Transdermal Oxygen Delivery to Diabetic Wounds: A
advertisement
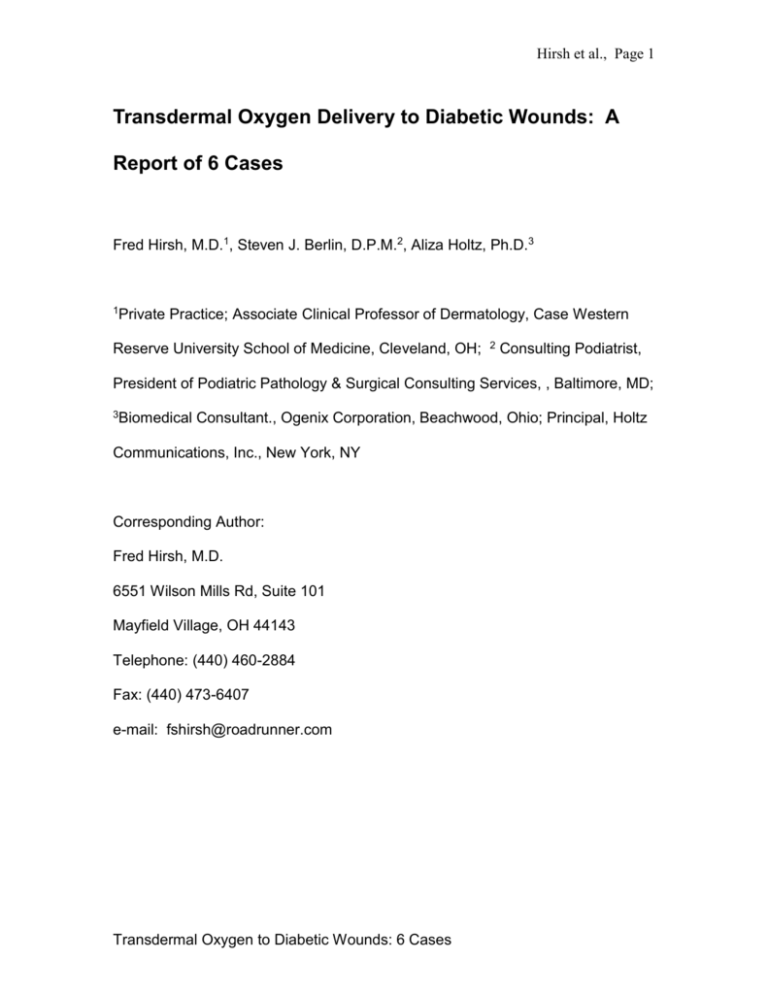
Hirsh et al., Page 1 Transdermal Oxygen Delivery to Diabetic Wounds: A Report of 6 Cases Fred Hirsh, M.D.1, Steven J. Berlin, D.P.M.2, Aliza Holtz, Ph.D.3 1Private Practice; Associate Clinical Professor of Dermatology, Case Western Reserve University School of Medicine, Cleveland, OH; 2 Consulting Podiatrist, President of Podiatric Pathology & Surgical Consulting Services, , Baltimore, MD; 3Biomedical Consultant., Ogenix Corporation, Beachwood, Ohio; Principal, Holtz Communications, Inc., New York, NY Corresponding Author: Fred Hirsh, M.D. 6551 Wilson Mills Rd, Suite 101 Mayfield Village, OH 44143 Telephone: (440) 460-2884 Fax: (440) 473-6407 e-mail: fshirsh@roadrunner.com Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 2 Abstract Objective To evaluate the use of a transdermal sustained oxygen delivery (TSOT) system to promote the healing of chronic lower extremity wounds in patients with diabetes. Six patients (5M, 1F; 32-77 years old) with diabetes and chronic lower extremity wounds unresponsive to prior multimodal therapy were treated with transdermal sustained oxygen. The transdermal sustained oxygen delivery device (EpiFLOSD; Ogenix Corporation, Cleveland, Ohio) delivered 100% oxygen at 3 mL/hr with ambient humidity, 24 hr/day directly to the wound site which was covered by an occlusive dressing. Despite chronicity of wounds (aged 4 months to more than 15 years) and nonresponsiveness to previous treatments, all wounds in this case series treated with transdermal sustained oxygen therapy improved within 2 to 20 weeks, within which time 5 of the 6 wounds had healed completely. In two cases scheduled amputation were prevented. The results of the six cases reported here strongly support the use of transdermal sustained oxygen therapy in promoting the healing of diabetic foot Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 3 and leg ulcers refractory to previous treatments. In addition, amputation was prevented in two cases, thus reducing prolonged costly patient care! Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 4 Introduction The National Health Interview Survey (NHIS) of 2003 estimated that the total prevalence of diabetes in the U.S. for all ages is 20.8 million people (7.0% of the population as a whole).1 Of these, an estimated 15% will develop foot ulcers during their lifetimes.2 More than 15% of foot ulcers result in amputation of the foot or limb,3 and foot ulcers precede approximately 85% of nontraumatic lowerlimb amputations in people with diabetes.4 In 2004, approximately 71,000 nontraumatic lower-limb amputations were performed in people with diabetes.5 In fiscal year 1992 under DRG reimbursement code 271 (skin ulcer) the average Medicare claim for inpatient care for foot ulcers was $10,171, and Medicare received 23,352 such claims.4 (These numbers do not include private insurance claims). In a 3-year (1993-1995) retrospective cohort study of patients with diabetes in a staff-model health maintenance organization, Ramsey et al.3 observed a cumulative incidence of foot ulcer of 5.8%, and determined that, for the 2 years following diagnosis, the attributable cost for a 40-to-60-year-old male with a new foot ulcer was $27,9876 The Undersea and Hyperbaric Medical Society's 1999 Committee Report states the cost of treating non-healing lower extremity diabetic ulcers totals more than $200 million annually. Gordois et al.7 determined that in 2001 the mean annual cost of treating an uninfected diabetic foot ulcer was $9,306, whereas that of treating an infected