Infections in Transplant recipients
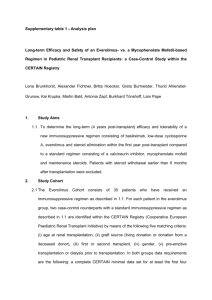
advertisement

Infections in Transplant recipients Infections following transplantation are complicated by the use of drugs that are necessary to enhance likelihood of survival of the transplanted organ but also cause the host to be immunocompromised. Variety of organisms have been transmitted by organ transplantation (see table 117-1) From 2% to >20% of donor kidneys are contaminated with bacteria – in most cases, with the organisms that colonize the skin or grow in the tissue culture medium used to bathe the donor kidney while it awaits implantation. Use of enrichment columns and monoclonal-antibody depletion procedures results in higher incidence of contamination. Approx 2% of cryopreserved and peripheral blood stem cells transfused as part of treatment for cancer are contaminated. Results of cultures performed at the time of cryopreservation and at the time of thawing were helpful in guiding therapy for the recipient. In many transplantation centers, transmission of infections that may be latent or clinically inapparent in the donor organ has resulted in the development of specific-donor screening protocols. Serologic testing focusing on such viruses such as HSV 1 and HSV 2; VZV, CMV, HHV 6, EBV, HHV-8, hepaB and C, HIV, HTLV -1 and on parasites such as Toxoplasma gondii, skin testing for M. tuberculosis. Investigation of patients dietary habits (consumption of raw meat or fish or unpasteurized products) , occupations or avocations (gardening or spelunking), and travel history (travel to areas with endemic fungi) is mandatory. It is expected that the recipient will have been likewise assessed. INFECTIONS IN BONE MARROW AND HEMATOPIETIC STEM CELL TRANSPLANT RECIPIENTS BM or hematopoeitic stem cell transplantation for either immunodeficiency or cancer patients results in a transient state of complete immune incompetence. Immediately after transplantation, both phagocytes and immune cells (T&B cells) are absent, and the host is extremely susceptible to infection. BACTERIAL INFECTIONS. 1st month bm or hematopoietic stem cell transplantation, infectious complications are similar to those in granulocytopenic patients receiving chemotherapy for acute leukemia. 1-4 week – due to anticipated neutropenia and high rate of bacterial infection in this population, many centers give prohyplactic antibitiocs to patients upon initiation of chemotherapy. LEVOFLOXACIN – decrease the incidence of gram- negative bacteremia among these patients Bacterial infections are common in first few days after BM transplant. Predominantly aerobic bacteria found in the bowel ( Pseudomonas, E.coli, Klebsiella) and those found in the skin or in intravenous catheters (S. aureus and coagulasenegative staph) Filamentous bacteria (Nocardia and organisms that cause actinomycosis) beyond 1st few days of neutropenia Episodes of bacteremia due to encapsulated organisms marked the late post transplantation period (>6 months after BM reconstitution). FUNGAL INFECTIONS beyond 1st week after transplantation, become increasingly common. Candida albicans most common in granulocytopenic patients Candida glabrata & aspergillus increased used of prophylactic fluconazole; resistant fungi Candida % aspergillus in patients with GVHD who required prolonged or indefinite coursed of glucocoticoids and immunospressive agents, high risk even after engraftment and resolution of neutropenia. High risk of reactivation of fungal infection (Histoplasmosis, Blastomycosis, Coccidiodomycosis) – endemic areas. PARASITIC INFECTIONS Pneumocystis pneumonia (especially among patients being treated for hematologic malignancies) most patients receive maintenance prophylaxis TMP-SMX (trimethroprim-sulfamethoxazole starting 1 month after engraftment and continuing for at least 1 year. TMP-SMX- may also protect patients seropositive fo T. gondii which may cause pneumonia & CNS lesion advantage on maintenance daily for 1 yr after transplanatation include protection against Listeria monocytogenes and Nocardial disease as well as late infections