Neuromuscular and Neurodegenerative Disorders
advertisement

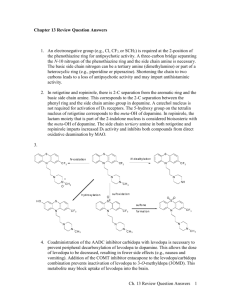
Chapter 11: Drugs Used to Treat Neuromuscular Disorders Case Study from 6th Edition ST is a 68 yo female who traded in her stressful job as an academic administrator at a major academic health center for the relaxed life of Southern California. Heading to “wine country” with her cats, retirement funds and a few family heirlooms, she purposefully sought a new life, making new friends and doing the things she loves most. She’s been very politically and culturally active in her community, and thoroughly enjoys her job as the social events planner at a small, family-owned winery that is just now beginning to gain regional notoriety. Attendance at her nightly “wine and cheese” gatherings have increased dramatically over the past year, giving ST a chance to network with clients and showcase the high quality of her employer’s “vino”. Life seemed perfect until a diagnosis of Parkinson’s disease was made three months ago. ST’s symptoms are characteristic of this dopamine deficiency disorder, and include rigidity, difficulty speaking and slowed movements. She is still able to function at work, but obviously worried about what the future holds. She began levodopa therapy immediately (400 mg twice a day) but is struggling to cope with drug-induced nausea and vomiting severe enough to limit her usually passionate involvement with a local Parkinson’s research advocacy group. In addition, while previously normotensive, she has experienced an increase in blood pressure that is now being treated with a thiazide diuretic. You meet up with ST at a wine-tasting event at the vineyard and, in a private moment, she asks for your professional advice and counsel. Consider the structure of the compounds drawn below and decide which might benefit this patient. Cl NH 2 CH2 CH2 NH NH2 HO C CH2 COOH HO OH CH2 CH Levodopa CH2 NH2 CH2 O HO C 3H 7 3 N 2 H CH2 + H3 C 1 N CH 2 - N H + N C 3H 7 Cl - CH3 4 OH 5 C CH 3 COOH Identify the therapeutic problem(s) where the pharmacist's intervention may benefit the patient. ST is facing a chronic and debilitating disease for which there is currently no known cure. She is on the “gold standard” anti-Parkinson’s therapy, levodopa, but experiencing side effects at a level sufficient to interfere with her quality of life. ST is on dopamine replacement monotherapy. The current standard of care attempts to maximize central dopamine augmentation by inhibiting premature degradation of its biochemical precursor, levodopa, in the periphery. This is done through combination therapy with levodopa and a dopa decarboxylase inhibitor. Levodopa, rather than dopamine, is the neurotransmitter replacement drug of choice because of its lower pKa (which translates into a higher u/i ratio at pH 7.4) and its ability to take advantage of amino acid transporting proteins for entry into the CNS. Dopamine cannot effectively cross the blood brain barrier if administered peripherally. Identify and prioritize the patient specific factors that must be considered to achieve the desired therapeutic outcomes. ST is experiencing significant nausea and vomiting from her levodopa therapy. Dopamine liberated from levodopa by peripheral dopa decarboxylase enzymes is stimulating the chemoreceptor trigger zone (CTZ) in the brainstem and directly irritating the GI tract. ST’s blood pressure is elevated as a result of peripherally-generated dopamine interacting with adrenoceptors in blood vessels (1, leading to vasoconstriction) and heart (1, leading to an increase in heart rate and force of contraction). ST’s job involves the consumption of wine and, often, cheese. ST is only 68 years old and theoretically has many years of life ahead of her. It is important to make those years of the highest possible quality by appropriately managing her Parkinson’s disease. Conduct a thorough and mechanistically oriented structure-activity analysis of all structures provided in the case. Levodopa is administered with the intent that it distribute intact to the brain where it can undergo decarboxylation to dopamine by central dopamine decarboxylase enzymes. Only after biotransformation to dopamine is this drug able to stimulate the central dopamine receptors that have been deprived of endogenous transmitter through the disease-induced destruction of dopaminergic nerve terminals. Dopa decarboxylase enzymes are also plentiful in the periphery and prematurely convert a large percentage of the levodopa dose to dopamine before it ever has a chance to reach central sites of action. As previously noted, dopamine generated in the periphery is unable to distribute to the CNS and the therapeutic effect in the treatment of Parkinson’s disease will be lost. Unless peripheral decarboxylase enzymes are inhibited, large doses of levodopa must be administered to ensure that therapeutic concentrations are achieved in brain. The high levels of dopamine generated in the periphery as a result of these augmented doses are responsible