foot ulcer was $24,582, and that of a foot ulcer with osteomyelitis was $45,579. In the United Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 5 States, the average hospitalization cost: $31,264; average amputation cost: $40,000; estimated Total (excluding rehabilitation and related medical and surgical disability care): $71,264; with an average of $30,000 for rehabilitation, the total cost is: $ 101,264. In a study of anatomic, pathophysiologic, and environmental factors contributing to the development of incident diabetic foot ulcers, Reiber et al.8 determined that the most common components of a patient’s causal pathway to foot ulcers were neuropathy (78%), minor traumatic event (77%), and foot deformity (63%), followed by edema (37%), ischemia (35%), and callus formation (30%). Foot ulcers may become chronic, non-healing wounds. Often painful, they always require vigilant attention to prevent infection. Because foot and leg ulcers precede amputations in a majority of instances, the importance of promoting wound healing cannot be overstated, and the need for therapeutically effective and cost-effective measures for the prevention and treatment of diabetic foot ulcers is self-evident. Oxygen has long been recognized as having an important role in wound healing, and much research in recent years has been aimed at elucidating this role at the cellular and molecular levels.9 Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 6 The recent development of a self-contained miniature device (EpiFLO®) that delivers transdermal oxygen therapy directly to the wound bed has made it possible for some patients to remain ambulatory while receiving oxygen therapy at the site of the ulcer (in contrast to the confinement and intermittent exposure associated with the use of a hyperbaric oxygen chamber or being attached to an oxygen tank to get topical oxygen therapy). The following are six case reports of chronic lower limb wounds in patients with diabetes who were treated with transdermal sustained oxygen therapy (TSOT) to promote wound healing. Methods Oxygen was delivered to the wound via a small, self-contained device (EpiFLOSD, Ogenix Corporation, Cleveland, Ohio) that produces 100% O2 at 3 mL/h continuously by means of a battery-driven electrochemical reaction. A sterile cannula leading from the device to the wound site which is covered by an occlusive dressing provides direct delivery of oxygen to the wound at ambient humidity 24 hours a day. The device is a single-patient, single-use, 7-day or 15day disposable apparatus. Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 7 Case Reports Case 1 A 77-year-old white male with diabetes presented with a 5-month-old neuropathic foot ulcer (2.5 cm long x 2.5 cm wide x 1 cm deep) with osteomyelitis. The patient had a prior history of two toe amputations because of wounds. Belowthe-knee amputation was planned because previous therapies, including revascularization of area had failed. Fifteen weeks after the initiation of TSOT (EpiFLOSD ), the osteomyelitis was resolved and the wound had closed completely.10 Case 2 A 74-year-old male with insulin-dependent diabetes with a history of renal failure was undergoing dialysis at the time of presentation. In addition to severe leg edema, he had a 48-week-old open weeping ulcer (72 x 80 x 2 mm) on the left lower extremity (Figure 2A). The ulcer had progressed and enlarged during the previous 12 months despite multimodal treatment (silver nitrate, topical and systemic antibiotics, and Ace wrap). Treatment with TSOT (EpiFLOSD ) was initiated and continued until the wound closed. One week after initiation