Immunology - very short notes - Croydon Health Services NHS Trust
advertisement

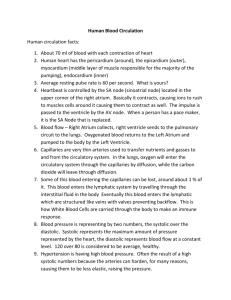
Immunology - short notes for GPs! As part of South West London Pathology the Immunology and Allergy service for Croydon University Hospital (CUH) is provided by the Protein Reference and Immunopathology Unit (PRU) at St. George’s Hospital. It is one of two UK Supra-regional Assay Service centres and provides an analytical and clinical advisory service. Interpretative comments are added to reports and telephone advice is available directly from the PRU. Clinically critical results will be telephoned to the requesting clinician where possible and the Duty Biochemist at CUH will also be alerted. Urgent requests or requests for advice can be made directly to the: PRU at St. George’s on The clinical team at CUH on 0208 725 0025 or 5106 0208 401 3024 or 3548. General notes Most “routine” tests e.g. ANA done daily, complex tests weekly and rare tests done when required. Phone us if you have a question - if you are not sure what test you want, phone to discuss first. Some tests need special collection e.g. cryoproteins - call CUH lab to arrange an appointment. No test has 100% specificity and 100% sensitivity for disease – Immunology tests often show both false negative and false positive results. Tests can be consistent with or suggestive of a disease, part of the diagnostic criteria or used in assessment of disease prognosis. Where used for monitoring, it is rarely necessary to measure more frequently than monthly (usually much less frequently). Repeat screening is rarely indicated unless new symptoms develop, certainly not within a year. Immunology testing is generally expensive e.g. coeliac testing costs £9.18, a single RAST test cost £15.89 and an ANA costs £11.60 - so use the tests carefully! Rheumatoid Factor (RF) Antibodies against the constant portion of other antibodies - usually IgM antibodies against the Fc portion of IgG. RF is NOT specific for rheumatoid arthritis however closer association with higher concentrations. Positive RF can be seen in the elderly, patients with chronic infections/inflammatory processes, B cell malignancy. Not very helpful for monitoring RA - better to use CRP. Anti CCP antibodies are the new exciting test – but NICE say refer the patient to Rheumatology if you think they have RA rather than doing lots of tests, so currently only offered for secondary care. Antinuclear antibodies (ANA) IgG antibodies to components of the cell nucleus e.g. DNA (double and single stranded), proteins and enzymes associated with nuclear functions. These nuclear components are distributed in the nucleus either homogeneously (DNA), in chromosomes (double stranded DNA) or in little clumps speckled throughout the nucleus (the Extractable Nuclear Antigens or ENAs). Relevant follow-on tests are automatically added depending on the staining pattern seen o No nuclear staining - ANA negative. o Homogeneous pattern - check specific antibodies to dsDNA - especially if chromosome staining is seen. o Speckled pattern - check for antibodies to the ENAs. There are only a few clinically relevant ENAs – antibodies to ss (Sjogrens syndrome) A and B, a.k.a. Ro and La. Anti Ro antibodies can cause foetal heart block. Anti Sm is very specific for SLE (but not sensitive). Anti RNP antibodies are seen in mixed connective tissue disease. Low titre ANAs (1/80) are usually non-specific findings and are often seen in infections (usually viral), chronic inflammatory conditions, more commonly in women than men, and in aged patients. Follow-up in 3-6 months (sooner only if clinically indicated) to see whether these antibodies have increased in concentration or disappeared is usually advised. Anti neutrophil cytoplasmic antibodies (ANCA) IgG antibodies to enzymes in the cytoplasm of neutrophils. The proteinase III enzyme is evenly distributed actoss the cell cytoplasm while the myeloperoxidase sits in the perinuclear area. Anti PRIII antibodies give a c (cytoplasmic)ANCA staining pattern and Anti MPO antibodies give a p (perinuclear)-ANCA staining pattern. c-ANCA and anti PRIII antibodies are associated with small vessel vasculitis e.g. Wegener's granulomatosis and microscopic polyarteritis. p-ANCA and anti MPO antibodies are seen in PAN, Churg Strauss and rheumatoid vasculitis. Serial monitoring of the anti PRIII or the anti MPO may be useful in known disease. When investigating a patient with deteriorating or poor renal function, if you ask for an ANCA you should also consider anti Glomerular Basement Membrane