ISMP Medication Safety Alert - Institute For Safe Medication Practices
advertisement

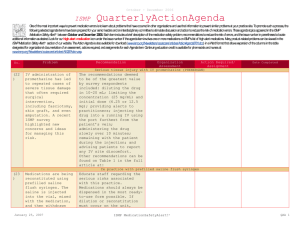
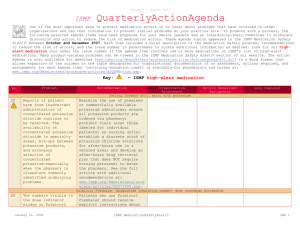
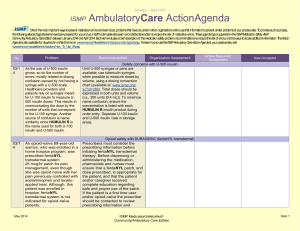
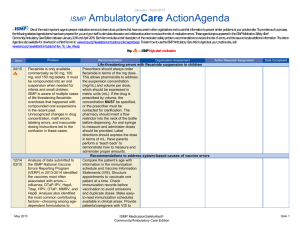
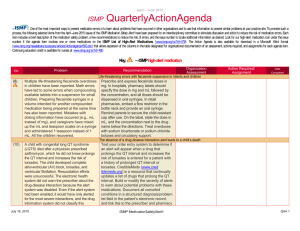
April – June 2011 ISMP QuarterlyActionAgenda Oneof themost important ways toprevent medication errors is tolearn about problems that haveoccurred in other organizations and tousethat information toprevent similar problems at your practicesite. To promotesuch aprocess, thefollowing selected items fromthe April-June2011 issues of theISMPMedication Safety Alert! havebeen prepared for an interdisciplinary committeetostimulate discussion and action toreducetherisk of medication errors. Each itemincludes a description of themedication safety problem, recommendations toreducetherisk of errors, and theissuenumber tolocateadditional information as desired. Look for our high-alert medication icon under theissuenumber if theagendaiteminvolves oneor moremedications on theISMPList of High-Alert Medications (www.ismp.org/Tools/highalertmedications.pdf). TheAction Agendais alsoavailablefor download in aWord format (www.ismp.org/Newsletters/acutecare/articles/ActionAgenda1103.doc) that allows expansion of thecolumns in thetabledesignated for organizational documentation of an assessment, actions required, and assignments for each agendaitem. Many product-related problems can alsobeviewed in theISMPMedication Safety Alert! section of our websiteat: www.ismp.org. Continuing education credit is availablefor nurses at: www.ismp.org/Newsletters/acutecare/actionagendas.asp. Key: Problem No. (13) (7, 8, 13) —ISMP high-alert medication Recommendation Organization Assessment Dosing confusion with colistimethate sodium for injection Action Required/ Assignment Date Completed ISMP and ASHP sent a warning Dose colistimethate sodium ONLY as through the National Alert Network colistin base, with a dosage reduction (NAN) about dosing errors involving for renal insufficiency. Consider colistimethate sodium for injection, a restricting ordering to infectious prodrug of colistin with a high disease specialists or intensivists. potential to induce nephrotoxicity and Use pre-approved guidelines or order neurotoxicity. The drug is used to sets with colistin base dosing only. treat multidrug-resistant organisms. Dose limits should be established with The strength of colistimethate sodium immediate investigation required for is labeled in terms of the colistin base, doses outside hospital guidelines. not the prodrug. Recently, a physician The full NAN alert can be accessed ordered the dose as the prodrug, but at: www.ismp.org/sc?k=nanalerts. the dose was dispensed as colistin base, which resulted in an overdose. Parenteral nutrition-related deaths and a cluster of bacterial endophthalmitis call for compounding pharmacy oversight Nineteen patients received The use of compounding pharmacies parenteral nutrition (PN) containing for com-plex solution preparation Serratia marcescens. Nine patients should not cease as a result of these died. All of the PN came from the outbreaks. Compounding pharmacies same compounding pharmacy. A are often better equipped to employ shortage of commercial amino acid and monitor compliance with USP solutions this winter led the <797>. Hospitals should use pharmacy to use amino acid commercially available solutions powder. A failure in the sterilization when possible. If solutions are process caused the contamination. outsourced, regularly monitor the Also, a cluster of bacterial external vendor using ASHP’s new endophthalmitis occurred related to Outsourcing Sterile Products intravitreal injections of Preparation: Contractor July 28, 2011 ISMP MedicationSafetyAlert! QAA 1 April – June 2011 ISMP Problem No. bevacizumab obtained from another compounding pharmacy. Not using masks, talking during preparation of the injections, and no vertical barrier were suspected to be sources of contamination. (9) Broselow Pediatric Antidotes for Chemical Warfare Tape (www.ismp.org/sc?k=broselow) resembles the Broselow Pediatric Emergency Tape. There could be confusion between the two tapes during a pediatric emergency. (11) A recent pharmacy compounding error involved a small volume injectable preparation in which a woman in labor received succinylcholine instead of ePHEdrine after a technician with multiple drugs under the hood during preparation of the medication syringes mixed up the two products. Another error involved an IV admixture in which an infant received a highly concentrated solution of sodium chloride after a technician pulled what he thought was a 250 mL bottle of sterile water to use as a base solution, but it was actually a bottle of 23.4% sodium chloride. (10) QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed Assessment Tool (www.ashpfoun dation.org/MainMenuCategories/ PracticeTools/SterileProductsTool.as px). Better FDA and licensing oversight for these pharmacies are also needed. Broselow tape for chemical warfare may be confused with the emergency tape Make staff aware that both