suggest that there may be other intrinsic mechanisms of disease protection, unrelated to Th17 cell induction. Further investigation is underway to define the mechanisms by which this protection is mediated.