with S. pneumoniae & H. influenzae which are consequence of the inability of immature BM to respond to polysaccharide antigens VIRAL INFECTIONS BMT/HSCT reciepents are susceptible to infection with variety of viruses, including reactivation syndrome caused by mist HHVS (Table 117-3) and infections caused by viruses that circulate in the community. HSV – Within 1st 2 weeks after transplantation HSV-1 from oropharynx prophylactic ACYCLOVIR (or VALACYCLOVIR) to seropositive BMT/HSCT recipients reduce mucositis and HSV pneumonia ( a rare condition reported exclusively in BMT recipients). Esophagitis due HSV-1 & anogenital disease HSV2 may be prevented with acyclovir prophylaxis VZV – Reactivation may occur in 1st month but more commonly after several months after transplantation. 40% in allogeneic patients and 25% for autlogous recipients. Disseminated disease could be controlled by ACYCLOVIR ( given prophylactic) to prevent sever disease. Low dose (400mg orally, TID) appear to be effective in preventing reactivation. However, it may also inhibit the dev’t of VZV-specific immunity. Thus administration for only 6 months after transplantation does not prevent zoster from occurring when treatment is stopped. Low dose for 1 year may be effective CMV – onset of CMV disease(interstitial pneumonia, BM suppression, or graft failure) usually comes betweedn 30 days and 90 days after transplantation, when granulocyte count is adequate but immunologic reconstitution has not occurred. it develops earlier than 14 days after transplantation may be evident as late as 4 months after the procedure. Great concern in the 2nd month after transplantation, particularly in BMT/HSCT recipients. In donor marrow is depleted of T cells – disease is manifested earlier aCD52 antibody (alentuzumab) prevent GVHD in nonmeloablative transplantation patients who receive gancyclovir (for prophylaxis, preemptive treatment, or treatment) may develop infection even later than 4 months after transplantation - - - - - - although CMV disease may present isolated fever, granulocyotpenia, or gi disease, the foremost cause of death from CMV infection in this setting is PNEUMONIA with the std use of CMV0negative filtered blood products, primary CMV infxn should be a risk in allogenic transplantation only when the donor is CMVseropositive and the recipient is CMV-seronegative. Reactivation or superinfection is common in CMV seropositive recipients and seropositice patients who undergo BM transplantation excrete CMV, with or without clinical findings Serious CMV disease is common among allogenic than autologous recipients and is often associated with GVHD. Finding of CMVin liver of a patient with GVHD does not necessarily mean that CMV iis responsible for hepatic enzyme abnormalities. MANAGEMENT: Prophylaxis Ganciclovir (or valganciclovir) abort CMV disease during the period of maximal vulnerability (from engraftment to day 120 after transplantation). Adverse effects: dose-related BM suppression (thrombocytopenia, leucopenia, anemia, and pancytopenia). Suppressive treatment – PCR evidence of CMV or urine cultures positive for CMV, entails unnecessary treatment of many individuals (on the basis of a lab test that is not highly predictive of disease) with drugs that have adverse effects. Treatment of CMV pneumonia in BMT/HSCT recipient requires both IVIg and ganciclovir. Foscarnet, for patients who cant tolerate ganciclovir, although it may produce nephrotoxicity and electroloyte imbalance. Transfusion of CMV-specific T-cells from the donor decreased viral load in small series of patients. HHV-6&7 - HHV-6 , cause of roseola in children, is a ubiquitous herpesvirus that reactivates (as determined by culture of the virus from the blood) in 50% of transplant patients between 2 and 4 weeks after surgery EBV appears to be asso with neutropenia, since, like CMV, this can be found in marrow cells although encephalitis developing after transplantation has been asso with HHV-6 in CSF,the causality of the association is not well defined. May be found in lung samples after transplantation susceptible to