Original Article
Four-Limb Blood Pressure as Predictors of Mortality
in Elderly Chinese
Chang-Sheng Sheng, Ming Liu, Wei-Fang Zeng, Qi-Fang Huang, Yan Li, Ji-Guang Wang
Abstract―The predictive value of blood pressure (BP) for cardiovascular morbidity and mortality diminishes in the elderly,
which may be confounded and compensated by the BP differences across the 4 limbs, markers of peripheral arterial
disease. In a prospective elderly (≥60 years) Chinese study, we performed simultaneous 4-limb BP measurement using
an oscillometric device in the supine position, and calculated BP differences between the 4 limbs. At baseline, the mean
age of the 3133 participants (1383 men) was 69 years. During 4 years (median) of follow-up, all-cause and cardiovascular
deaths occurred in 203 and 93 subjects, respectively. In multiple regression analyses, arm BPs on the higher arm side of
systolic BP did not predict mortality (P≥0.06) except for a negative association between mean arterial pressure and total
mortality (P=0.04). However, in adjusted analyses, the hazard ratios associated with a 1-SD decrease in ankle-brachial
BP index or increase in interarm or interankle BP difference were 1.15 to 1.23 for total mortality (P≤0.01) and 1.17 to
1.24 for cardiovascular mortality (P≤0.04). In categorical analyses, similar results were observed for a decreased anklebrachial index (≤0.90, ≤0.95, or ≤1.00) or increased interarm or interankle difference (≥15 mm Hg or ≥10 mm Hg).
In conclusion, in the elderly, above and beyond arm BP level and together with ankle-brachial index, the interarm and
interankle BP differences improve prediction of mortality. Simultaneous 4-limb BP measurement has become feasible
with current technology and might be useful in cardiovascular prevention. (Hypertension. 2013;61:00-00.) Online
Data Supplement
•
Key Words: ankle-brachial index
■
Chinese ■ elderly ■ interankle blood pressure difference
■ interarm blood pressure difference ■ mortality
igh blood pressure (BP) is an established modifiable risk
factor for cardiovascular disease and mortality. However,
the association between BP and cardiovascular risk weakens
in the elderly.1 A major confounding factor is atherosclerotic
peripheral arterial disease (PAD).2,3 When PAD is present in
subclavian and brachial arteries, arm BP cannot be accurately
measured, and hypertension therefore cannot be timely diagnosed and properly managed in clinical practice.4,5
Current technology allows simultaneous BP measurement
in 4 limbs,6,7 which may provide a comprehensive evaluation
of BP and generate accurate BP differences between 4 limbs,
such as ankle-brachial BP index (ABI) and the interarm and
interankle BP differences. ABI is a well-documented diagnostic tool for PAD in lower extremities.8 The interarm BP
difference is also being recognized as an indicator of PAD
in the subclavian or brachial arteries.2–5,9–11 To the best of our
knowledge, the diagnostic and prognostic significances of the
interankle BP difference have not been investigated in prospective studies.
We performed simultaneous BP measurement in 4 limbs
in an elderly Chinese population, which was prospectively
followed up for mortality. In the present study, we investigated total and cardiovascular mortality in relation to the
level of arm BP, ABI, and the interarm and interankle BP
differences.
H
Methods
Study Population
Our study was conducted in the framework of the Chronic Disease
Detection and Management in the Elderly (≥60 years) Program supported by the municipal government of Shanghai. In a newly urbanized suburban town, 30 kilometers from the city center, we invited all
residents of 60 years or older to take part in comprehensive examinations of cardiovascular disease and risk. The Ethics Committee of
Ruijin Hospital, Shanghai Jiaotong University School of Medicine
approved the study protocol. All subjects gave written informed
consent.
A total of 3263 subjects (participation rate 90%) were enrolled
in the period from 2006 to 2008, and followed up for vital status
and cause of death till June 30, 2011. We excluded 130 subjects
from the present analysis, because 4-limb BP measurement was not
performed (n=45) or because of missing other information (n=85).
Thus, the number of participants included in the present analysis
was 3133.
Received December 28, 2012; first decision February 16, 2013; revision accepted March 12, 2013.
From the Centre for Epidemiological Studies and Clinical Trials, The Shanghai Institute of Hypertension, Ruijin Hospital, Shanghai Jiaotong University
School of Medicine, Shanghai, China.
The online-only Data Supplement is available with this article at http://hyper.ahajournals.org/lookup/suppl/doi:10.1161/HYPERTENSIONAHA.
111.00969/-/DC1.
Correspondence to Ji-Guang Wang, The Shanghai Institute of Hypertension, Ruijin 2nd Road 197, Shanghai 200025, China. E-mail
jiguangw@gmail.com
© 2013 American Heart Association, Inc.
