Can oral fluconazole be used during pregnancy?
advertisement

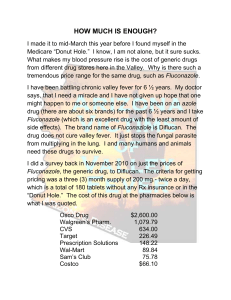
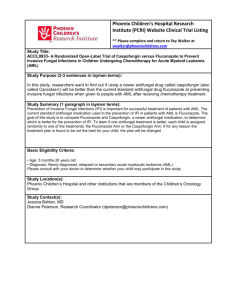
Medicines Q&As UKMi Q&A 147.4 Can oral fluconazole be used during pregnancy? Prepared by UK Medicines Information (UKMi) pharmacists for NHS healthcare professionals Before using this Q&A, read the disclaimer at www.ukmi.nhs.uk/activities/medicinesQAs/default.asp Date prepared: May 2012 Summary Fluconazole is used orally to treat a variety of superficial fungal infections including vulvovaginal candidiasis, and invasive systemic infections including candidiasis, coccidioidomycosis and cryptococcosis. Dosages used in these conditions vary widely. Reported outcomes for over 1,500 pregnancies involving low dose (≤150mg daily) fluconazole provide no evidence of an increased risk of malformations or miscarriage. There are a small number of case reports describing an unusual pattern of congenital malformations similar to the Antley-Bixler syndrome in infants born to mothers who received high dose fluconazole (≥400mg daily) for prolonged periods during the first trimester of pregnancy. Not all of the children presented with the same signs and symptoms. A causal relationship has not been established. Guidance for the use of fluconazole in pregnancy Vulvovaginal candidiasis is common in pregnancy.Topical imidazoles e.g.clotrimazole should be used first-line for the treatment of this condition and used for at least 7 days. These preparations must be prescribed by an appropriate healthcare professional. If topical treatment is ineffective low dose oral fluconazole (150mg single dose) may be considered as second-line treatment. However, prescribers should be aware that some manufacturer’s prescribing information states that use of fluconazole is contraindicated in pregnancy. Inadvertent exposure to low dose fluconazole in pregnancy does not constitute a need to seek termination of the pregnancy. The mother should be reassured that the risk to the fetus is minimal. If high dose fluconazole treatment is given to a woman of childbearing age then she should be counselled on the use of adequate contraception because of the potential for birth defects. Background Fluconazole is a triazole antifungal used orally for treating a variety of superficial fungal infections and either orally or parenterally for systemic infections including candidiasis, coccidioidomycosis and cryptococcosis (1). Dosages used in these conditions vary widely. In the UK, fluconazole is available over-the-counter as a single oral 150mg dose for the treatment of vulvovaginal candidiasis (thrush). This condition is common in women with a higher prevalence of both asymptomatic colonisation with Candida albicans and symptomatic candidiasis in pregnancy. There is, therefore, the potential for inadvertent exposure to low dose fluconazole in the early stages of pregnancy. In pregnant women with severe systemic fungal disease, treatment with high dose fluconazole may be necessary. This Q&A examines data on the potential risks to the fetus when fluconazole is taken by the mother during pregnancy. General information about prescribing in pregnancy can be found here. If you are not familiar with this information, you are advised to review it before reading further. Answer Low dose fluconazole for the treatment of vulvovaginal candidiasis Most data relating to the use of low dose oral fluconazole (≤150mg daily) during pregnancy come from cohort studies. From the NHS Evidence website www.evidence.nhs.uk The largest study to date, identified 171, 532 women from the Danish Medical Birth Registry who had a live birth or stillbirth, between 1991 and 2005 (2). Of these, 1,079 women redeemed a prescription for fluconazole during the first trimester at a total dosage of 150mg (74%), 300mg (22%), 350mg (2%) and 600mg (2%). The prevalence rate of malformations was 4.1% in babies born to these women compared to 3.6% in controls. After adjustment for confounders (maternal