foscarnet ( and possibly to ganciclovir) - Primary EBV infection can be fatal to transplant recipients EBV reactivation can cause EBV-B cell lymphoproliferative disease (LPD), which may be fatal in patients taking immunospuppressive drugs. Marrow ablation that occurs as part of BMT/HSCT procedure may eliminate latent EBV from the host. Infection may be reacquired immediately after transplantation by transfer if infected donor B cells. Reactivation can occur in T-cell depleted autologous recipients (patients being given antibioses to T cells for treatment of a T-cell lymphoma with marrow depletion). EBV-LPD, becomes apparent as soon as 1 to 3 months after engraftment, causes high fever, and cervical lymphadenopathy resembling the symptoms of infectious mononucleosis but more commonly presents as an extranodal mass.. In all cases, EBV-LPD is more likely to occur with continued immnosuppression (especially that caused by the use of antibodies to T-cell and cyclosporine or other T-cell suppressive agents). 1st line treatment: Monoclonal anibody to CD20 (rituximab) for treatment of B cell lymphomas - Ganciclovir has been postulated to have activity on the basis of its ability to inhibit proliferation of B cells, but is asso with high toxicity. High-dose Ziduvidine – shows a promising effect for treatment of EBV positive CNS lymphomas Both interferon alpha and retinoic acid have been used As has IVIg HHV – 8 – EBV related gamma herpesvirus which is usually asso with Kaposi’s sarcoma, with primary effusion lymphoma, and sometimes with multicentric Castleman;s disease, has rarely resulted in disease in BMT/HSCT recipients. Other (nonherpes) virus – Both RSV and parainfluenza particularly type 3, can cause severe or fatal pneumonia in BMT recipients. Therapy with aerosolized ribavirin as well as RSV Ig or monoclonal ab to RSV(palivizumab) has been reported to lessen severity of RSV disease Influenza also occurs in BMT recipients and generally mirrors the presene of infection in the community. (amantadine/rimantadine, ribavirin?), but have limited effects, primarily reducing symptoms and shortening the duration of illness. Neuraminidase inhibitors (oseltamivir and zanamivir) are active against Influenza Typa A and B and are a reasonable treatment option. Adenovirus occurs in 1st or 2nd month after transplantation., is often asymptomatic. Parvovirus B19 (presenting as anemia, or occasionally as pancytopenia) can be treated with IVIg and enterovirus can occur and being treated with Pleconaril, a capsid binding agent. Rotavirus are common cause of gastroenteritis in BMT/HSCT recipients. Polyomavirus BK is found at high titers in the urine of patients who are highly immunosuppressed. BK viruria may be asso with hemorrhagic cystitis. PML by JC virus is rare among BMT/HSCT recipients compared with the rate among patients with impaired T cell function due to HIV infection. INFECTIONS IN SOLID ORGAN TRANSPLANT RECIPIENTS Organisms that cause infections in recipients of solid organt transplant recipients are different from those that infect BMTHSCT because solid organ recipients do not go through neutropenia. As the transplantation procedure involves surgery, however, solid organ recipients are subject to infections at anastomotic sites and to wound infections. Compared with BMT/HSCT, organ transplant patients are immunosuppressed for longer periods (often permanently). Thus they are susceptible to organisms as patients with chronic impaired T cell immunity. Early period (< 1month after transplantation),infections are most commonly due to extracellular bacteria ( staph, strep, e. coli and other gram-neg bacteria), which often originate in surgical wound or anastomotic sites. In subsequent weeks, consequences of the administration of agents that suppress cell-mediated immunity and of the acquisition or reactivation of virus and parasites become apparent. CMV infection – first 6 months HHV-6 reactivation – occurs within the 1st 2 to 4 weeks and may be asso with fever and granulocytopneia HHV6&7 – exacerbate CMV disease CMV – asso not only with generalized immunosuppression