Hypertension is available at http://hyper.ahajournals.org
DOI: 10.1161/HYPERTENSIONAHA.111.00969
1
Copyright by American Heart Association, Inc. All rights reserved.
2
Hypertension
June 2013
Four-Limb BP Measurements
Four-limb BP was measured by the use of the Vascular Profiler-1000
device (Omron, Kyoto, Japan), which operates the oscillometric technique and has been validated previously.6,7 Trained technicians and
physicians placed the pressure cuffs on both arms and both ankles
and performed the measurements, after the subject had rested for ≈10
minutes in the supine position. The device simultaneously and automatically measures the BPs twice, and then discards the first measurement and only stores the second one in the database.
ABI was reported by the device as the ratio of the lower ankle over
the higher brachial systolic BPs. For systolic and diastolic BPs separately, we calculated the interarm and interankle BP differences as the
absolute value of the difference between the right and left brachial
BPs and between the right and left ankle BPs, respectively. Pulse
pressure was the difference between systolic and diastolic BPs. Mean
arterial pressure was two-thirds diastolic pressure plus one-third systolic pressure.
Filed Work
One experienced physician measured each participant’s BP 3× consecutively using a validated Omron 7051 oscillometric BP monitor
(Omron, Kyoto, Japan) on the nondominant arm, after the subjects
had rested for ≥5 minutes in the sitting position. The same observer
also administered a standardized questionnaire to collect information
on medical history, lifestyle, and use of medications. Hypertension
was defined as a sitting BP (average of 3 readings) of ≥140 mm Hg
systolic or 90 mm Hg diastolic or as the use of antihypertensive drugs,
unless the interarm difference of BP measured in the supine position
was ≥10 mm Hg (n=285). In the latter case, hypertension was defined
according to supine BP on the higher arm side and the same diagnostic thresholds. A trained technician performed anthropometric measurements. Venous blood samples were drawn after overnight fasting
for the measurement of plasma glucose, serum total cholesterol, and
triglycerides. Diabetes mellitus was defined as a plasma glucose concentration of ≥7.0 mmol/L fasting or 11.1 mmol/L at any time or as
the use of antidiabetic agents.
During follow-up, information on vital status and the cause of death
was obtained from the official death certificate, with further confirmation by the local Community Health Center and family members
of the deceased people. The International Classification of Diseases
9th Revision was used to classify the cause of death. Cardiovascular
mortality included deaths attributable to stroke, myocardial infarction, and other cardiovascular diseases.
Statistics
For database management and statistical analysis, we used SAS software (version 9.13, SAS Institute, Cary, NC). Means and proportions
were compared with the Student t test and Fisher exact test, respectively. Multiple Cox regression analysis was performed to compute
hazard ratios with their 95% confidence intervals (CIs). The logrank test was used to compare the cumulative incidence of mortality between groups with Kaplan–Meier survival function to show the
time to death. In continuous analyses, we analyzed the BP indexes
for both systolic and diastolic BPs, except ABI that was only calculated for systolic BP. In categorical analyses, we defined reduced ABI
(≤0.90,12 ≤0.95,13 or ≤1.0014) and increased interarm and interankle
BP differences (≥15 mm Hg or ≥10 mm Hg4,9) according to systolic
BP only, and used various cutoff limits according to the current guidelines12 or otherwise the literature.4,9,13,14 We plotted time-dependent–
operating characteristics curves and calculated the c statistic with CIs
to examine the incremental prognostic value for mortality.15 We also
evaluated the overall improvement in reclassification of subjects by
the net reclassification improvement method.16
Results
Characteristics of the Study Participants
At baseline, the 3133 participants (1383 [44.1%] men) had a
mean (±SD) age of 69.0±7.4 years and included 1895 (60.5%)
and 285 (9.2%) patients with hypertension and diabetes mellitus, respectively. Table 1 shows the baseline characteristics
by sex.
Continuous Analyses
During 4.0 years (median) of follow-up, the cumulated number
of person-years was 12 800, and all-cause and cardiovascular
deaths occurred in 203 and 93 subjects, respectively. In multiple Cox regression analyses adjusted for age, sex, body mass
index, current smoking, alcohol intake, use of antihypertensive drugs, diabetes mellitus, and serum total cholesterol, brachial BP on the higher arm side of systolic BP did not predict
mortality (P≥0.06) except for a negative association between
mean arterial pressure and total mortality (P=0.04; Table S1
in the online-only Data Supplement). However, the BP ratios
and differences across the 4 limbs significantly predicted total
(P≤0.01) and cardiovascular mortality (P≤0.04; Table 2). The
hazard ratios associated with each 1-SD decrease in ABI or
increase in the interarm or interankle BP difference were 1.15
to 1.23 for total mortality and 1.17 to 1.24 for cardiovascular
mortality.
