G:\respcare\charting
advertisement
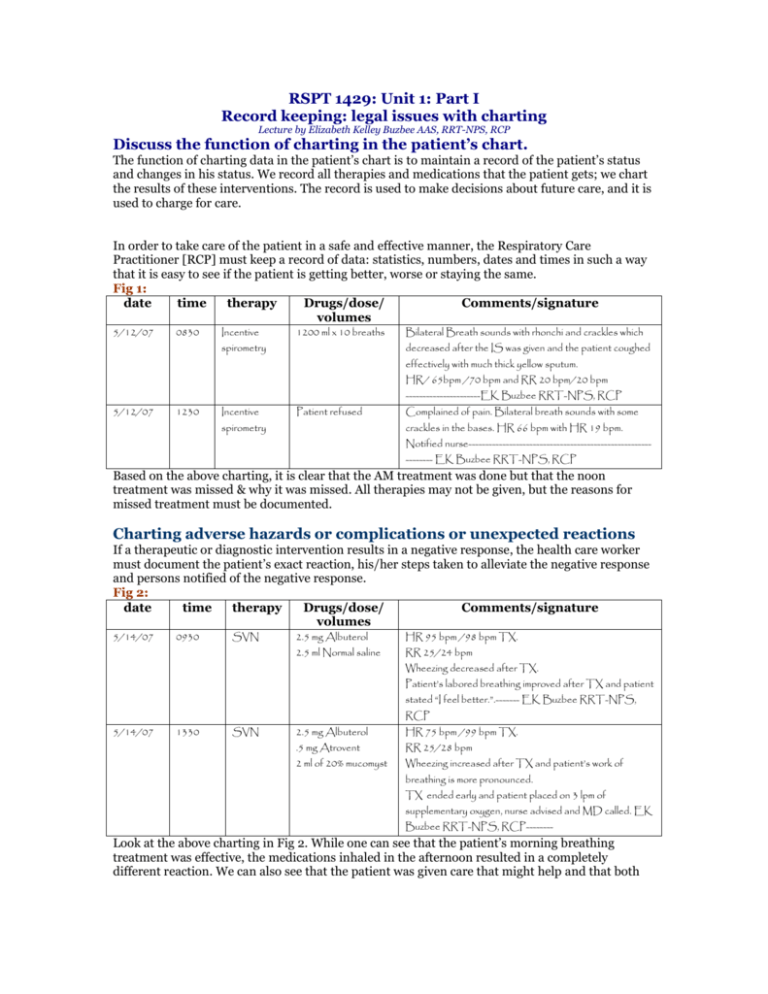
RSPT 1429: Unit 1: Part I Record keeping: legal issues with charting Lecture by Elizabeth Kelley Buzbee AAS, RRT-NPS, RCP Discuss the function of charting in the patient’s chart. The function of charting data in the patient’s chart is to maintain a record of the patient’s status and changes in his status. We record all therapies and medications that the patient gets; we chart the results of these interventions. The record is used to make decisions about future care, and it is used to charge for care. In order to take care of the patient in a safe and effective manner, the Respiratory Care Practitioner [RCP] must keep a record of data: statistics, numbers, dates and times in such a way that it is easy to see if the patient is getting better, worse or staying the same. Fig 1: date time therapy Drugs/dose/ Comments/signature volumes 5/12/07 0830 Incentive 1200 ml x 10 breaths spirometry Bilateral Breath sounds with rhonchi and crackles which decreased after the IS was given and the patient coughed effectively with much thick yellow sputum. HR/ 65bpm /70 bpm and RR 20 bpm/20 bpm ----------------------EK Buzbee RRT-NPS, RCP 5/12/07 1230 Incentive Patient refused spirometry Complained of pain. Bilateral breath sounds with some crackles in the bases. HR 66 bpm with HR 19 bpm. Notified nurse------------------------------------------------------------- EK Buzbee RRT-NPS, RCP Based on the above charting, it is clear that the AM treatment was done but that the noon treatment was missed & why it was missed. All therapies may not be given, but the reasons for missed treatment must be documented. Charting adverse hazards or complications or unexpected reactions If a therapeutic or diagnostic intervention results in a negative response, the health care worker must document the patient’s exact reaction, his/her steps taken to alleviate the negative response and persons notified of the negative response. Fig 2: date time therapy Drugs/dose/ Comments/signature volumes 5/14/07 0930 SVN 2.5 mg Albuterol HR 95 bpm /98 bpm TX. 2.5 ml Normal saline RR 25/24 bpm Wheezing decreased after TX. Patient’s labored breathing improved after TX and patient stated “I feel better.”.------- EK Buzbee RRT-NPS, RCP 5/14/07 1330 SVN 2.5 mg Albuterol HR 75 bpm /99 bpm TX. .5 mg Atrovent RR 25/28 bpm 2 ml of 20% mucomyst Wheezing increased after TX and patient’s work of breathing is more pronounced. TX ended early and patient placed on 3 lpm of supplementary oxygen, nurse advised and MD called. EK Buzbee RRT-NPS, RCP-------- Look at the above charting in Fig 2. While one can see that the patient’s morning breathing treatment was effective, the medications inhaled in the afternoon resulted in a completely different reaction. We can also see that the patient was given care that might help and that both the nurse and the doctor have been notified. Furthermore, one can see that the medication given in the AM differs from that given in the PM. The above data is objective with numbers and other measurable data that can be used to further assess the patient. When the doctor looks that this record, he/she can make decisions about medication because all of the available information is there. Not only can he make a decision, he can reassess the patient’s response to the new care because he has measurable data to compare. Please notice what is NOT there. The RCP charts only the results, not her conclusions that the patient might not be tolerating the one of the drugs. The RCP does not use phases like, “Patient looks terrible,” or other subjective, even emotional descriptions. Discuss the Legal Status of the Patient Chart. The