but also with organ specific, rejection-related syndromes, glomerulopathy in kidney transplant patients, bronchitis obliterans in lung transplant , vasculopathy in heart transplant, and vanishing bile duct in liver transplant. Beyond 6 months, infections characteristic of patients with defects in cell-mediated immunity – L. monocytogenes, Nocardia, various fungi and intracellular parasites. May be susceptible to EBV-LPD from as early as 2 months to many years after transplantation. The prevalence of this complication is increased by potent and prolonged used of T-cell suppressive drugs. Among organ transplant patients, those with heart and lung transplants- who receive most intensive immunosuppressive regimens- are most likely to develop EBV-LPD. KIDNEY TRANSPLANT Early infections often caused by bacteria asso with skin or wound infections. There is a role for perioperative antibiotic prophylaxis Cephalosporins to decrease risk of postoperative complications. UTI developing soon after transplantation are usually related to anatomical alterations resulting from surgery. UTI that occur >6 months after transplantation do not seem associated with high rate of pyelonephritis or relapse seen with infections that occur in 1st 3 months and may be treated in shorter periods. Prophylaxis with TMP-SMX for the 1st 4 months after transplantation decreases incidence of early and middle-period infections. Middle-Period infections predisposal to lung infection characteristic of those In patients with T-cell deficiency with intracellular bacteria, mycobacteria, nocardiae, fungi, viruses and parasites. 50% of all renal transplant recipients with fever in 1 to 4 months after transplantation has evidence of CMV disease. CMV may also present with athralgias or myalgias During this period, this infection may present as primary disease, or may present as reactivation or superinfection. Px may have atypical lmphocytosis. Unlike immunocompetent patients, however, they often do not have lyphadenopathy or splenomegaly. CMV may also cause glomerulopathy. Ig enriched with ab to CMV decreases incidence in group at higher risk (seronegative recipient of seropositive kidneys) Ganciclovir – useful prophylaxis and treatment of CMV disease Prophylacitv valacyclovir for the first 90 days after renal transplantations shows 50 % reduction in CMV disease and rejection at 6 months Herpes group infection become evident within 6 months of infection. HSV cause either oral or anogential lesions that are responsive to acyclovir. VZV may cause fatal disseminated infection in nonimmunie kidney transplant recipiens, but in imunie patients may cause reactivation zoster usually does not disseminate outside dermatome. HHV-6 may be reactivated and (usually asymptomatic) may be associated with fever, rash, suppression, encephalitis EBV reactivation disease is more serious; it may present as extranodal proliferation of B cells that invade the CNS, naspharynx, liver, small bowel, heart and transplanted kidneys. - - - Disease may regress once immunocompetence is restored. HHV-8 asoo with development of Kaposi’s sarcoma often appears within 1 year after transplantation, although the range is wide (1 month – 20 years) Papovavirus BK and JC have been cultured from the urine of kidney transplant recipients. The excretion kf BK virus is asso with urethral strictures Patients may develop pulmonary infections with Nocardia, Aspergillus, and Mucur as well as other intracellular organisms. In patients with IV catheter, L. monocytogenes is a common cause of bacteremia > 1 month after renal transplantation and should be seriously considered in recipients presenting with fever and headache. Salmonella bacteremia may lead to endovascular infections and require a prolonged therapy. Nocardia occur generally > 1 month after transplantation and may follow immunosuppressive treatment episode of rejection. May present as skin, bones, and lungs or in CNS in single or multiple abscesses. TMP-SMX is often efficacious. Late infections 6 months after kidney transplantation include CMV retinitis and a variety of CNS