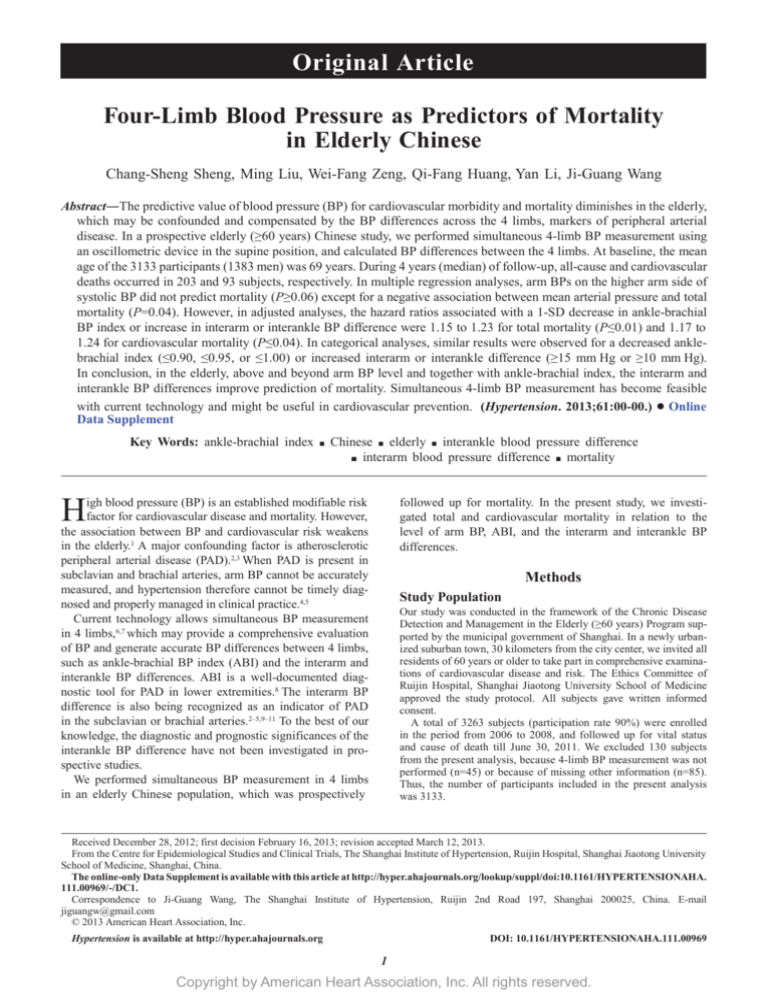
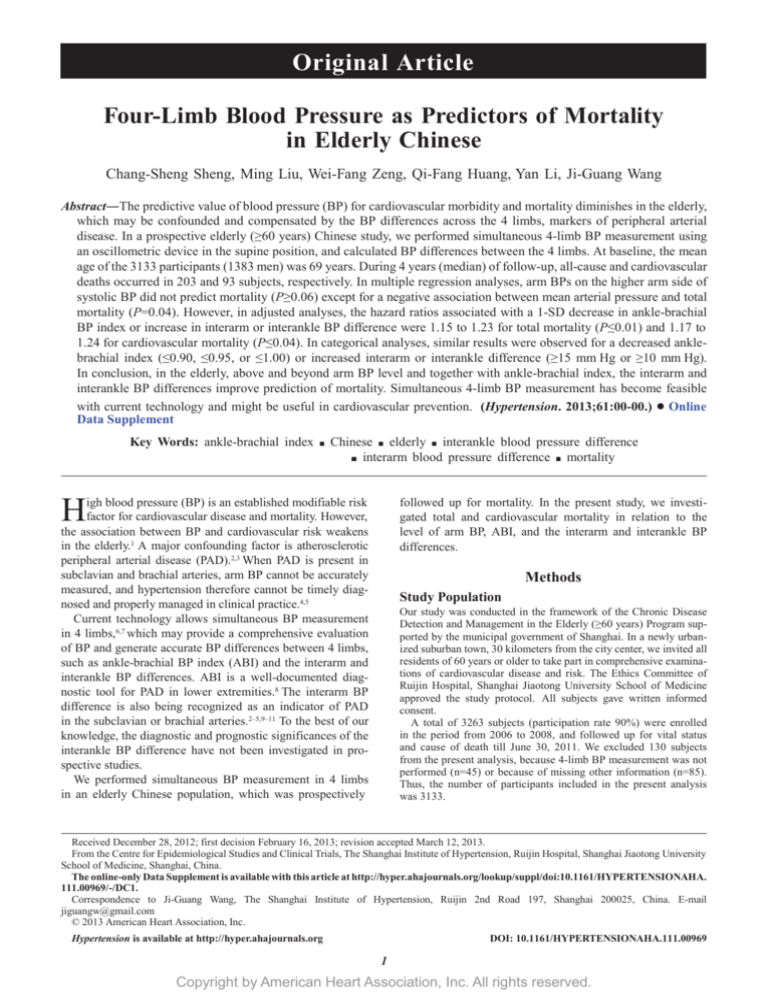
Categorical Analyses
The categorical analyses showed a curvilinear relationship
between the BP ratios and differences across the 4 limbs and
mortality (Figure 1), with a significantly higher incidence rate
of total mortality in the presence of a reduced ABI (≤0.90,
≤0.95, or ≤1.00) or greater interarm or interankle difference
(≥10 mm Hg or ≥15 mm Hg; Figure 2). After adjustment for
the abovementioned covariates and for the brachial BP, multiple Cox regression analyses were confirmatory (Table 3).