for the side effects experienced by ST (nausea, vomiting, hypertension). Compound 1 is an aralkylhydrazine that competes with catecholamine-based neurotransmitters (including dopamine) for access to monoamine oxidase (MAO) enzymes. MAO inactivates endogenous neurotransmitters and some xenobiotics through oxidative deamination, the first step of which is hydroxylation of an unsubstituted (methylene) -carbon to form an unstable carbinolamine. The carbinolamine intermediate rapidly degrades to release ammonia and an aldehyde metabolite. Compound 1, being a hydrazine, has no -carbon atom and thus, once bound to the enzyme through its terminal amine and phenyl ring, cannot be hydroxylated. Rather, the drug oxidizes to a reactive diazine that loses N2 and generates a highly destructive benzyl radical which inactivates the enzyme. Potent MAO inhibition in aralkylhydrazines demands an unsubstituted phenyl ring and a 2-3 carbon chain between phenyl ring and terminal nitrogen. Compound 1 is a nonspecific MAO antagonist, meaning it irreversibly inactivates both MAO-A and MAO-B. MAO-A is involved in metabolizing monoamines in foodstuffs (e.g., tryamine found in wine, cheese, beer, herring, etc.), as well as endogenous neurotransmitters like epinephrine and it nor derivative. MAO-B, on the other hand, metabolizes endogenous phenethylamines and dopamine, but not vasoactive amines found in foods. Compound 2 is a -aminopropanol substituted at the (carbinol) carbon with two cyclic hydrocarbon substituents. This is one structural prototype for antimuscarinic action (the others are aminoalkyl ethers and aminoalkyl esters). The amino nitrogen, in cationic form, anchors the drug to the G-protein coupled muscarinic receptor, and the “bulky” hydrocarbon ring systems both increase affinity for the receptor protein over the acetylcholine transmitter (a slender structure with a terminal methyl group) and provide steric hindrance to competition from the endogenous agonist. The terminal OH group is also believed to enhance affinity for the muscarinic receptor through hydrogen bonding. Aminoalcohol antimuscarinics can be either protonated tertiary amines or quaternary amines. The protonated tertiary amines are in equilibrium with their unionized free base forms at pH 7.4 and, therefore, have the ability to penetrate into the CNS. While their efficacy in Parkinson’s disease can be debated, they are sometimes used to provide a better balance of dopamine and acetylcholine receptor stimulation in the brains of Parkinson’s patients. The commonly observed peripheral side effects of dry mouth, blurred vision, urinary retention and constipation are, at best, annoying while the central effects of sedation, ataxia and potential hallucinogenic or delusional thinking can be use-limiting. Quaternary amine antimuscarinics are fully cationic at all pH values and cannot penetrate the blood brain barrier. They are, however, very effective peripheral agents, and are often used to treat overactive bladder (antispasmotic) or COPD (bronchodilation). Compound 3 has a “phenethylamine” pharmacophore buried in its structure which provides access to dopamine receptors. The tertiary amine is able to penetrate the blood brain barrier to reach central sites of action, and dopamine receptor agonism results. While the unionized amine is required for distribution to the CNS, the cationic amine is essential for anchoring the drug to the G-protein coupled dopamine receptor. The dihydroindol-2-one aromatic moiety provides access to the D2 and D3 subtypes but does not permit stimulation of other catcholaminergic receptors (e.g., , ). As dopamine agonists, molecules like Compound 3 can directly irritate the GI tract and stimulate dopamine receptors in the CTZ, leading to significant nausea and vomiting. Compound 4 is an N-methyl-4-phenyl-tetrahydropyridine structure known as MPTP. This chemical is a byproduct of the clandestine synthesis of a highly addicting opioid known chemically as 4-hydroxy-N-methyl-4-phenylpiperidine propionate ester (MPPP). If this ester hydrolyzes, which happens often during synthesis and work-up, it forms a tertiary alcohol which readily dehydrates to form this highly neurotoxic substance. Once transported into the brain, MPTP oxidizes to a quaternary dihydropyridine structure (N-methyl-4-phenyl-5,6-dihydropyridine or MPP+) that is trapped in the CNS and destroys dopaminergic neurons in the substantia nigra. The signs and symptoms of Parkinson’s disease result. O O N C CH2 CH3 C2H2 COOH hydrolysis CH3 MPPP ("synthetic heroin") OH H2O N CH3 dehydration N CH3 4 oxidation N + CH3 MPP+ (trapped in CNS) Compound 5 differs from levodopa only by the presence of an -CH3 group. While this destroys affinity for dopamine receptors, the compound retains high affinity for peripheral dopa decarboxylase enzymes. With the peripheral dopa decarboxylase enzymes tightly bound to Compound 5, levodopa can escape their metabolic action, allowing a greater percentage of the dose to reach the brain and undergo the desired