smoking status, parity, maternal age, prescriptions for antiepileptics or antidiabetes drugs, and maternal diabetes) there was no overall increased risk of congenital malformations with fluconazole. The adjusted prevalence odds ratio associated with first-trimester fluconazole use was 1.0 [95% CI 0.8 to 1.4]. The findings of this study are supported by those of the following studies. A UK prescription event monitoring (PEM) study reviewed 26,000 prescriptions for fluconazole written between September 1988 and January 1989. In 60 cases of pregnant women receiving a single dose of fluconazole 150mg there were no cases of fetal abnormalities in their children (3,4). Another PEM study identified 48 pregnancies in which fluconazole was taken in the first trimester although the dose and duration of treatment was not specified (5). Pregnancy outcomes for these included 30 single full-term births, 3 single premature births, 2 multiple births of 2 sets of twins full-term, 4 spontaneous abortions, 5 elective abortions and 4 with unknown outcomes. No congenital anomalies were observed. A review of prescriptions from the UK General Practice Research Database, identified 234 women who received a prescription for fluconazole in the first trimester of pregnancy, 92% of whom received a single 150mg dose (6). Matched controls included 492 women who received topical imidazole preparations and 1,629 women who were not exposed to fluconazole or imidazoles. The relative risk of congenital malformations for oral fluconazole users compared with non-users was 1.1 [95% CI 0.4 to 3.3]. Congenital anomalies reported included polydactyly-syndactyly (fluconazole n=1, topical imidazole n=1, non-exposed n=5) and limb abnormalities (fluconazole n=0, topical imidazoles n=1, non-exposed n=3). A prospective cohort study of women who contacted one of three Italian Teratology Information centres between January 1992 and June 1994 compared the outcomes of 226 pregnant women treated with fluconazole during the first trimester of pregnancy with a control group of 452 pregnant women exposed to non-teratogenic agents (7). The primary indication for fluconazole treatment was vaginal candidiasis (90.7%). Doses of fluconazole ranged from single to multiple doses of 50mg, 100mg or 150mg. None of the women in the study group were exposed to other known teratogens. There was a miscarriage rate of 9.7% in the study group compared to 7.5% in the control group, and an elective abortion rate of 12.8% vs. 2.0%. 175 completed pregnancies, resulted in the birth of 177 infants; one was stillborn due to abruptio placentae at 37 weeks and seven had a congenital anomaly (prevalence rate 4.0% compared to 4.2% in the control group). There was no significant association between exposure to fluconazole and any of the primary outcomes including risk of birth defects, late fetal deaths or miscarriages. The only significant pregnancy outcome associated with exposure to fluconazole was induced abortion (odds ratio 5.06 [95% CI 2.28 to 11.21]). An Italian drug information centre received 16 calls from pregnant women who had taken fluconazole in pregnancy. Follow-up of these identified 11 normal births, four by caesarean section and one set of twins were stillborn (no malformations). The average fluconazole dose was 291mg (median 300mg; range 150 to 1,000mg) starting in the first trimester (range 1 to 26 weeks) (8). Nine reports to the FDA involving fluconazole exposure in pregnancy described various malformations including one case each of miscarriage with severe shortening of all limbs and of syndactyly both after a single 150mg dose of fluconazole in the first trimester (9). The UK Teratology Information Service has data on 65 cases of fluconazole exposure in pregnancy There was no increased frequency of congenital malformations above the background rate 3.7% [95% CI 0.64 to 13.83] (10). In summary there are over 1,500 pregnancy outcomes recorded involving low dose oral fluconazole ( ≤150mg daily) with no evidence