The hazard ratios ranged from 1.52 to 2.47 for total mortality (P<0.0001–0.02) and from 1.45 to 2.12 for cardiovascular
mortality (P values from 0.006 to 0.27).
C-Statistics and Reclassification Analyses
We calculated the c-statistic to estimate the incremental prognostic value of the interarm and interankle differences beyond
an ABI of ≥0.90 (Table S2). An interankle BP difference of
≥15 mm Hg alone or in combination with an interarm BP difference of 15 mm Hg significantly (P<0.001) increased the
prognostic value for total (c-statistic from 0.54 to 0.59 or to
0.60, respectively) and cardiovascular mortality (c-statistic
from 0.56 to 0.62 or to 0.63, respectively). However, an interarm BP difference of ≥15 mm Hg alone did not increase the
prognostic value (P≥0.46).
Reclassification analysis was confirmatory. Net reclassification improvement for an interankle BP difference of ≥15
mm Hg was significantly (P<0.001) positive for total (0.14;
95% CI, 0.08–0.20) and cardiovascular mortality (0.20; 95%
CI, 0.10–0.30).
Sensitivity Analyses
After exclusion of 83 persons with an ABI of ≤0.90, we
performed sensitivity analysis on the interarm and interankle
systolic BP differences. Similar trends and size of estimations
for association were observed. However, because of the
substantial reduction in the number of deaths, the association
remained statistically significant only for the interankle BP
Copyright by American Heart Association, Inc. All rights reserved.
Sheng et al
Table 1.
by Sex
Baseline Characteristics of the Study Participants
Characteristics
Age, y
Body mass index, kg/m
2
Men
(n=1383)
Women
(n=1750)
68.5±7.2
69.3±7.5‡
23.4±3.4
23.8±3.7‡
Simultaneous 4-limb BP measurement, mm Hg
Systolic pressure in left arm
134.5±18.3
138.9±19.9§
Diastolic pressure in left arm
80.8±10.2
78.5±10.2§
Systolic pressure in right arm
134.8±18.3
139.7±20.0§
Diastolic pressure in right arm
80.9±10.0
79.0±10.1§
Systolic pressure in left ankle
153.0±24.6
154.6±23.7
Diastolic pressure in left ankle
78.0±10.4
76.6±9.6§
Systolic pressure in right ankle
154.3±24.0
155.2±23.6
Diastolic pressure in right ankle
77.3±10.2
75.5±9.7§
BP on the higher arm side of systolic BP, mm Hg
Systolic pressure
136.5±18.6
141.3±20.2§
Diastolic pressure
81.5±10.1
79.5±10.1§
Pulse pressure
55.0±12.7
Mean arterial pressure
99.8±12.1
61.7±13.9§
100.1±12.7
Ankle-brachial systolic BP index
Mean±SD
1.10±0.10
1.07±0.08§
≤0.90, n (%)
40 (2.9)
43 (2.5)
≤0.95, n (%)
73 (5.3)
102 (5.8)
≤1.00, n (%)
141 (10.2)
276 (15.8)§
Interarm BP difference, mm Hg
Systolic pressure, mean±SD
3.71±3.67
3.89±3.84
Diastolic pressure, mean±SD
3.13±3.15
3.23±3.00
Systolic pressure, ≥15 mm Hg, n (%)
18 (1.3)
37 (2.1)
Systolic pressure, ≥10 mm Hg, n (%)
76 (5.6)
123 (7.0)
Interankle BP difference, mm Hg
Systolic pressure, mean±SD
6.54±6.72
6.26±6.15
Diastolic pressure, mean±SD
3.47±3.99
3.54±3.51
Systolic pressure, ≥15 mm Hg, n (%)
113 (8.2)
134 (7.7)
Systolic pressure, ≥10 mm Hg, n (%)
284 (20.5)
361 (20.6)
Use of antihypertensive drugs, n (%)
513 (37.3)
705 (40.4)
Diabetes mellitus, n (%)*
107 (7.8)
178 (10.2)†
Current smoking, n (%)
750 (55.1)
38 (2.2)§
Alcohol intake, n (%)
503 (37.1)
21 (1.2)§
Serum total cholesterol, mmol/L
5.51±1.42
5.68±1.41§
Values are mean±SD or numbers of subjects (%). BP indicates blood
pressure.