Respiratory Care Practitioner [RCP] must remember that all patient charts are always legal documents that are subject subpoena in a court of law. Under these circumstances, we not only sign with our first initial and last name, we sign with our professional credentials. [see entries in Fig 1 and 2] In addition to making it easier identify who we are when we sign with credentials, these professional designations tell the court if we are qualified to perform and assess this therapy. For instance, if a registered dietician was to make a determination about the effectiveness of a given amount of supplementary 02, this statement would be of less importance that the registered respiratory therapist’s opinion, because oxygen is the business of the RCP. Identify how the signature is written in the chart A student would be clearly designated as a student respiratory therapist and the signature of the credentialed RCP co-signing the document would immediately follow so the court can tell if the student was supervised by a credentialed RCP. Credentials: RRT: registered respiratory therapist [passed all three exams] CRT: certified respiratory therapist [passed the entry level exam] RRT-NPS: registered therapist with a specialty in neonatal and pediatric care CRT-NPS: certified respiratory therapist with a neonatal / pediatric specialty RPFT: registered pulmonary function technologist [passed advance PFT exam] CPFT: certified pulmonary function technologist [passed entry level PFT exam] RCP: in the state of Texas, all respiratory care personal must be a state-cerified respiratory care practitioner. Explain how an error is corrected in the chart Mistakes happen; because this is a legal document, the RCP would be careful to correct entries in such a way that the original mistaken data is readable. Draw a single line over the error, write “Error” over the entry and then keep going. Attempting to erase or eradicate the erroneous data just makes a jury suspicious. Remember that most documents will be completed by several persons over several days, so each entry needs to be correctly dated, timed and signed. If the RCP forgot to document something and goes back to discover someone has written in the next space, the late entry should labeled “Late entry,” and the time of the actual therapy so that there is no question of the sequence of the patient’s care. Never chart in pencil or erasable ink, never erase and never chart in anything but black ink because black reproduces more clearly and these records will be copied and reduced and kept for years. We chart in past tense after we do the procedure; never in future tense because we are charting what has happened, never what might have been. We chart using standard abbreviation and standardized terminology. If a form uses odd abbreviations, the form needs to include ‘translation.” Sometimes a chart will have only enough room for initials, but some place on the document, the RCP should be able to sign next to her initials so that anyone reading the document knows exactly who charted what. Because this is a legal document, to protect oneself, the RCP would draw lines so that no one else can chart on the same line. [see above entries] Military time Because hospitals run 24/7, we use military time. 700 AM is 0700, while times after 12 noon are calculated as [12 + hour] so 1 PM is 12 = 1 = 1300. 