of an increased risk of malformations or miscarriages suggesting that there is minimal risk of fetal toxicity. High dose fluconazole for the treatment of systemic fungal infections High dose fluconazole (≥400mg daily) is used in the treatment of invasive candidal infections (including candidaemia and disseminated candidiasis) and cryptococcal infections (including meningitis) (11). There are a small number of case reports in which mothers were treated with high dose (≥400mg/daily) fluconazole over a period of months including use in the first trimester of pregnancy. From the NHS Evidence website www.evidence.nhs.uk A 22-year-old woman had disseminated coccidioidomycosis during her first pregnancy and was treated with amphotericin B. She delivered a healthy baby. Subsequently she was treated with oral fluconazole 400mg daily and a second pregnancy was diagnosed at 23 weeks of gestation. Fluconazole was discontinued. Premature rupture of the membranes occurred at 27 weeks and one week later a baby girl was delivered by caesarean section. The baby had grossly dysmorphic features and died shortly after birth. Anatomic abnormalities included cranioschisis of the frontal bones, craniostenosis of the sagittal suture, hypoplasia of the nasal bones, cleft palate, humeral-radial fusion, bowed tibia and femur, bilateral femoral fractures, contractures of both upper and lower extremities, an incompletely formed right thumb and medial deviation of both feet with short toes (12,13). This mother went on to have a third pregnancy but serum levels of fluconazole indicated non-compliance with treatment. She delivered a normal male infant. After this pregnancy she restarted taking fluconazole 400mg daily. A fourth pregnancy was diagnosed in the fourth month of gestation and fluconazole was discontinued. A female infant was born at full term but died later secondary to pneumonia complications. The infant had multiple abnormalities of the head and face, skeleton and the heart (13). A 25-year-old woman diagnosed with Coccidioides immitus meningitis was prescribed fluconazole 800mg daily. She became pregnant and at seven weeks gestation was advised to discontinue taking fluconazole. However, it became necessary to restart fluconazole treatment during the ninth week of gestation. At 38 weeks a male infant was delivered by caesarean section. The infant was small for gestational age and cyanotic with poor tone. Multiple malformations were observed involving the head and face, skeleton and the heart (14). A 27-year-old woman treated with oral fluconazole (400mg daily initially increased to 800mg daily) for Coccidioides immitis had a pregnancy diagnosed at nine weeks gestation. Fluconazole was discontinued and amphotericin started. At 22 weeks amphotericin was discontinued and fluconazole restarted at a dose of 1,200mg daily along with other medicines. Spontaneous rupture of membranes occurred at 31 weeks and a baby boy was delivered by caesarean section with multiple malformations (14). These cases had striking similarities and the features overlap with that of an autosomal recessive genetic disorder known as Antley-Bixler syndrome (ABS). As several features of ABS were lacking in these infants the authors concluded that the abnormalities exhibited were due to the teratogenic effects of fluconazole. Several of the defects observed were similar to those described in fetal rats exposed to fluconazole (13). Although it has been implied that the pattern of these anomalies resembled ABS, the descriptions of some of the cases are incomplete and the rationale for treatment is not always fully explained. Also the effect of the severe systemic maternal illness on the fetus is not known with certainty. No firm causal relationship has been established. In August 2011 the U.S. Food and Drug Administration (FDA) issued a safety announcement stating that chronic, high doses (400-800 mg/day) of fluconazole may be associated with a rare and distinct set of birth defects in infants