*For the definition of diabetes mellitus, see Methods.
†P<0.05; ‡P<0.01; §P<0.001 vs men.
difference (P≤0.03) but not for the interarm BP difference
(P≥0.17; Table S3).
We also performed sex-based sensitivity analysis and
found similar results in both sexes. For instance, the hazard
ratio (95% CI) for total mortality associated with an ABI of
≤1.00 or an interarm or interankle difference of ≥10 mm Hg
was 2.13 (1.36–3.33), 1.45 (0.71–2.97), and 1.57 (1.03–2.39),
respectively, in men and 1.79 (1.14–2.82), 2.06 (1.05–4.02),
and 1.46 (0.92–2.30), respectively, in women.
Four-Limb Blood Pressure and Mortality
3
Discussion
Our key finding is that in the elderly, the predictive value of
arm BP level is limited, ABI provides additional predictive
value, and above and beyond, the interarm and interankle BP
differences improve prediction of mortality. Four-limb BP
measurement might be therefore useful for cardiovascular
prediction and prevention in the elderly. Moreover, 4-limb
BP measurement, by demonstrating BP ratios and differences
across the 4 limbs, can be used as a diagnostic investigation
in placing an individual in a cardiovascular disease group
and at high-cardiovascular risk. This is apparently beyond
recording a brachial BP, which only provides a measure for
a validated risk stratification tool, such as the Framingham
Risk Score.17 However, this diagnostic capacity of BP ratios
and differences, especially ABI (recommended by current
guidelines),12 might immediately give a patient an opportunity
for lifestyle and pharmacological interventions, and hence
weaken the studied associations, which is irremediable by any
statistical adjustment.
To the best of our knowledge, our study is the first that
has demonstrated in the elderly independent and significant
prognostic value of interankle BP differences for mortality.
Despite that ABI has high sensitivity and specificity for the
diagnosis of PAD,18 the predictive value of increased interankle BP differences may still be related to lower extremities.
It is possible that an increased interankle BP difference detects
even milder arterial diseases in the lower extremities than
ABI. Nevertheless, other mechanisms cannot be excluded.
Our study is the first Chinese population-based prospective
study on the prognostic value of the interarm BP difference
and ABI for mortality. Our finding is in line with the results of
recent meta-analyses9,19 and the study of a cohort of Chinese
patients.20 In a meta-analysis of 4 studies, an interarm BP difference of ≥15 mm Hg was associated with a 60.0% and 70%
increase in total and cardiovascular mortality, respectively.9
Similarly, in a pooled analysis of 11 studies based on individual data, an ABI of ≤0.90 was associated with a 60.0% and
a 96% increase in total and cardiovascular mortality, respectively.19 In a Chinese study of patients with coronary heart
disease, stroke, end-stage renal disease, or diabetes mellitus,
an ABI of ≤0.90 was associated with a 53.4% and a 103.1%
increase in total and cardiovascular mortality, respectively.20
The prevalence of PAD in our current study is lower than
that of several previous studies in Chinese20,21 and other
populations.8,22,23 The diagnostic threshold of ABI for the
diagnosis of PAD might be an explanation. The Chinese might
require a higher threshold of ABI, for example, 0.95 instead of
0.90.13 The oscillometrically measured ABI might also require
a higher threshold, for example, 1.00 instead of 0.90.14 The
prevalence of the interarm BP difference of 10 or 15 mm Hg
or more in our current research is also lower than that of other
studies.24 Simultaneous measurement might have diminished
the interarm and interankle BP differences. In addition to these
technical explanations, ethnicity may play a role, especially
when the known risk factors for PAD are considered.22 In our
study, men had a much higher proportion of smokers but lower
prevalence of reduced ABI than women, although men had
slightly lower prevalence of diabetes mellitus.
Copyright by American Heart Association, Inc. All rights reserved.
4
Hypertension
Table 2.
June 2013
Continuous Analyses on the Prognostic Significance of Blood Pressure Ratio and Differences Across the 4 Limbs
Total Mortality
Blood Pressure Ratio or Difference
Cardiovascular Mortality
Hazard Ratio (95% Confidence Interval)*
P Value
Hazard Ratio (95% Confidence Interval)*
P Value
1.22 (1.10–1.36)
0.0003
1.24 (1.07–1.44)
0.005
Systolic pressure, +3.76 mm Hg
1.16 (1.04–1.30)
0.01
1.18 (1.01–1.40)
0.04
Diastolic pressure, +3.07 mm Hg
1.17 (1.05–1.31)
0.005
1.23 (1.06–1.44)
0.006
Systolic pressure, +6.40 mm Hg
1.15 (1.05–1.27)
0.004
1.20 (1.06–1.36)
0.004
Diastolic pressure, +3.73 mm Hg
1.15 (1.06–1.24)
0.0009
1.17 (1.06–1.30)
0.002
Ankle-brachial systolic blood
pressure index, −0.09
Interarm blood pressure difference
Interankle blood pressure difference
*Hazard ratios and their 95% confidence intervals were computed for each 1-SD decrease in ankle-brachial blood pressure index or increase in interarm and
interankle blood pressure differences, with adjustments for age, sex, body mass index, current smoking, alcohol intake, use of antihypertensive drugs, diabetes mellitus,
and serum total cholesterol.