4 PM is 12 + 4 = 1600. Midnight is 12 + 12 + 2400, but 1200 is noon and one in the morning is 0100. Computer charting: Those hospitals that have moved to computer charting will provide the RCP with a logon and password that will identify the person by name and credentials. Federal laws protecting patient confidentiality prevents staff from sharing these passwords. The actual programs used by RT departments are varied but with all any errors will be dealt with in such a manner that it is clear when the error was made and when & by whom it was corrected. Record keeping: On a regular basis, any patient records can be accessed by [1] case workers employed by thirdparty payer such as insurance companies or federal agencies such as Medicare/Medicaid. [2] Nursing and respiratory care supervisors during quality assurance monitoring [3] regulatory agencies that award hospitals their credentials and [4] If there is legal action, both parties will get copies of all hospital records for use in the case. HIPAA: Federal law passed in 1996 that protects the privacy of the patient, but allows authorized parties to access the chart when it is needed for care or for billing. The law includes electronic information as well as paper records. USA website for HIPAA: http://www.hhs.gov/ocr/hipaa/ Patient’s rights page: http://www.hhs.gov/ocr/hipaa/consumer_summary.pdf Discuss the legal ramifications of failing to chart. Most hospital bills are paid by third parties such as insurance companies or Medicare/Medicaid. Our charting is part of the required paperwork for this billing procedure. Patients can only be charged for care that has been given. We have to have a record that can justify a billing entry. As far as billing is concerned; if you don’t chart it, you didn’t do it. Charting therapy that was not given is considered fraudulent and if the patient is a Medicare patient, this fraud is against federal law. Discuss the problems associated with only charting changes or deteriorations. The respiratory therapist taking care of the patient needs to document statistics on each visit to the patient’s bedside. If the patient vital signs are unchanged by the therapy or the medication we give, this must be documented. Example: Fig. 3 date 8/22/07 The RCP who is taking care of Mr. Spenser who needs to get 2.5 mg of Albuterol every 4 hours. His first treatment was done at 0730 in the AM making his next treatment due at 11:30 AM. She goes into the room at 11:15 and discovers that the patient is out of the room, returns at 11:30, at 1200, at 12:30 when the patient refuses the treatment. At 100 PM [1300] the nurse finds him slumped over the bed in great respiratory distress. This is what she charted. time 0730 therapy SVN Drugs/dose/ volumes Comments/signature 2.5 mg Albuterol in 3 HR 88bpm/88bpm & RR 20 bpm/19 bpm ml normal saline Bilateral breath sounds with diffuse expiratory wheezing that decreased after TX. ------- EK Buzbee RRT-NPS, RCP 8/22/07 1326 SVN 2.5 mg Albuterol in 3 HR 110bpm/115bpm & RR 30 bpm/29 bpm ml normal saline Bilateral breath sounds with diffuse expiratory wheezing that persists after the TX. MD called. ---. EK Buzbee RRT-NPS, RCP-------- If you were this RCP’s supervisor who was investing this situation, you would be hard pressed to defend your RCP because she gave you nothing to work with. Below see how this same situation could have been documented. Fig. 4 date time therapy Drugs/dose/ Comments/signature volumes 8/22/07 0730 SVN 2.5 mg Albuterol in 3 HR 88bpm/88bpm & RR 20 bpm/19 bpm ml normal saline Bilateral breath sounds with diffuse expiratory wheezing that decreased after TX. ------- EK Buzbee RRT-NPS, RCP 8/22/07 8/22/07 8/22/07 8/22/07 11:15 11:30 12:00 12:30 TX not Pt out of room. given EK Buzbee RRT-NPS, RCP-------- TX not Pt out of room. given EK Buzbee RRT-NPS, RCP-------- TX not Pt out of room. given EK Buzbee RRT-NPS, RCP-------- TX not Pt refused. No apparent respiratory distress at this time. given Patient states: “I feel fine; I’ll call for TX.’ Nurse advised. EK Buzbee RRT-NPS, RCP--------