organ donation required readings
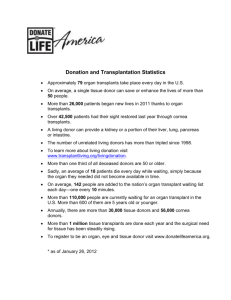
advertisement

Ethical Issues in Organ Donation Lo pg 301-310 issues: ● donor’s well-being compromised to benefit someone else ● need for organs higher than supply (98k on waiting list but just 35k transplants in 2006) Donation of Cadaveric Organs ● Ethical Concerns about Cadaveric Donation ● Harm to donors ● initial concerns that cadaveric donations hastened donors death ● criteria developed for determining death ● misunderstandings persist today about what brain death entails and people don’t understand why organs can’t be harvested from anencephalic infants and persons in a persistent vegetative state ● Respect for organ donors ● raise concerns about respect for human remains, wishes of the deceased ● deference given to wishes of survivors ● Conflicts of Interest ● decisions about potential donors care must be independent and take priority over decisions about organ procurement ● physician for potential donor may not be part of transplantation team ● payments for donation are prohibited to prevent abuse and exploitation of potential donors ● The Current System for Cadaveric Donation ● US has voluntary system for organ donation ● Uniform Anatomical Gift Act allows for organ donor card to grant permission to use organs for transplantation usually attached to drivers license, though few sign it ● people fear it might result in suboptimal care ● only 50% of relatives of brain dead patients give permission for donation ● some cultural beliefs pose barriers to organ donation eg Asian or Latino families believe bodies must be buried whole ● NonHeart-Beating Cadaver Donors ● most cadaver donors declared dead by brain criteria and have effective circulation ● growing number donors declared dead by cardiorespiratory criteria ie terminal patients whose life-sustaining interventions withdrawn eg trauma, intracerebral bleed, endstage musculoskeletal disease ● pts moved to OR where life support withdrawn, death declared, organs retrieved. ● might alter family experience of death bc time so short ● concerns: ● is donor really dead? (5 min from asystole to declaration, circulation cannot spontaneously return) ● process of donating organs can’t cause/hasten death so no association between care team and transplantation team (explicit consent needed for organ preservation steps such as heparin and catheter insertion for preservation solution) ● Proposals to increase donation of cadaveric organs ● Mandated Choice ● persons would be required to state preferences regarding donation while filing taxes or renewing drivers license ● Following Donor Cards ● drs would retrieve organs from people who had signed donor cards even if family objects ● technically this is what is legal now and ethically correct since following pt autonomy and advanced directives, however if family object strongly the adverse publicity could undermine public trust ● Presumed Consent ● organs harvested unless specified otherwise explicitly by pt or family ● unpopular concept ● Financial Incentives for Donation ● critics say undermines altruism, treats body as a commodity, and results in exploitation, fraud, or coercion especially in poor countries ● commercially motivated transplants in poor countries might increase rate of HIV, Hep B infection ● others propose modest incentives eg medical leave, life insurance, highest priority for transplantation if needed by living donors Donation of Organs from Living Donors -most have preexisting relationship w/ recipient -donation by non-relative feasible bc human leukocyte antigen compatibility not huge factor -quality of organ higher bc shorter ischemic time and more thorough medical screening ● Ethical Issues Regarding Live Donation ● Harm to Donors ● violate do no harm when operating on healthy person for another’s benefit ● risk injury, death, infection, pain, lost wages for donor ● persons can’t be living donor if have conditions that increase operative risk or impaired organ function ● Motives of Donors ● donation to fam/friends understandable ● donation to stranger raises ethical concerns either altruistic or driven by desire for publicity, financial gain, or psychological issues ● need to screen stranger donations carefully ● Consent from Donors ● decision needs to be of free will and informed ie know all the risks ● use of children raises concerns bc they cannot give consent for themselves and depend on others to protect their interest (extreme circumstances and approval from court should be sought) ● Payment to Donors ● similar to those above ● Confidentiality of Recipient ● the right of the donor to know if their organ is going to cancer pt w/ high chance of relapse, or alcoholic cirrhosis, HIV infection in which donor might feel condition brought about by recipients choices ● weight this against patient confidentiality of recipient ● Current System of Donation ● live donors undergo education and psychosocial evaluation ● some eligible donors might be facing familial pressure or internal pressure to donate against their will, dr can help potential donor by telling family they are not suitable w/o explanation Selection of Recipients ● Historical Background ● allocation decisions cannot be avoided bc o the limiting factor is lack of organs ● a fair allocation procedure needed to maintain public willingness to donate, it would ● ● be unfair to ask people to donate if there was no opportunity for them to receive one if needed Beneficience ● from utilitarian perspective, scarce organs should go to those that will receive greatest medical benefit ● relative outcomes include likelihood and duration of survival, quality of life ● poor adherence to medical regimens, substance abuse, lack of family support might compromise outcomes ● critics say these sentiments cloak biases against