Although the prognostic significance of ABI and the interarm
and interankle BP differences are independent and additive, PAD
can still be a common explanation of association. PAD, especially
in the subclavian and brachial arteries, can also partially explain
the diminished predictive value of the conventionally measured
brachial BP in the elderly.2,3 When PAD is present in arteries
in the upper extremities, the reduced BP on the diseased arm
would not only possibly delay the diagnosis of hypertension,
but also lead to inappropriate management of hypertension.4,5
Nonetheless, there is no direct radiological evidence for plaques
in the interarm or interankle BP differences of 10 or 15 mm Hg
or more.9 Imaging studies are required.
Our study should be interpreted within the context of its
limitations. First, our study had a relatively short duration of
follow-up and small number of events, which may compromise the quantitative accuracy of the studied associations.
Second, the oscillometric technology, although validated in
technological6,7,25 as well as outcome studies,26,27 might be
still prone for measurement errors, especially in patients with
incompressible arteries,28,29 and, depending on the level of
ABI, might slightly differ from the manual Doppler technique
in the measurement of ABI values.7 Moreover, this technology
operates on a dedicated device, which is not cheap compared
with existing equipments, such as the Doppler devices, and
hence can be a barrier to its wide use as a clinical tool. Third,
although we emphasize the importance of simultaneous measurement of 4-limb BPs, the clinically used 2-limb devices
may be equally effective in the measurement of BP ratios or
differences across the 4 limbs. Finally, a single measurement
might be less accurate than multiple repeated measurements.
Nonetheless, our previous reproducibility study has shown
that as far as the BP ratio or difference is concerned, the intersession variation is small.7
In conclusion, in the elderly, the predictive value of the
level of arm BP for mortality is limited. ABI provides additional predictive value. Above and beyond, the interarm and
interankle BP differences improve prediction of mortality.
Simultaneous 4-limb BP measurements have become feasible
with current technology and might be useful in cardiovascular
prevention, especially in the elderly.
Figure 1. Incidence rate of total and cardiovascular mortality. Open and closed circles represent total and cardiovascular mortality,
respectively, according to quartiles of ankle-brachial systolic blood pressure index (left) and the interarm (middle) and interankle systolic
blood pressure differences (right). The number of deaths and subjects is given alongside the symbols and at the bottom, respectively. P
values for trends of each group are given.
Copyright by American Heart Association, Inc. All rights reserved.
Sheng et al
Four-Limb Blood Pressure and Mortality
5
Figure 2. Kaplan–Meier survival
curve for total mortality.
Kaplan–Meier survival curve
for total mortality was stratified
by ankle-brachial systolic
blood pressure index (>0.9 vs
≤0.9 and >0.95 vs ≤0.95, left)
and the interarm (<15 vs ≥15
mm Hg and <10 vs ≥10 mm Hg,
middle) and interankle systolic
blood pressure differences
(<15 vs ≥15 mm Hg and <10 vs
≥10 mm Hg, right). A P value
by the log-rank test is given for
each comparison.
Perspectives
In the elderly, PAD is prevalent. With increasing longevity, there
would be a huge number of patients with this disease. Simultaneous
4-limb BP measurements may identify these patients, unidentified
by the use of ABI alone, and hence might be used for the screening
of patients with PAD. Nonetheless, imaging studies are required
to investigate the arterial structural characteristics of patients with
abnormal interarm or interankle BP differences.
Acknowledgments
We gratefully acknowledge the voluntary participation of all study
subjects and the technical assistance of the physicians and nurses of
Table 3.
Zhaoxiang Community Health Center (Qingpu District, Shanghai)
and the expert assistance of Jie Wang, Li Zheng, Wei-Zhong Zhang,
and Yi Zhou.
