Morbi-mortality One Year After Surgery
advertisement
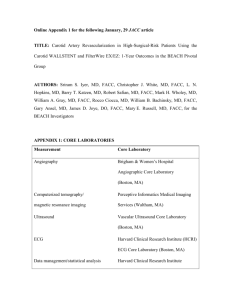
EVERSION VERSUS PATCH CLOSED CAROTID ENDARTERECTOMY: MORBI-MORTALITY ONE YEAR AFTER SURGERY AUTHORS: Bárbara Silva Soeiro (mimed08035@med.up.pt), Joana Brandão Silva (mimed08101@med.up.pt), Jorge Araújo Monteiro (mimed08131@med.up.pt), Mafalda Martins Barbosa (mimed08153@med.up.pt), Marco Batista Assunção (marco_ma@med.up.pt), Pedro Ribeiro Tavares (mimed08196@med.up.pt), Rodrigo Ferreira Monteiro (mimed08228@med.up.pt), Rosário Barbosa Monteiro (rosariom@med.up.pt), Tiago Melo Alves (mimed08234@med.up.pt) ADVISER: Professor Sérgio Sampaio, CLASS N. 20 ABSTRACT BACKGROUND: Carotid endarterectomy (CEA) with patch closure and eversion CEA are currently considered the best surgical procedures to correct carotid stenosis. However, doubt remains on whether one of the procedures is superior over the other and well designed studies that analyse this question are lacking. AIM: This study aimed to compare reports on mortality, neurological morbidity and risk of restenosis for both procedures one year after surgery and determine if one surgical procedure may have advantages over the other. METHODS: We performed a meta-analysis starting with a literature review of articles published regarding one or the other surgical procedures in PubMed, Scopus and ISI Web of Knowledge using appropriate search terms. Studies reporting the proposed outcomes for at least one year after surgery were reviewed and data concerning the outcomes was collected and analysed. Articles that reported both techniques simultaneously (n = 8) were analysed for heterogeneity and overall effect using RevMan. Studies reporting only one of the techniques (n = 46), after pooling data from all studies and including results from studies reporting both procedures into groups of eversion or patch CEA, were analysed by calculating the prevalence of each outcome, relative risk and comparing with chi-square tests. Combined outcomes for neurological morbidity (transient ischemic attack (TIA) + stroke) and morbimortality (neurological morbidity + death) were also calculated and analysed. RESULTS: Pooled data analysis revealed that, for all outcomes analysed, eversion CEA seems to be associated with fewer risks (restenosis RR = 0.332, P < 0.01; TIA RR = 0.551, P < 0.01; stroke RR = 0.504, P < 0.01; neurological morbidity RR = 0.605, P < 0.01; death RR = 0.337, P < 0.01; morbimortality RR = 0.472; P < 0.01). When studies reporting both procedures were analysed, the same was observed for neurological morbidity and death (RR = 0.30, 95% CI [0.11, 0.81], P = 0.02 and RR = 0.41, 95% CI [0.22, 0.77], P < 0.01, respectively) and there was an equal trend for data on stroke (RR = 0.34, 95% CI [0.11, 1.05], P = 0.06). However, this analysis seemed to attribute fewer cases of restenosis to patch closure CEA (RR = 1.31, 95% CI [0.96, 1.78], P = 0.09). CONCLUSION: Eversion CEA is associated with fewer cases of neurological morbidity and death and may result in less cases of stroke one year after surgery. However, CEA with Dacron patch closure may be more effective in preventing restenosis. KEYWORDS: Carotid endarterectomy, mortality, stroke, transient ischemic attack, restenosis, eversion, patch closure INTRODUCTION Carotid artery stenosis occurs as a consequence of hardening and atherosclerotic deposition of oxidized lipoproteins within the inner layers of the carotid artery(1, 2). This substantially reduces lumen size, increasing the occurrence of blood clotting at that point with subsequent higher likelihood of thrombus formation and embolism(2, 3). Since the carotid artery is the main blood supplier to the brain(2-4), the occlusion of brain vessels with ischemic lesion of adjacent brain areas is increased in subjects bearing carotid stenosis. These events are termed strokes also known as cerebrovascular accidents, and result in impairment of the brain area affected and inability to perform its normal functions (usually sight, speech and movement of one side of the body are affected)(4, 5). If the neurological dysfunction is brief and lasts no more than 24 h, then it is termed transient ischemic attack (TIA)(4). There are currently several surgical techniques being used to correct extracranial carotid stenosis (6). Among them, carotid endarterectomy (CEA) has been shown to have excellent results in the reduction of the risk of stroke(7-10). Since it was first established, several advances have been made to the surgical procedure to improve the clinical results and long-term durability of CEA(9). Despite having evolved from a somewhat different procedure described in 1954(11), the standard surgical approach to endarterectomy consisted of performing a longitudinal arteriotomy to gain access to the lumen of the artery followed by resection of the atheromatous plaque and primary closure after surgery(9, 