of TSOT treatment, excellent granulation tissue and early re-epithelialization were Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 8 observed and the patient reported less pain. At Week 2, re-epithelialization tissue had improved significantly and the wound dimensions had decreased. The wound was covered with DuoDERM® (ConvaTec). At Week 3 the wound had almost closed (wound dimensions had decreased from 60 x 100 x 1 mm at Week 1 to 15 x 10 x 1 mm at Week 3) (Figure 2B). Twice during Week 3 the EpiFLOSD canula was temporarily dislodged, but this did not negatively influence the overall healing. After 4 weeks of treatment, the wound had completely closed. Case 3 A 68-year-old female with a 15-year history of diabetes had a fairly painful ulcer on the dorsum of the foot that remained open with no evidence of healing despite multimodal treatments. The lesion was nonpurulent, had no odor, and had been stable for 12 years, measuring 60 x 60 x 3 mm (Figure 3A). One week after the initiation of TSOT (EpiFLOSD ) treatment, a large amount of exudate was noted, as was increased bleeding on debridement, but there was no change in the size of the lesion. During weeks 2-8, persistent drainage and a foul-smelling discharge were noted, but the wound never became infected. The lesion was healing slowly and steadily, measuring 40 x 40 x 2 mm at Week 8. At Week 9, the lesion was fully granulated, drainage was minimal, and the depth of the wound decreased to 0.5 mm. The pain had completely resolved during this period. Extensive re-epithelialization was observed at Week 10 and the lesion was reduced to 10 x 15 x 0.0 mm (Figure 3B). Our data extend through only Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 9 Week 10 because the patient suddenly expired before the wound completely healed. Case 4 A 32-year-old male with diabetes had an ulcer (4 x 4 x 2 mm) with 100% red granulation tissue and macerated edges on the plantar aspect of the left great toe (Figure 4A). The wound had been open for 6 months. Prior treatment included wet to dry therapy with iodine gel to control infection and absorb the wound exudate. One week after EpiFLOSD treatment, the wound was reduced to pinpoint size (1 x 1 x 0 mm), and after two weeks, the ulcer was completely closed and healed (Figure 4B). Case 5 A 50-year-old female with diabetes mellitus had two neuropathic ulcers that had not healed for 24 months, one 3.5 cm x 1.8 cm x 1.5 cm on the right plantar foot and the other 3.8 cm x 1.2 cm x 0.8 cm on the right medial foot (Fig 5A). Prior to presenting at the wound care clinic, the patient had been hospitalized, received antibiotic therapy and debridement. The patient was treated with TSOT only for the wound on the right medial foot ;for the next eight weeks, dressings being changed QOD as necessary depending on drainage and then weekly until healed. The TSOT treated wound healed in 8 weeks (Fig 5B). The wound on the right plantar foot did not receive TSOT, but received regular dressing changes. This wound healed in two weeks. It appears the TSOT treatment on the right medial foot wound had beneficial spill-over effects on the wound on the right plantar foot. Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 10 Case 6 A 54-year-old male with diabetes and a deformed Charcot foot had a 4-month-old foot ulcer (8.0 cm x 6.0 cm x 0.8 cm on presentation) on the left plantar aspect of the heel area of the left foot (Fig 6A) as well as another wound on the lateral distal aspect of the left foot in an area where toes had been amputated. The treatment history of the left plantar wound consisted of wet to dry dressings for several months prior to TSOT (EpiFLOSD).. A scheduled amputation was anticipated, but delayed for a trial of TSOT. The oxygen therapy closed the chronic ulcer in 20 weeks (Fig 6B) and amputation was cancelled.. Results A summary of the six case reports is presented in Table 1. Despite the chronic nature of the wounds (aged 4 months to more than 15 years) and their nonresponsiveness to previous treatments, all wounds in this case series treated with TSOT responded within 2 to 20 weeks, within which time 5 of the 6 wounds had healed completely. In two cases scheduled amputations were cancelled. In all cases, an occlusive form of dressing was applied to enhance the oxygen therapy and the treatment was well-tolerated and without complications. Due to the nature of this therapy, none of the patients were restricted in any fashion. Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 11 Discussion The results presented in each of the six case reports above demonstrate the efficacy and safety of EpiFLOSD, a transdermal sustained oxygen delivery system, in promoting wound healing in instances of recalcitrant wounds despite prior multimodal efforts to help them heal. In a study by Oyibo et al.,11 the area of a foot ulcer at presentation was correlated with healing time and also predicted healing of the ulcer in diabetic patients with new foot ulcers. These investigators showed also that the presence of ischemia was a predictor of nonhealing, and, as would be expected, neuroischemic ulcers and infected ulcers took longer to heal than those without these confounding factors. Age, sex, type of diabetes, duration of diabetes at presentation, and site of foot ulcer did not influence the outcome of diabetic foot ulcers. In their study of the outcomes of diabetic foot ulcers after 6 to 12 months in 194 patients who presented with new foot ulcers, Oyibo et al. found that the median (interquartile range; IQR) ulcer area in patients whose ulcers healed was 1.1 (0.5-2.6) cm2 whereas the median (IQR) ulcer area in patients whose ulcers did not heal was 1.4 (0.7-3.5) cm2. Median (IQR) ulcer areas of 3.9 (1.4-5.4) cm2 were associated with amputation.11 If ulcer area according to Oyibo et al.11 had been used as a predictor of healing in our cases, only one of the six would have been predicted to heal, and the other Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 12 five would have been predicted to have led to amputation. However, our cases demonstrate that sustained transdermal oxygen therapy promoted healing even in ulcers refractory to various previous therapies and with areas as large as 58 cm2, and that the healing occurred within.2 to 20 weeks. In fact, amputations had been scheduled for two of the cases but were cancelled because of the healing. Treating physicians noted that within approximately 1 to 2 weeks of initiation of the use of EpiFLOSD, the wounds produced an exudate, and this was followed by the process of epithelialization. A recent animal study demonstrated improved epithelial healing in a rabbit ear wound model using the same transdermal sustained oxygen delivery device. 