Sources of Funding
The present study was financially supported by grants from the
National Natural Science Foundation of China (30871360, 30871081,
81170245, and 81270373), the Ministry of Science and Technology
(a grant for China-European Union collaborations [1012]) and
the Ministry of Education (NCET-09-0544), Beijing China, the
Shanghai Commissions of Science and Technology (11QH1402000)
and Education (the Dawn project 08SG20), the Shanghai Bureau
of Health (2009Y111 and XBR2011004), and Shanghai Jiaotong
Categorical Analyses on the Prognostic Significance of Blood Pressure Ratio and Differences Across the 4 Limbs
Total Mortality
Blood Pressure
Ratio or Difference
No. of Events/Patients on Risk
(Rate per 1000 Person-years)
Cardiovascular Mortality
Hazard Ratio (95%
Confidence Interval)*
P Value
No. Events/Patients on Risk (Rate
per 1000 Person-years)
Hazard Ratio (95%
Confidence Interval)*
P Value
Ankle-brachial systolic blood pressure index
≤0.90 vs >0.90
22/83 (65.9)
2.02 (1.24–3.30)
0.005
13/83 (38.9)
1.70 (0.86–3.39)
0.13
≤0.95 vs >0.95
39/175 (55.8)
2.23 (1.52–3.26)
<0.0001
22/175 (31.5)
2.12 (1.24–3.64)
0.006
≤1.00 vs >1.00
64/417(38.3)
1.92 (1.39–2.66)
<0.0001
31/417 (19.4)
1.74 (1.09–2.80)
0.02
Interarm systolic blood pressure difference, mm Hg
≥10 vs <10
21/199 (25.5)
1.72 (1.06–2.80)
0.02
9/199 (10.9)
1.45 (0.70–3.00)
0.27
≥15 vs <15
9/55 (40.3)
2.47 (1.24–4.93)
0.01
4/55 (17.9)
2.11 (0.75–5.96)
0.17
Interankle systolic blood pressure difference, mm Hg
≥10 vs <10
73/645 (28.1)
1.52 (1.16–2.06)
0.008
42/645 (16.2)
1.75 (1.12–2.74)
0.01
≥15 vs <15
40/244 (41.8)
1.63 (1.12–2.38)
0.01
26/244 (27.5)
1.89 (1.13–3.18)
0.02
*Hazard ratios and their 95% confidence intervals were computed for patients at risk vs the rest of study participants in a Cox regression model adjusted for age,
sex, body mass index, current smoking, alcohol intake, use of antihypertensive drugs, diabetes mellitus, serum total cholesterol, and arm systolic and diastolic blood
pressures on the higher arm side of systolic blood pressure.
Copyright by American Heart Association, Inc. All rights reserved.
6
Hypertension
June 2013
University School of Medicine (a grant of Distinguished Young
Investigators to Y. Li).
Disclosures
J.-G. Wang reports receiving grants and lecture and consulting fees
from Omron Healthcare (Kyoto, Japan). The other authors have no
conflicts to report.
References
1. van Bemmel T, Gussekloo J, Westendorp RG, Blauw GJ. In a populationbased prospective study, no association between high blood pressure and
mortality after age 85 years. J Hypertens. 2006;24:287–292.
2. Clark CE. Difference in blood pressure between arms might reflect
peripheral vascular disease. BMJ. 2001;323:399–400.
3. Aboyans V, Criqui MH, McDermott MM, Allison MA, Denenberg JO,
Shadman R, Fronek A. The vital prognosis of subclavian stenosis. J Am
Coll Cardiol. 2007;49:1540–1545.
4. Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood
pressure readings between arms and survival: primary care cohort study.
BMJ. 2012;344:e1327.
5. Lane D, Beevers M, Barnes N, Bourne J, John A, Malins S, Beevers DG.
Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens. 2002;20:1089–1095.
6. Cortez-Cooper MY, Supak JA, Tanaka H. A new device for automatic
measurements of arterial stiffness and ankle-brachial index. Am J Cardiol.
2003;91:1519–22, A9.
7. Pan CR, Staessen JA, Li Y, Wang JG. Comparison of three measures of the
ankle-brachial blood pressure index in a general population. Hypertens
Res. 2007;30:555–561.
8. Ankle Brachial Index Collaboration. Ankle brachial index combined with
Framingham Risk Score to predict cardiovascular events and mortality: a
meta-analysis. JAMA. 2008;300:197–208.
9. Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of
a difference in systolic blood pressure between arms with vascular disease and
mortality: a systematic review and meta-analysis. Lancet. 2012;379:905–914.
10. Clark CE, Campbell JL, Powell RJ. The interarm blood pressure difference as predictor of cardiovascular events in patients with hypertension in
primary care: cohort study. J Hum Hypertens. 2007;21:633–638.
11. Agarwal R, Bunaye Z, Bekele DM. Prognostic significance of betweenarm blood pressure differences. Hypertension. 2008;51:657–662.
12. Rooke TW, Hirsch AT, Misra S, Sidawy AN, Beckman JA, Findeiss LK,
Golzarian J, Gornik HL, Halperin JL, Jaff MR, Moneta GL, Olin JW,
Stanley JC, White CJ, White JV, Zierler RE. 2011 ACCF/AHA focused
update of the guideline for the management of patients with peripheral
artery disease (updating the 2005 guideline): a report of the American
College of Cardiology Foundation/American Heart Association Task
Force on Practice Guidelines. Circulation. 2011;124:2020–2045..