complication. Patients whose immunosuppression has been increased, are at high risk of Subacute meningitis due to Cryptococcus neoformans Listeria meningitis, acute and fatal “Transplant elbow” to patients who take glucocorticoids; a recurrent bacterial infection in and around the elbow that is thought to result from a combination of poor tensile strength of the skin of steroid-treated patients. Bouts of cellulites due to S. aureus Susceptible to Aspergillus and Rhizopus which may present as superficial lesions before dissemination M. marinum diagnosed by skin examination Protheteca wickerhamii by skin biopsy Warts caused BY HPV HEART TRANSPLANTATION Early infection Sternal wound infection and mediastinitis as early complication Common microbes in the skin are involved can also be due Mycoplasma hominis can be cured with a combination of surgical debridement (sometimes requiring muscle flap placement) plus clindamycin and tetracycline. Middle Period infections T. gondii TMP-SMX CMV – 1 to months after transplantation causes early signs and lab abnormalities (usually with fever and atypical lymphocytosis orleukopenia and thrombocytopenia) at 2 to 3 months, and produces severe disease (pneumonia) in 3 to 4 months. Ganciclovir is efficacious Late infections EBV infection usually present as a lymphoma-like proliferation of Bcells late after heart transplantation especially in patients on heavy immunosuppression. LUNG TRANSPLANTATION Early infection combination of ischemia and resulting mucosal damage together with accompanying denervations and lack of lymph drainage probably contributes to high rate of pneumonia. Prophylactic use od high doses broad spectrum antibiotics for first 3-5 days after surgery decreases incidence of pneumonia - Gram negative organisms (pseudomonas and enterobacteriaceae) are troublesome in first 2 weeks after surgery. It can also be caused by Candida, Aspergillus and Cryptococcus. Mediastinitis may occur at higher rate and most commonly develops within 2 weeks of surgery, Pneumonitis due to CMV usually present within 2 wekks and 3 months after surgery, with primary disease occurring later than reactivating disease. Middle-period infection 75 to 100% incidence of CMV infection. More than half has CMV pneumonia CMV can also cause bronchitis obliterans Ganciclovir is more active against CMV and also HSV. Prophlaxis is recommended. Late infections Incidence of Pneumocystisinfection is high among heart-lung recipients. TMP-SMX for 12 months after transplantation may be sufficient for 12 months after transplantation. EBV may cause either mononucleosis-like syndrome or LPD. The tendency of B cell blasts to present on lung appears to be greater after lung transplantation than after the transplantation of other organs. LIVER TRANSPLANTATION Early infections Administratioin of systemic broad-spectrum antibiotics for the first 5 days after surgery, even in the absence of documented infection, However, despite prophylaxis, infectious complications are common and are correlated with the duration of the surgical procedure and the type of biliary drainage. Operation lasting >12 hrs is asso with high likelihood of infection. Patients who have choledojejunostomy with drainage of the biliary dure to a Roux-en- Y jejunal bowel loop have more fungal infections thant those whose bile is drained via a choledochocholedochostomy with anastomosis of the donor common bile duct to the recipient common bile duct. Peritonitis and intraabdominal abscesses are common complications of liver transplantation. Bacterial peritonitis may result from biliary leaks and primary and secondary infection after leakage of bile. Abscesses within the 1st month after surgery may occur not only over the liver but also in the spleen, pericolic area and pelvis. treatmentL antibiotic and drainage as necessary Middle Period Infections development of postsurgical biliary stricture predisposes patients to cholangitis. These patients may lack the characteristic signs and symptoms of cholangitis: fever, abdominal pain and jaundice. Alternatively, may be present but suggests graft