decarboxylation reaction right at the site of action. Importantly, central dopa decarboyxlase enzymes are fully operational since Compound 5 does not distrtibute and is not transported to the CNS. Evaluate the SAR findings against the patient specific factors and desired therapeutic outcomes and make a therapeutic decision. Compound 1 (phenelzine) would be dangerous to use in this patient, particularly with the likelihood of her consuming wine and cheese on a regular basis. The inhibition of MAO-B would be desirable, as it would attenuate the inactivating metabolism of dopamine in central synapses, but the inhibition of MAO-A could lead to a hypertensive crisis, especially if large amounts of tyramine are consumed. Tyramine is a highly vasoactive amine and, if it is allowed to persist due to a loss of its inactivating MAO enzyme, it will increase blood pressure to potentially fatal levels. The half-life of the endogenous vasopressor neurotransmitter norepinephrine would also be extended through the inhibition of MAO-A and –B, so the risk of hypertension is significant even without the added impact of exogenous tyramine. With the consumption of tyramine-rich foods, pathological hypertension would be essentially guaranteed. Compound 2 (the quaternary analog of the antimuscarinic trihexyphenidyl) would do no good in a Parkinson’s patient since it would be unable to cross the blood brain barrier and, therefore, could not decrease cholinergic activity in the CNS. The tertiary analog might have had some value, although clinicians debate risk:benefit ratio of antimuscarinic therapy in Parkinson’s disease. The value of compound 3 (ropinirole) might also be debated in ST’s case. As a centrally active dopamine receptor agonist, it could take the place of levodopagenerated dopamine, and might be a good alternative therapy if the extent of neurodegeneration progresses to where ST can no longer decarboxylate levodopa. Dopamine agonists like ropinirole are sometimes used in combination with levodopa, allowing a lower dose of the latter compound with, hopefully, fewer side effects. However, the levodopa side effects most troubling to ST (nausea and vomiting) are also commonly experienced with ropinirole. In addition, patients on ropinirole can experience excessive daytime drowsiness, and can fall asleep without warning while engaged in normal daytime activities. Administering compound 4 (MPTP) would be an invitation to a malpractice lawsuit and a jail sentence. This neurotoxic substance, generated from the clandestine synthesis of a narcotic, would worsen ST’s Parkinson’s disease, and could prove fatal. Compound 5 (carbidopa) should be added to ST’s levodopa regimen ASAP. This peripheral dopa decarboxylase inhibitor would allow for a significant reduction in the levodopa dose and should decrease the extent and severity of the adverse effects this patient is experiencing. Counsel your patient ST should be told how the actions of carbidopa can help decrease the side effects of levodopa therapy, and that a single medication is available that contains both drugs in an appropriate ratio (1:10 carbidopa:levodopa). Carbidopa can also be administered separately (which permits titration to an optimal patient-specific ratio), but should be taken at the same time as levodopa. ST should be told to take her first dose of carbidopa (or the carbidopa:leovopa combination medication) no sooner than 8-12 hours after her last dose of levodopa, and informed that her urine may be darker than usual. ST should be warned that she might experience orthostatic hypotension when carbidopa is added to her regimen. She should take appropriate precautions when rising from a sitting position until she knows how she will respond to this new therapy. You may want to decrease the dose of the thiazide as ST begins carbidopa therapy, and assess need for continued antihypertensive therapy after she has been stabilized on the new combination antiParkinson’s regimen. If ropinerole is added to the regimen, ST must be warned about its sedating potential, and to exercise extreme caution until she knows how she will respond. As noted, patients fully engaged in the activities of daily living (including driving a car) can fall asleep without warning. This potential adverse effect is very serious, and can occur long after therapy is initiated. ST should definitely avoid other CNS depressants, including alcohol. She should, however, take this medication with food to avoid potential GI distress. ST should be asked to monitor the extent of nausea and vomiting she experiences on this therapy so it can be determined if it is having a beneficial effect. As with carbidopa, postural hypotension is possible and appropriate precautions should be taken. She should promptly report any visual, auditory or sensory hallucinations or worsening of Parkinson’s symptoms to her physician.




![[1] Edit the following paragraph. Add 4 prepositions, 2 periods](http://s3.studylib.net/store/data/007214461_1-73dc883661271ba5c9149766483dcfed-300x300.png)