13. Guo X, Li J, Pang W, Zhao M, Luo Y, Sun Y, Hu D. Sensitivity and
specificity of ankle-brachial index for detecting angiographic stenosis of
peripheral arteries. Circ J. 2008;72:605–610.
14. Verberk WJ, Kollias A, Stergiou GS. Automated oscillometric determination of the ankle-brachial index: a systematic review and meta-analysis.
Hypertens Res. 2012;35:883–891.
15. Chambless LE, Diao G. Estimation of time-dependent area
under the ROC curve for long-term risk prediction. Stat Med.
2006;25:3474–3486.
16. Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating
the added predictive ability of a new marker: from area under the ROC
curve to reclassification and beyond. Stat Med. 2008;27:157–172; discussion 207.
17. Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J. 1991;121(1 pt 2):293–298.
18. Ouriel K, McDonnell AE, Metz CE, Zarins CK. Critical evaluation of
stress testing in the diagnosis of peripheral vascular disease. Surgery.
1982;91:686–693.
19. Heald CL, Fowkes FG, Murray GD, Price JF; Ankle Brachial Index
Collaboration. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: systematic review. Atherosclerosis.
2006;189:61–69.
20. Li X, Luo Y, Xu Y, Li J, Hu D. Relationship of ankle-brachial index
with all-cause mortality and cardiovascular mortality after a 3-year
follow-up: the China ankle-brachial index cohort study. J Hum Hypertens.
2010;24:111–116.
21. Woo J, Lynn H, Wong SY, Hong A, Tang YN, Lau WY, Lau E, Orwoll E,
Kwok TC. Correlates for a low ankle-brachial index in elderly Chinese.
Atherosclerosis. 2006;186:360–366.
22. Meijer WT, Grobbee DE, Hunink MG, Hofman A, Hoes AW. Determinants
of peripheral arterial disease in the elderly: the Rotterdam study. Arch
Intern Med. 2000;160:2934–2938.
23. Weatherley BD, Nelson JJ, Heiss G, Chambless LE, Sharrett AR, Nieto
FJ, Folsom AR, Rosamond WD. The association of the ankle-brachial
index with incident coronary heart disease: the Atherosclerosis Risk
In Communities (ARIC) study, 1987-2001. BMC Cardiovasc Disord.
2007;7:3.
24. Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic
review. J Hum Hypertens. 2006;20:923–931.
25. Beckman JA, Higgins CO, Gerhard-Herman M. Automated oscillometric
determination of the ankle-brachial index provides accuracy necessary for
office practice. Hypertension. 2006;47:35–38.
26. Morimoto S, Yurugi T, Aota Y, Sakuma T, Jo F, Nishikawa M, Iwasaka T,
Maki K. Prognostic significance of ankle-brachial index, brachial-ankle
pulse wave velocity, flow-mediated dilation, and nitroglycerin-mediated
dilation in end-stage renal disease. Am J Nephrol. 2009;30:55–63.
27. Kitahara T, Ono K, Tsuchida A, Kawai H, Shinohara M, Ishii Y, Koyanagi
H, Noguchi T, Matsumoto T, Sekihara T, Watanabe Y, Kanai H, Ishida
H, Nojima Y. Impact of brachial-ankle pulse wave velocity and anklebrachial blood pressure index on mortality in hemodialysis patients. Am J
Kidney Dis. 2005;46:688–696.
28. Clairotte C, Retout S, Potier L, Roussel R, Escoubet B. Automated anklebrachial pressure index measurement by clinical staff for peripheral arterial disease diagnosis in nondiabetic and diabetic patients. Diabetes Care.
2009;32:1231–1236.
29. Diehm N, Dick F, Czuprin C, Lawall H, Baumgartner I, Diehm C.
Oscillometric measurement of ankle-brachial index in patients with suspected peripheral disease: comparison with Doppler method. Swiss Med
Wkly. 2009;139:357–363.
Novelty and Significance
What Is New?
•
Simultaneous 4-limb blood pressure measurement allows accurate assessment of ankle-brachial blood pressure index and interarm and interankle blood pressure differences. These blood pressure–derived indexes
are complementary in the prediction of mortality in the elderly.
What Is Relevant?
•
In the elderly, peripheral arterial disease is prevalent and predicts cardiovascular disease and mortality. The interarm and interankle blood
pressure differences, above and beyond ankle-brachial blood pressure
index, may improve prediction of mortality.
Summary
In the elderly, the predictive value of arm blood pressure level is
limited, ankle-brachial index provides additional predictive value,
and above and beyond, the interarm and interankle blood pressure
differences improve prediction of mortality.
Copyright by American Heart Association, Inc. All rights reserved.