rejection. Invasive studies of biliary tract (either T-tube cholangiography or endoscopic retrograde cholangiopancreatography) may lead to cholangitis. For this reasons, prophylaxis with antibiotics covering gram – negative and anaerobes is recommeneded when these procedures are performed in liver transplant patients Reactivation of HepaB and C High dose Hepa B Ig to prevent Hepa B. Long term efficacy of lamivudive and aefovir in inhibiting hepa b viral replication after transplantation is being studied - Combination of interferon alpha and ribavirin is being tested for treatment /prophylaxis of Hepa C. CMV causes vanishing bile syndrome after liver transplantation PANCREAS TRANSPLANTATION To prevent contamination of the allograft with enteric bacteria and yeasts,some surgeons, instead of draining the pancreas through the bowel, drain secretions into urinary tract or bladder. Bladder drainage casuses a high rate or UTI and sterile cystitis. Prophylactic antimicrobials or transplantation of islet cells only as alternative. MISCELLANEOUS INFECTION IV catheter poses a risk of local and bloodstream infection, significant insertion-site-infection is most commonly caused by S. aureus. Coaugulase-neagative Staph are the most common isolates from the blood. Tuberculosis -Occurring within 12 months after solid organ transplantation. - It has been rarely transmitted from the donor organ. Virus-associated Malignancies transplant patients may develop nonmelanoma skin or lip cancers, that, in contrast to de novo skin cancers, have high ratio of squamous cells to basal cells. Among renal transplants, rates of melanoma are modestly increased and rates of ca of kidney and bladder are increased. VACCINATION OF TRANSPLANT RECIPIENTS recipients of allogenic BMTs must be reimmunized if they are to be protected against pathogens. In the absence of compelling data as to optimal timing, it is reasonable to administer pneumococcal and HiB conjugate vaccines to both autologous and allogenic BMT recipients 12 months after transplantation and again 12 months later. pneumococcal and HiB are important for patients whi have undergone splenectomy. N. meningitides polysaccharide vaccibe, diphtheria, tetanus, and inactivatedpolio vaccines can all be given at these same intervals (12 and 24 months after transplantation) Some authorities, recommend (12, 14 and 16 months after transplantation) Because of risk of spread, household contacts of BMT recipients should receive only inactivated polio vaccine. Live attenuated vaccines(MMR) can be given to autologous BMT recipients 24 months after transplantation and to most allogenic BMT recipients at the same point if they are receiving ,aintenance therapy with immunosuppressive drugs and do not have ongoing GVHD. Avoid all live-virus vaccines in patients who have GVHD and/or taking high maintenance dose of glucocorticoids. Solid organ transplant recipients all the usual vaccines and of the indicated booster doses should be completed before immunosuppression, if possible, to maximize responses. For taking immunosuppressive agents, the administration of pneumoccocal vaccine should be repeated every 5 years. H influenzae conjugate vaccine is safe and should be efficacious in this population; therefore, its administration is recommended. Person exposed to measles should receive Ig - Seronegative for Varicella and comes in contact with a person who has chicken pox should be given VZIg asap (and certainly within 96 hrs) or, if this is not possible, should be started immediately on a 10-14 day couese of acyclovir therapy. Susceptible household contacts should receive live vaccines - Immunocompromised patients who travel may benefit from some but not all vaccines. CHAPTER 117 INFECTIONS IN TRANSPLANT RECEPIENTS A. BONE MARROW TRANSPLANT INFECTIONS: 1st month of bone marrow transplant LEVOFLOXACIN: decreases bacteremia maong bone marrow transplant px 1st few days: common org: aerobic( E coli, klebsiella, Pseudomonas and thru skin or catheter ( Staph coag -/+) beyond 1st few days; Filamentous bacteria ( Nocardia/ Actininomyctes) Late posttransplant: encapsualted org (>6 months after BM reconstitution) beyond 1st week: fungal (candida) TMP-SMX- prophylactic for Pneumocystis; 1 month after engrafment and continiung for at least 1 year - prophylactic also for Toxoplasma, Listeria, Nocardia, Strep and haemophilus ACYCLOVIR: prophylactic for seropositve BMT/SCT; reduce mucositis and prevent HSV pneumonia : 2 wks after BMT excretion of virus of seropositve HSV 1 _ also good for Varicella- Zoster virus (low dose for the entire year) CMV: 30- 90 days after transplant: great concern on the 2nd month -assoc w/ used of alpha CD52 antibody among GVHD px -Ganciclovir- delay the devt of normal immune rsponse to CMV, not really protective - IVIg and Ganciclovir: tx for CMV pneumonia HHV-6 / Roseola- 2-4 wks after surgery: ? foscarnet EBV- fatal to transplant recepients -lymphopriliferative disease (LPD) - 1-3 months after engrfment - tx: ? EBV specific T cells; Rituximab , ganciclovir; zidovudine HHV -8 - Kaposi' s Sarcoma, primary effusion sarcoma, castle man RSV and Parainfluena- fatal pneumonia on BMT - tx: aerosolized Ribavirirn, RSV Ig ,Palivizumab Influenza- Oseltamivir and Zanamivir Rotavirus- gastoenteritis Polyomavirus BK- hemorrhagic cystitis B. SOLID ORGAN TRANSPLANT Early period( <1 month)- extracellular ( Staph, strep, e coli,) - origin : surgical wound or anostomotic sites CMV- 1st 6 months; sever systemic disease HHV 6 reactivation- w/in 1st 2 to 4 wks; fever and granulocytopenia CMV rejection related syndromes: - glomerulopathy- kidney -bronchilitis obliterans- lung transplant -vanishing bile duct syndrome- liver transplant Beyond 6 months: defects on CMI ( listeria , nocardia, fungi other intracellular org) EBV_LPD- 2 months to many years after transplant; heart and lung transplants 1) KIDNEY TRANSPLANTS -Early: due ti skin and wound infections; Tx: Cephalosporins -UTI- due to anatomical alterations from surgery (pyelonephritis)-longer duration of tx appear after 6 mos: shorter duration of tx -Prophylaxis: TMP-SMX -Middle period- lung infections w/ T-celldef( ICbacteria, nocardia, fungi, virus, parasite) -Legionella pnuemophilia- high mortality - CMV- 1 to 4 months -fever, glomerulopathy; tx: administer Ig w/ antibodies w/ CMV -EBV reactivation- extranodal prolif of B cells; invade CNS, nasopharynx, liver, small bowel heart and transplanted kidney -PAPOVAVIRUS:BK-nepropathy; JC virus- progressive multifocal leukoencephalopathy - L. monocytogenes- most common cause of bacteremia >= 1 month after renal transplantation -NOCARDIA- skin, bones, lungs and CNS, multiple abscess -Late infection (>6 months) - CMV retinitis, transplant ebow?, invasive fungal 2) HEART TRANSPLANTS -early: sternal wound infxn and mediastinitis -dx: sternal instability and failure to heal -middle: toxoplasmosis, CMV ,CNS infxn - late: EBV-lymphoma like 3) LUNG TRANSPLANTS -eearly: ischemia and mucosal damage, denervtion and lack of lymph drainage - prophylactic broad spectrum 1st 3 to 4 days antibiotics 4) LIVER TRANSPLANTS - infection on early; systemic broad spectrum antibiotic for the 1st 5 days - operation >12 hrs - inc incidence of infection -PERITONITIS and Intraabdominal Abscess- Common complication -Peritonitis- from biliary leak and primary or 2ndary infx,polymicrobil -Abscess- w/in 1st month, spleen, liver, pericolic and pelvis,Tx: antibiotic and drainage -middle: Cholangitis- devt postsurgical stricture on biliaryfever abdominla paina nd jaundice -Viral hepatitis- lamiduvine and adefovir for hepa B 5) Pancreas -infection prevented by draining pancreas to urinary tract or bladder INdwelling cathter- S. aureus- bloodstream infxn w/in a week Tuberculosis- w/in 12 months VACCINATION: For autologous and allogenic BMT recepients-(1 year and 2 years after) 1) pneumococcal -repeated every 5 years for px on immunosuppresants -every 3 years w/ significant exposure risk 2) H. Influenza type b conjugate vaccines Add: (12-14and 16 months after) 3) N. meningitides polysaccharide disease 4) diphtheia vaccines 5) tetanus vaccine 6) inactivated polio vaccine OTHERS: 7) Live virus MMR- BMT recepients 24 mos after transplant