tapes exist. Guard against confusion by underlining the words “Chemical Warfare” and storing this tape on carts in the emergency department only, in a different part of the cart than the emergency tape. Safe practices in pharmacy sterile compounding areas Limit in-house preparation of injectables and solutions to products not available commercially. Separate the storage of concentrated bulk solutions, particularly concentrated electrolytes, amino acids, and dextrose. Have a pharmacist pull the necessary ingredients prior to preparation to give to technicians. Use an automated compounder when possible. Place the ingredients of only one product under the hood at a time. Establish a standard procedure for verifying products, preferably checking additives before mixing high-alert medications. Final Acute Care Guidelines for Timely Administration of Scheduled Medications posted on ISMP website Nurses who responded to an ISMP ISMP has posted the final Acute Care survey made it clear that changes in Guidelines for Timely Administration the drug administration system have of Scheduled Medica-tions at: made the long-standing Centers for www.ismp.org/tools/guidelines/acute Medicare & Medicaid Services care/tasm.pdf. The guidelines July 28, 2011 ISMP MedicationSafetyAlert! QAA 2 April – June 2011 ISMP QuarterlyActionAgenda Problem Recommendation (CMS) “30-minute rule” error prone. Nurses reported taking shortcuts to comply with the rule, which have led to errors, some harmful. Examples include skipping pre-medication assessments and double checks, pre-pouring medications, borrowing medications, and failing to use available bar-coding technology. ISMP has been working towards documentation of what we believe represents best practices associated with timely administration of scheduled medications. suggest that hospitals should define a short list of time-critical scheduled medications that should be administered within 30 minutes of the scheduled time. For non-time-critical medications, administer daily, weekly, or monthly medications within 2 hours of the scheduled time, and drugs prescribed more frequently than daily (but not more often than every 4 hours) within 1 hour of the scheduled time. For now, hospitals will still be held accountable to CMS for the “30minute rule,” although we anticipate that changes will be forthcoming. No. (9) FDA continues to receive reports of methemoglobinemia (www.fda.gov/Safety/MedWatch/Saf ety Information/SafetyAlertsforHumanM edicalProducts/ucm250264.htm), a serious and potentially fatal adverse effect associated with topical benzocaine products, including sprays used to numb mucous membranes before procedures and over-the-counter gels and liquids used to relieve pain from teething, canker sores, and gum irritation. (13) Regardless of whether a correct or incorrect product or patient has been scanned, audible barcode scanners produce the same beeping sound. The nurse must confirm whether he/she scanned the correct patient/medication by reading the actions on the July 28, 2011 Organization Assessment Action Required/ Assignment Date Completed Benzocaine risk of methemoglobinemia Screen patients who may receive topical benzocaine for risk factors (e.g., G6PD deficiency). Avoid sprays of longer duration than recommended on the label. When possible, use metered-dose sprays. Monitor patients who receive benzocaine sprays for signs of methemoglobinemia during the procedure and for 2 hours postapplication. Additional recommendations can be found at the FDA link to the left. Overreliance on a barcode scanner beep can lead to errors Identify and remedy conditions that may result in absent or poor visibility of the full eMAR during the entire medication administration process, including the scanning process. Scanners that incorporate their own self-contained internal logic may be employed so nurses can view alerts ISMP MedicationSafetyAlert! QAA 3 April – June 2011 ISMP Problem No. electronic medication administration record (eMAR) or hand-held scanner screen. Some nurses have mistakenly relied on the sound of the beep alone to signal verification of the patient and medication. (13) The purpose of barcode scanning is defeated when it occurs after drug administration—a practice called back scanning, which is one of the observed workarounds used to reduce workload during the drug administration process. Employing this workaround increases the risk of wrong drug, wrong dose, wrong time, wrong route, and wrong patient errors. (8) An infant died after receiving a PN solution that contained 60 times more sodium than prescribed. A pharmacy technician entered the dose of calcium (“982” mg) into the mEq field for sodium instead of the correct dose of 14.7 mEq. A sodium dose warning did not appear while entering the order because it had either been entered into a non-PN template without dose limits or entered using an adult template. A free-text label that listed the sodium content as 14.7 mEq was placed over the compounder label, QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed associated with scanning, although the entire eMAR may not be viewable. Educate