9 The results of the animal study as well as the observations noted in the current case reports suggest that transdermal sustained oxygen delivery promotes epithelial wound healing in cases of leg and foot ulcers in patients with diabetes. If further research with transdermal sustained oxygen therapy in diabetic and other chronic—and possibly also acute—wounds yields similar results, it is likely that the physical and economic burdens of at least some of the complications of diabetes will be mitigated. It is reasonable to assume from the results presented here that the costs of treatment of diabetic leg ulcers in this case series were decreased with the use of EpiFLOSD compared to the probable costs of continued treatment of recalcitrant wounds or to the costs of amputation and follow-up care. EpiFLOSD can be up to Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 13 50% less costly than other advanced wound care therapies when comparing the device cost to that of other devices and treatments. Randomized controlled trials currently under way will capture health econometric data—including other costs such as nursing time, dressings and other components—and further the cost benefit analysis over the entire episode. Conclusion The results of the six cases reported here provide strong support for the use of transdermal sustained oxygen therapy in promoting the healing of diabetic foot and leg ulcers that were refractory to other prior treatments. Large wound areas (up to 58 cm2) that would have been predicted not to heal and amputation may have been necessary were healed within 20 weeks of initiation of transdermal sustained oxygen therapy, and in two cases, scheduled amputations was cancelled. The healing ability of a continuous oxygen therapy device (EpiFLOSD) has shown to reduce the amputation potential in healing chronic wounds and has also shown that the continuous flow of oxygen has also eliminated pain associated with such wounds. It is reasonable to assume that Transdermal Sustained Oxygen Therapy can reduce the financial burden of chronic diabetic ulcers. Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 14 Acknowledgments We thank Alan Hirsh, M.D., Alex Hirsh, M.D., Scott Hirsh, D.P.M., Philibert Fluck, PT, and David Skrobot, D.P.M. for providing the data and photographs from their cases and for their assistance in reviewing the manuscript. Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 15 References 1. Harris MI. Chapter 1: Summary. In: Diabetes in America. 2nd ed: National Diabetes Data Group, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, NIH Publication No. 95–1468; 1995. p. 1-14. 2. Palumbo PJ, Melton LJ. Peripheral vascular disease and diabetes. In: Harris MI, Hamman RF, editors. Diabetes in America. Washington, DC: U.S. Government Printing Office, NIH publication no. 85-1468; 1985. p. XV 1-21. 3. Ramsey S, Newton K, Blough D, et al. Incidence, outcomes and cost of foot ulcers in patients with diabetes. Diabetes Care 1999;22:382-387. 4. Reiber GE, Boyko EJ, Smith DG. Chapter 18. Lower extremity foot ulcers and amputations in diabetes. In: Diabetes in America. 2nd ed: National Diabetes Data Group, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. NIH Publication No. 95-1468; 1995. p. 409-428. 5. National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics Fact Sheet: general information and national estimates on diabetes in the United States, 2003. Bethesda, MD: U.S. Department of Health and Human Services, National Institute of Health, 2003. Rev. ed. Bethesda, MD: U.S. Department of Health and Human Services, National Institute of Health, 2007. NIH Publication No. 08-3892; 2008 June. 6. Mackey WC, McCullough JL, Conlon TP, et al. The costs of surgery for limb-threatening ischemia. Surgery 1986;99(1):26-35. 7. Gordois A, Scuffham P, Shearer A, Oglesby A, Tobian JA. The Health Care Costs of Diabetic Peripheral Neuropathy in the U.S. Diabetes Care 2003;26(6):1790-1795. 8. Reiber GE, Vileikyte L, Boyko EJ, et al. Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Diabetes Care 1999;22(1):157-62. 