Use of bovine antibodies-based oral immunotherapy for
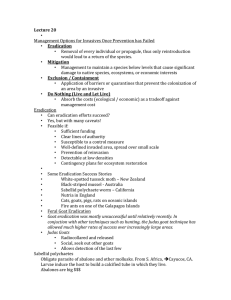
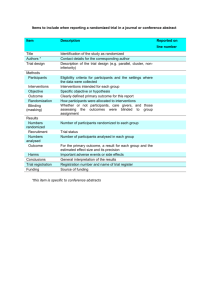
advertisement

Bovine antibody-based oral immunotherapy for reduction of intragastric Helicobacter pylori colonization: A randomized placebo-controlled clinical trial C.M. den Hoed1, A.C. de Vries1, P.B.F. Mensink1, C.M. Dierikx1, N. de Groot2, L. Capelle1, H. van Dekken3, E.J. Kuipers1, 4 C.M. den Hoed1, A.C. de Vries1, P.B.F. Mensink1, C.M. Dierikx1, N. de Groot2, L. Capelle1, H. van Dekken3, E.J. Kuipers1, 4 For treatment of H. pylori (Hp) infections antibiotic-based regimens are mostly used. However, antibioticbased eradication fails in 15-40% of patients, due to antimicrobial resistance and poor patient compliance. Effective prevention and eradication of Hp by passive immunisation with orally administered bovine antibodies has been demonstrated in animal studies and may serve as an alternative therapy in humans. The aim of this study was to study efficacy and safety of orally administered antibodies for reduction of intragastric bacterial load and eradication of Hp in humans. Polyclonal antibodies (sIgA) were raised in milk of dairy cows by nasal and supra-mammary lymph node immunisations with a mix of clinical Hp isolates during lactation. The milk was processed into a whey protein concentrate (WPC). A prospective, double-blind, placebo-controlled randomized clinical trial was designed. Hp-infected subjects were randomized into a WPC-treated or placebo-treated group. Study medication was continued for 28 days; subjects were followed up for 56 days. Efficacy of treatment was evaluated as reduction in intragastric Hp colonization density, determined by urea breath test (UBT) and histology. A blinded pathologist assessed biopsies according to the updated Sydney classification system. Safety was evaluated with blood tests and quality of life questionnaires. All outcome measures were evaluated on day 0 and day 29; on day 56 UBT, blood tests and quality of life questionnaires were repeated. In total, 30 subjects were included; 27 completed the protocol, and the remainder either discontinued study medication within 2 weeks or was lost to follow-up. Within 27 evaluable subjects, there was no significant difference in UBT decrease between the WPC- and the placebo-group (mean decrease ± SEM 0.9 ± 4.3 vs. 3.0 ± 5.0, p=0.75). Hp density and polymorphonuclear neutrophil activity in antrum and corpus were not significantly reduced after treatment in both groups (all p>0.05). In one subject, Hp eradication was achieved after concomitant use of the WPC-product and a 1 day metronidazole course. No serious adverse effects occurred after treatment with the WPC-product. Bovine antibody-based oral immunotherapy appears safe, but does not significantly reduce intragastric Hp density in humans. However, further studies are needed to determine whether WPC treatment has additional value to conventional antibiotic treatment for Hp.