whose mothers were treated with the drug during the first trimester of pregnancy. This risk does not appear to be associated with a single, low dose of fluconazole 150 mg to treat vaginal candidiasis (15). In contrast to the above there are a few reports of healthy outcomes after exposure of the fetus to highdose fluconazole. One brief case report described a 24-year-old woman with shock, brain haemorrhage and Torulopsis glabrata fungemia treated with intravenous (IV) fluconazole 600mg daily for 21 days starting in the 14th week of pregnancy (16). A healthy baby was delivered in the 41st week and no abnormalities or malformations were noted in a follow-up period of 18 months. In another report a 24year-old woman was diagnosed with Candida albicans sepsis at 16 weeks gestation. A test dose of amphotericin B led to severe nausea and vomiting and so she was treated with IV fluconazole 400mg daily (10mg/kg/day) for 16 days followed by 34 days of oral therapy at the same dose. At 39 weeks a healthy female infant was born who continued to have normal growth and mental development at two years of age (17). A 42–year-old woman with severe nausea and vomiting since the eighth week of pregnancy was admitted to hospital at 31 weeks gestation and diagnosed with Candida oesophagitis. IV fluconazole 150mg daily was started and continued for 14 days. Vomiting ceased and nausea improved slightly. She was discharged at 36 weeks with parenteral nutrition. At 38 weeks she delivered a healthy female infant (18). From the NHS Evidence website www.evidence.nhs.uk Guidance for the use of fluconazole in pregnancy Vulvovaginal candidiasis is common in pregnancy.Topical imidazoles e.g. clotrimazole should be used first-line for the treatment of this condition and used for at least 7 days. These preparations must be prescribed by an appropriate healthcare professional (19,20) If topical treatment is ineffective low dose oral fluconazole (150mg single dose) may be considered as second-line treatment (11). However, prescribers should be aware that some manufacturer’s prescribing information states that use of fluconazole is contraindicated in pregnancy. Inadvertent exposure to low dose fluconazole in pregnancy does not constitute a need to seek termination of the pregnancy. The mother should be reassured that the risk to the fetus is minimal. If high dose fluconazole treatment is given to a woman of childbearing age then she should be counselled on the use of adequate contraception because of the potential for birth defects. Limitations Published case reports lack details of maternal concomitant medication, medical and obstetric history, rationale for treatment and full descriptions of the malformations. Direct causality cannot be proven. Randomised controlled studies have not been conducted and are unlikely to be carried out. Studies available have limitations: pregnancies may have been exposed to polytherapy, data may be duplicated, details of dosage, duration of therapy and gestation of exposure are often lacking. References 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) Sweetman SC, editor. Martindale. The Complete Drug Reference. Accessed via www.medicinescomplete.com on 29/05/2012. Nrgaard M, Pedersen L, Gislum M et al. Maternal use of fluconazole and risk of congenital malformations: a Danish population-based cohort study. J Ant Chemo 2008; 62: 172-176. Inman WHW, Pearce G, Wilton L. Safety of fluconazole in the treatment of vaginal candidiasis. A prescription-event monitoring study, with special reference to the outcome of pregnancy. Eur J Clin Pharmacol 1994; 46: 115-8. Rubin PC, Wilton LV, Inman W.. Fluconazole and pregnancy: results of a prescription eventmonitoring study. Int J Gynecol Obstet 1992; 37(Suppl): 25-7. Wilton LV, Pearce GL, Martin RM et al. The outcomes of pregnancy in women exposed to newly marketed drugs in general practice in England. Br J Obstet Gynaecol 1998; 105: 8829. Jick SS. Pregnancy outcomes after maternal exposure to fluconazole. Pharmacotherapy 