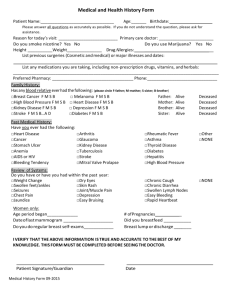
Patient Health History Form
advertisement

Patient Health History Form Franklin County Cardiovascular Associates Department of Cardiology Name: ________________________________________ Date of Birth: ___________ Date _____________ Referring Physician: Reason for your visit: Date of visit: Please indicate if you are having or have had any of these problems in the past Circle= YES Cross out =No cont. Catheterization PTCA/Stent CABG Pacemaker Other Heart Procedure: Constitutional: HEENT: Fatigue Fever Night Sweats Weakness Recent Weight Loss/Gain Nose Bleeds Blurred Vision Ringing in Ears Difficulty eating or swallowing Endocrine: Gastrointestinal: Hematological/Lymphatic: Musculoskeletal: Thyroid Disease Diabetes Heat/Cold Intolerance Hormone Therapy Nausea/Vomiting Reflux/Heartburn Diarrhea/Constipation Anemia Easy Bruising Muscle Cramps Joint Swelling Extremity Swelling Pain to legs with walking Neurological: Psychiatric: Respiratory: Skin: Fainting Seizures Visual Changes Extremity weakness Numbness or tingling Stroke Anxiety Depression Memory Loss/Confusion Asthma COPD Cough History of Pneumonia Emphysema Other: ___________ Sores/Lesions Itching Rashes Bruising Genitourinary: Sleep Habits: Snoring Sleep Apnea Cardiovascular: Chest Pain Palpitations Heart Murmur Hypertension Shortness of Breath Heart attack (MI) Frequent Urination Painful Urination Difficulty/No erection (men) Do you have any allergies or sensitivities to medication or food? Please tell us what and the symptoms. Any allergic reactions to Latex, Tap, IV dye? Current Medications: Name: Dose: # times/day: Name: Dose: # times/day: Hospitalizations (including operations): Year: Reason: Have you ever been told you had (please circle) •Hypertension (yes/no) •Diabetes (yes/no) Hospital: •High Cholesterol (yes/no) Physician: •Stroke (yes/no) Are your parents alive (yes/no) If alive, how old are they? ________________________ If not alive, how old were they when they passed away and what was the cause of death? Mother: Father: How many siblings do you have: ________ Are they all alive: (yes/no) If no, what were the ages and cause of death: _______________________ Family History - Has any of your immediate family members had: (mother, father, sister, brother) Heart Attack: Yes _____ No _____ Who and at what age? ___________________________ Stroke: Yes _____ No _____ Who and at what age? ___________________________ Heart Rhythm Problems: Yes ____ No ____ Who and at what age? ___________________________ Sudden Death: Yes ____No ____ Who and at what age? ___________________________ Social History: Material status: Single Married Divorced Widowed Significant Other Live with: __________________ How many children do you have? _____ What are their ages? If not alive, what was the cause of death? ________________________________________________ Do any of your children have illness (yes/no) If yes, what illness? ____________________________ Do you smoke? How many packs per day? How long? Were you ever a smoker? If yes, for low long? Years as a Nonsmoker: When did you quit? Do you drink alcohol? How many? Per day Per week Do you use recreational Drugs? If yes, what kind? Occupation: Do you do any regular exercise? 2