race, class, social status Justice ● Time on waiting list ● first come first serve not exact bc different stages of illness, proximity to regional transplantation networks ● richer pts may take better advantage ● Medical Need ● only pts meeting minimum clinical criteria may be placed on list ● need factor in determining order ie in liver, heart transplants those pts that would die w/o expedited intervention given priority over more stable pts ● cadaveric livers assigned according to Model for End-Stage Liver DIsease (MELD) system, where severity of illness scored based on lab tests and predicts risk of death while waiting ● Ability to pay ● Medicare pays for kidney transplants for all Americans ● uninsured need to raise money for other transplants ● allocating organs by ability to pay criticized as unfair to ask poor people to donate when poor and uninsured would not be eligible recipients ie if they see system favoring the wealthy ● Previous Transplantation ● success rate for 2nd transplantation significantly lower ● drs often feel loyalty to patients they have already begun to treat so want to keep at it ● critics contend this is an unwillingness to say enough is enough ● Citizenship ● some object to foreigners coming to US specifically for organ transplant ● though unfair to exclude foreign nationals who contribute to US economy and who would be asked to serve as donors themselves ● Geographic Location ● waiting times for liver transplant vary up to 5 fold depending on location ● thought is to nationalize organ allocation to those w/ greatest medical need ● this might resdistribute organs away from states that have done well to increase donations and the increased ischemic time might also worsen outcomes ● Ethnic Background ● african americans more likely to develop chronic renal failure than caucasians, but are less likely to receive kidney transplant ● less likely to be evaluated for transplantation, placed on waiting list, and to find donor ● point system for prioritizing cadaveric kidneys gives priority to HLA matching but this hurts african americans because of the prevalence of ABO and HLA makes it less likely that an african american could find a highly matched white donor. ● recent changes have put less weight in HLA and have increased AA access ● UNOS policy forbids consideration of gender, race, or social factors ● Differences in Allocating Various Organs -kidney, dialysis provides mode to increase survival time so can wait for high HLA match and that determines priority -liver, no such treatment and HLA match does not determine success so priority is given to most critical pt ● Patient Behaviors that cause Disease -noncompliant with immunosuppressives, alcoholics, smokers etc have arguments for and against regarding right to transplantation -alcoholism has genetic and environmental components that are beyond pts control so unfair to exclude them -pts need to be abstinent from alcohol for 6 mos prior to transplant, many times this allows their liver to recover anyway ● Directed Donation to Strangers case: advertising for an organ donor - liver cancer pt placed billboard ads asking for liver and received cadaveric liver specifically for him. he died 7 mos later. unclear of cause. this case shows the power of advertising and a mechanism for the wealthy to jump ahead in line since recipients can be specified. to address these concerns about fairness, proposals for publicly solicited organs must go to next person on waiting list unless recipient and donor have pre-existing relationship Selection of Recipients -kidney: $143000, liver $314000, heart $392000. follow up care also high. -cost-effectiveness questioned USA confronts looming organ-shortage crisis - Lancet article summary US organ shortage seen by many as a failure of the altruistic donation system in place. Some suggest cash incentives as a way to circumvent this, however critics view this as exploitation of the poor. Others suggest redefining brain death to include merely higher brain death which would then classify patients in permanent vegetative states or unconscious comas to be legally dead. This would likely be met with staunch opposition as evidenced by public uproar to recent right to life cases such as Terri Schiavo. Other means to increase organ pool is to allow IV drug users, ‘men who have sex w/ men’, and other high risk people to donate to recipients that are so terminal the risk of infection is nothing compared to the imminent organ failure. Consent for Organ Donation - Balancing Conflicting Ethical Obligations NEJM article summary Conflict between facilitating patients’ right to donate organs and obligation to ensure that the consent process is informed and voluntary. Promoting organ donation too much makes one lose sight that the donor is a dying person, not a bag of organs. Past ethical issues stemmed from life-sustaining treatments being administered solely to keep the patient alive until the local organ-procurement organization OPO could determine if the patient’s organs were suitable for donation, even if it was in opposition to advanced directives. These issues were resolved by amendments that called for the physician to consult w/ the pt or surrogate to determine and follow their wishes. Current problems exist because hospitals need to notify local OPO of individuals who have died in the hospital or whose deaths are imminent. The OPO representatives use a strategy known as the ‘presumptive approach for organ donation’ which is basically a high pressure technique to convince families to give up their loved one’s organs. It inherently undermines informed consent and seems to not respect a family’s decisions. While there certainly needs to be an increase in organ supply, a tactic that impairs the informed consent process does not seem to be ethically sound.