1999; 19: 221-2. Mastroiacovo P, Mazzone T, Botto LD et al. Prospective assessment of pregnancy outcomes after first-trimester exposure to fluconazole. Am J Obstet Gynecol 1996; 175: 1645-50. Campomori A and Bonati M. Fluconazole treatment for vulvovaginal candidiasis during pregnancy. Annals of Pharmacother 1997; 31: 118. Letter. Briggs G et al. Drugs in Pregnancy and Lactation. Ninth edition 2011. Philadelphia. Lippincott, Williams and Wilkins 2005. Page 573. United Kingdom Teratology Information Service. Use of fluconazole in pregnancy. Updated November 2008. Accessed 29/05/2012 at www.toxbase.org (subscription required). Mehta DK, editor. British National Formulary No 59. London. BMJ Publishing Group Ltd and RPS Publishing March 2010. Accessed via www.bnf.org.uk on 29/05/2012. Lee BE, Feinberg M, Abraham JJ et al. Congenital malformations in an infant born to a woman treated with fluconazole. Ped Infect Dis J 1992; 11: 1062-4. Pursley TJ, Blomquist IK, Abraham J et al. Fluconazole-induced congenital anomalies in three infants. Clin Infect Dis 1996; 22: 336-40. Aleck KA and Bartley DL. Multiple malformation syndrome following fluconazole use in pregnancy: report of an additional patient. Am J Med Genet 1997; 72: 253-6. From the NHS Evidence website www.evidence.nhs.uk 15) 16) 17) 18) 19) 20) US Food and Drug Administration Drug Safety Communication. Use of long-term, high-dose Diflucan (fluconazole) during pregnancy may be associated with birth defects in infants. August 2011. Accessed at www.fda.gov/Drugs/DrugSafety/ucm266030.htm on 29/05/2012. Krcmery V Jr, Huttova M, Oto M. Teratogenicity of fluconazole. Pediatr Infect Dis J 1996; 15: 841. Wiesinger EC, Mayerhofer S, Wenisch C et al. Fluconazole in Candida albicans sepsis during pregnancy: case report and review of the literature. Infection 1996; 24: 263-6. Kalish RB, Garry D, Figueroa R. Achalasia with Candida esophagitis during pregnancy. Obstet Gynecol 1999; 94: 850. Young G and Jewell D. Topical treatment for vaginal candidiasis (thrush) in pregnancy (review). Cochrane Database of Systematic Reviews 2010, Issue 2. Art No:CD000225. Prodigy. Candida, female genital - management. Accessed at www.prodigy.clarity.co.uk/candida_female_genital/management/scenario_during_pregnanc y#283995006 Quality Assurance Prepared by Lindsay Banks, North West Medicines Information Centre, Liverpool Contact nwmedinfo@nhs.net Date Prepared/ updated March 2006 / March 2008/ March 2010/May 2012 Checked by Christine Proudlove June 2012 Date of check August 2006 / March 2008 / April 2010/June 2012 Search strategy Briggs G et al. Drugs in Pregnancy and Lactation. Ninth edition. Philadelphia. Lippincott, Williams and Wilkins. 2011. Lee A et al. Therapeutics in Pregnancy and Lactation. Oxon. Radcliffe Medical Press Ltd. 2000. Schaefer C et al. Drugs During Pregnancy and Lactation. Treatment options and risk assessment. Second Edition. London. Academic Press. 2007 Rubin P. Prescribing in Pregnancy. Fourth Edition. BMJ Books. 2008. Prodigy searched 29/05/2012 via www.prodigy.clarity.co.uk/home. Search term: candida-female genital. Toxbase searched 29/05/2012 via www.toxbase.org Search term: fluconazole Cochrane Library searched 29/05/2012. Search terms: fluconazole + pregnancy, triazole + pregnancy, antifungals + pregnancy, candida + pregnancy. Medline and Embase searched 29/05/2012: Search History: 1. MEDLINE; exp FLUCONAZOLE/; 2. MEDLINE; exp PREGNANCY/; 3. MEDLINE; 1 AND 2; 4. MEDLINE; 3 [Limit to: Humans and English Language]; 5. MEDLINE; 4 [Limit to: Publication Year 2008-Current and Humans and English Language]; 6. EMBASE; exp FLUCONAZOLE/;. 7. EMBASE; exp PREGNANCY/;. 8. EMBASE; 6 AND 7; 9. EMBASE; 8 [Limit to: Human and English Language]; 10. EMBASE; 9 [Limit to: Publication Year 2008-Current and Human and English Language]; Clinical expert: Dr PR McElhatton, Director of the National Teratology Information Service (NTIS), Newcastle upon Tyne, UK. From the NHS Evidence website www.evidence.nhs.uk