9. Said HK, Hijjawi J, Roy N, Mogford J, Mustoe T. Transdermal sustaineddelivery oxygen improves epithelial healing in a rabbit ear wound model. Arch Surg 2005;140(10):998-1004. 10. Wilson C, Hirsh S, Hirsh A, Burk M. Transdermal, Sustained Oxygen Therapy Promotes Healing of a Diabetic Foot Ulcer in a Patient with Osteomyelitis – A Case Report. Wound Healing Society Annual Meeting. Chicago; 2005 (Poster presentation). 11. Oyibo SO, Jude EB, Tarawneh I, et al. The effects of ulcer size and site, patient's age, sex and type and duration of diabetes on the outcome of diabetic foot ulcers. Diabetic Medicine 2001;18(2):133-138. Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 16 Table Table 1. Summary of Cases Cas e No. 1 M/F Patient Age M 77 5 months 2.5 cm x 2.5 cm x 1 cm 6.25 cm2 Time to heal with EpiFLO(SD) 15 weeks 2 M 74 48 weeks 7.2 cm x 8.0 cm x 0.2 cm 57.6 cm2 4 weeks Yes 3 F 68 12 years 6.0 cm x 6.0 cm x 0.3 cm 36 cm2 No 4 M 32 6 months 0.4 cm x 0.4 cm x 0.2 cm 0.2 cm2 Extensive epithelialization & reduction of lesion to 10 mm x 15 mm x 0 mm at 10 weeks 2 weeks 2 weeks (dressing changes only; no EpiFLO) 8 weeks No 20 weeks (EpiFLO treatment from Weeks 6 to 26) Yes 5 6 F M 50 54 Wound Age Wound size Wound area cm2 24 months 3.5 cm x 1.8 cm x 1.5 cm on right plantar foot 6.3 24 months 3.8 cm x 1.2 cm x 0.8 cm on right medial foot This wound was treated with EpiFLO, while the adjoining wound above was not treated with EpiFLO. 8.0 cm x 6.0 cm x 0.8 cm 4.6 cm2 4 months Transdermal Oxygen to Diabetic Wounds: 6 Cases 48 cm2 Amputation Scheduled ? No No No Hirsh et al., Page 17 Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 18 Figures FIGURE LEGENDS Figure 1. Case 1—Non-healing 5-month-old neuropathic foot ulcer with osteomyelitis in 77-year-old male with diabetes at Week 0 (A); osteomyelitis was resolved and wound was healed after 15 weeks of treatment with EpiFLOSD (B). Figure 2. Case 2—Non-healing unresponsive weeping ulcer at week 0 (A) on lower right leg of 74-year-old male with insulin-dependent diabetes and renal failure; after 4 weeks of EpiFLOSD treatment, wound was completely closed (B). Figure 3. Case 3—A chronic, non-healing, diabetic foot ulcer with a vascular component that had been stable for 12 years (A) in a 68-year-old female was significantly reduced after 10 weeks of treatment with EpiFLOSD (B). Figure 4. Case 4—A diabetic foot ulcer that had not healed for 6 months (A) in a 32-year-old male was completely closed after 2 weeks of treatment with EpiFLOSD (B). Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 19 Figure 5. Case 5—Non-healing neuropathic right medial foot ulcer (A) in 50year-old female with diabetes healed after 8 weeks of EpiFLOSD treatment (B). Figure 6. Case 6—Four-month-old wound (A) in a 54-year-old male with diabetes mellitus and Charcot foot healed after 26 weeks of treatment, first with 6 weeks of wet-to-dry dressings only, followed by 20 weeks with EpiFLOSD (B). Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 20 Figure 1 (A) Figure 1 (B) Courtesy of Alan Hirsh, MD, Orange Village, OH Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 21 Figure 2 (A) Figure 2 (B) Week 0 Week 4 Courtesy of Alex Hirsh, MD, Cleveland, OH Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 22 Figure 3(A) Figure 3 (B) Courtesy of Alan Hirsh, MD, Orange Village, OH Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 23 Figure 4 (A) Figure 4 (B) Courtesy of David Skrobot, DPM, Zanesville, OH Transdermal Oxygen to Diabetic Wounds: 6 Cases Hirsh et al., Page 24 Fig. 5A Week 0 Fig. 5B Week 8 Fig. 6A Week 0 Fig. 6 B Week 26 Courtesy of Philibert Fluck, PT, U.S.Virgin Islands Transdermal Oxygen to Diabetic Wounds: 6 Cases