users not to rely on the audible beep to verify the patient/medication. Barcode scanning after drug administration has little value Hospitals should monitor for back scanning practices, identify the causes if it occurs, and make the necessary system changes to avoid this practice, including but not limited to educating nurses about the risks associated with back scanning. If a drug must be given under urgent conditions, the safest method is to scan the patient and medication barcodes, and create a new task on the electronic medication administration record (eMAR) to document the drug administration, which must be later verified. Parenteral nutrition (PN) calcium dose entered as sodium dose, leading to infant’s death July 28, 2011 Synchronize the order and format of ingredients listed in PN order sets, the pharmacy computer system, the compounder software, and the PN label to help prevent errors. If your PN software supports dose warning limits, fully implement them but do not rely on them only. Define and install more restrictive weight-based dosing limits applicable to specific patient populations. Use product labels that include the actual dose/ strength of the base solution and each additive. Conduct verification processes in the pharmacy to ensure ISMP MedicationSafetyAlert! QAA 4 April – June 2011 ISMP Problem Recommendation contributing to a failure to detect the error during product verification. appropriateness and accuracy of the PN order, additives, and the final PN product, including the expected versus actual weight. No. (10) (9) (9) QuarterlyActionAgenda Organization Assessment Action Required/ Assignment Date Completed PENTACEL (Diphtheria and Tetanus Toxoids, Acellular Pertussis, Poliovirus, Haemophilus b conjugate vaccine [DTaP-IPV and ActHIB]) Numerous infants did not receive the Pharmacies should dispense the two Haemophilus influenzae type b vials together using a rubber band or component of PENTACEL, a twoby placing the two vials in a ziplock part vaccine packaged in cartons bag. Affix an auxiliary label to the containing vials of liquid DTaP-IPV carton to remind staff to use both and vials of lyophilized Haemophilus vials. To confirm administration of influenzae. Nurses administering the both components, staff should two-part vaccine failed to use the document the NDC number for each DTaP-IPV component to dilute and vial in the vaccine log before mix with the lyophilized ActHIB administration. Documenting the powder component of the vaccine. actual administration of the vaccine should always occur after it is given. Inconsistent use of smart pump libraries may lead to legal concerns Clinicians sometimes view the dose Available smart pump technology checking feature of smart pumps as should be fully maximized and an option that can be turned off, or employed consistently, and alerts they may bypass alerts without issued by the technology should be consideration. Serious errors may addressed before administering result. From a legal perspective, parenteral therapy. For assistance when this technology is available but with these formidable tasks, see not used, litigation could be ISMP guidelines for safe successful in finding fault with implementation and use of smart nurses (Harding AD, et al. Nurses’ pumps at: risk without using smart pumps. www.ismp.org/Tools/guidelines/smart JONAS Healthc Law Ethics Regul. pumps/default.asp. 2011;13(1):17-20). Serious interaction between simvastatin and ketoconazole demonstrates a series of latent failures A serious interaction between Ensure that pharmacy computer simvastatin and ketoconazole systems warn about this serious harmed a patient. Concomitant use interaction and require action on the of these drugs increases the risk of part of the pharmacist if both drugs rhabdomyo-lysis. The interaction remain on the patient’s profile. was not detected due to a series of Encourage practitioners who July 28, 2011 ISMP MedicationSafetyAlert! QAA 5 April – June 2011 ISMP Problem Recommendation latent failures including inactive prescriptions that were refilled and a temporary suspension of the pharmacy computer alert system during transition to an electronic record system. investigate events to always look for multiple latent system failures and multiple human errors (active failures) that might have occurred. No. (13) QuarterlyActionAgenda FDA recently alerted the public about mix-ups between risperiDONE and rOPINIRole, some involving patients who required hospitalization. The causes of confusion include: name similarity; illegible written prescriptions; similar product strengths, dosage forms, and dosing intervals; storage next to each other; and appearance together in computer listings. July 28, 2011 Organization Assessment Action Required/ Assignment Date Completed Mix-ups between risperiDONE (RISPERDAL) and rOPINIRole (REQUIP) When prescribing either drug, the drug name should be printed, and the purpose of the drug should be listed. In pharmacies, the products should not be stored near each other, and tall man letters should be used for storage labeling and computer listings. ISMP MedicationSafetyAlert! QAA 6