antibodies (GBM) - they are associated with Goodpastures syndrome and patients may have very similar symptoms. ANCA and GBM antibodies would usually only be relevant for patients in secondary care. Other conditions/disease and their relevant Immunology testing Coeliac - IgA & IgG anti-Tissue Transglutaminase (NICE guidelines); endomysial antibodies added if indicated Autoimmune liver - ANA, anti-mitochondrial, anti LKM and anti smooth muscle Abs Pernicious anaemia (only if B12 deficient) - anti Gastric parietal cell; intrinsic factor antibodies added if positive. Rheumatology/Connective tissue - ANA + appropriate follow on tests, Rheumatoid factor Vasculitis - ANCA and appropriate follow on tests Hypothyroidism & Hashimotos - TFTs thyroid peroxidase (or microsomal) antibodies Graves disease - TSH receptor antibodies Bullous skin diseases - skin basement membrane or intercellular cement Renal disease in SLE or active immune complex disease – Complement, particularly C4 IgE and Allergy Allergic diseases are affecting an increasing proportion of the population. Testing should be done on the basis of a good history that identifies possible allergens. Blanket allergy testing is extremely costly and of limited clinical value. Check what symptoms and when – e.g. if winter, unlikely to be pollen allergen. Timing of pollens – tree, followed by grasses then weeds. Symptoms all year - house dust mite, feathers. For respiratory allergies, skin testing is the most appropriate investigation but you can do specific IgE. It can be difficult to skin test if the patient is a baby/child, if the patient has significant skin problems, it is unreliable if the patient is on anti-histamines and it lacks sensitivity for food allergies. For suspected food allergy, ideally a food diary should be kept and testing based on this. Testing for multiple, easily excluded (non-staple) foods is not appropriate. Not all reactions are IgE mediated - e.g. strawberries, chocolate and wine can be direct pharmacologic effects. Most allergens have been reported to cause anaphylaxis - the most common are Penicillin, wasp and bee venom, peanuts, latex, egg, fish and shellfish. Immunoglobulins and electrophoresis Immunoglobulins behave as acute phase proteins and their concentration changes in numerous diseases; there are really only two clear indications for measuring Igs and doing protein electrophoresis – these are: (1) Investigation of suspected immune deficiency and (2) Investigation of suspected B cell malignancy. When considering lymphoid malignancy you should ALWAYS check SERUM AND URINE for paraprotein. Incidence of Ig classes in paraproteins is IgG>IgA>IgM>kappa>lambda>IgD>IgE. Kappa and lambda are the light chains and if MONOCLONAL are called Bence Jones protein. IgM paraproteins (big molecule, intravascular - can give hyperviscosity) usually result from tumours earlier in B cell progression - e.g. Waldenstroms macroglobulinaemia, CLL, lymphoma. Paraprotein types in myeloma: IgG>IgA>Bence Jones protein ( or are approx 20% of all myelomas) IgD (approx 3% of myelomas). BJP is small and passes easily through the glomerulus so you can miss BJ only myelomas if you only look in the serum - usually you see low serum IgG, A and M and a monoclonal band on the urine EP. BJP-only and IgD myelomas are usually more aggressive. Diagnosis of myeloma - 2/3 of paraprotein in serum and/or urine, lytic lesions on X-ray survey, abnormal numbers of plasma cells in bone marrow. Paraproteins are also seen in benign disease, secondary to infection, in monoclonal gammopathy of unknown significance and with increasing prevalence in the elderly population. Small paraproteins can be incidental findings, particularly in the elderly. Follow local guidelines for investigation and monitoring. Consider Immune deficiency (ID) in any patient with repeated, severe, atypical infections. In adults, ID is most likely to be secondary to protein loss, malnutrition, cytotoxic treatment, immune suppression, infection (eg HIV), malignancy. Check IgG,A,M, albumin and protein EP. Primary ID is rare (IgA deficiency is the most common 1/700 of pop - many are asymptomatic). Common Variable ID worth considering in patients with bronchiectasis - IgG, A and M are usually all low and low-normal lymphocyte counts. IgG subclasses, complement components and more detailed testing are generally specialist immunology requests originating from secondary care. Dr Joanna Sheldon, Protein Reference Unit, St. George's Hospital Tel: 0208 725 0025 Dr Anne Tarn, CUH Chemical Pathology Tel: 0208 401 3024 July 2014