10). Notwithstanding, it has been determined that although very efficient, this technique involved some risk of restenosis of the carotid artery(9, 12), which led to the development of slightly modified procedures for CEA. One of them involves basically the same procedure, but using a fragment of vascular tissue removed from superficial veins, usually from the lower limbs, to close the section, avoiding reduction of vessel lumen after closure(9, 10). This has further evolved to the use of synthetic prosthetic materials, obtaining a similar result but sparing the superficial lower limb vessels(9, 10, 13, 14). In parallel with this patch closure procedure, a new technique was introduced, consisting of the transection of the common carotid artery, eversion of the limits of the vessel, performing the removal of the damaged inner layer of the artery and restoring the vessel with closure of both extremities of the resected vessel(9, 10). This later technique, called eversion CEA, has been considered by some surgeons a simpler, faster procedure and has been suggested to be related with fewer post-surgery complications, lower risk of stroke and death than the remaining(15, 16). However, there is still no exact knowledge on which technique, eversion CEA or CEA with patch closure, is the most effective and is related with lower mortality and fewer complications(8, 17). In this work, we aimed at evaluating both surgical techniques through a meta-analysis comparing main outcomes: mortality, occurrence of neurological morbidity and restenosis one year after surgical treatment. Specific research questions are: is mortality different in patients subjected to eversion CEA in comparison to patients treated with CEA with patch closure? Does one of the procedures represent lower risk of neurologic morbidity? What is the combined risk of mortality and neurological morbidity for each technique? Which technique is associated with lower risk of restenosis? METHODS After indentifying adequate keywords and respective medical subject headings (MeSH) terms a query algorithm was built to perform searches of articles in PubMed, Scopus and Isi Web of Knowledge databases. Main search terms were: CEA, mortality, stroke, TIA, restenosis, eversion, patch closure (or equivalent terms). The query algorithm used for database search was: carotid AND (endarterectomy OR endarterectomies) AND (eversion OR patch) AND (mortality OR death OR "neurologic morbidity" OR stroke OR "vascular accident" OR "brain vascular accident" OR "cerebrovascular accident" OR CVA OR restenosis OR "transient ischemic attack" OR “transient brainstem ischemia" OR "cerebral ischemia" OR TIA). Search was limited to articles published in English from January 1st, 1990 to November 30th, 2008. The upper time limit was chosen to avoid disparities due to independent factors (evolution in pharmacotherapy used in atherosclerotic patients to decrease the risk of complications that may have impact on measured outcomes, and grade of evolution of surgical techniques). Repeated references were eliminated from the retrieved lists of references and remaining abstracts were selected by two investigators according to a predefined list of exclusion criteria. Disagreements were resolved by consensus. Eligibility criteria Articles that fitted one or more exclusion criteria were excluded. Succinctly, an article that: 1) was not a complete or consecutive patient series or clinical trial; 2) did not refer endarterectomy with Dacron patch closure or eversion; 3) did not mention post-operative neurological morbidity or mortality; 4) did not present outcomes for both techniques separately or 5) had a follow-up lower than one year, was excluded. From the 1242 references initially retrieved (346 from PubMed, 506 from Scopus and 390 from ISI Web of Knowledge), 709 remained after elimination of repeated references. From these, 619 were excluded (211 for criterion 1, 280 for 2, 37 for 3, 72 for 4 and 19 for 5), whereas 90 were considered candidate studies. After abstract selection, the complete articles were gathered, either through retrieval online or through contacts of local libraries or article authors. Only 72 full-text articles were retrieved of the 90 references. Articles were read by two researchers and either included or excluded using the same predefined eligibility criteria. A total of 52 articles were included after full text reading as 1 were excluded for criterion 1, 8 for 2, 1 for 3, 8 for 4 and 2 for 5. In studies performed by the same group of researchers the articles was carefully read to determine if the data referred to the same case series and if it was the case, the article presenting the largest, usually most recent, series would be used. Variable description and statistical analysis Data were collected from the studies, namely descriptive data (e.g. number of patients subjected to the procedure of interest), methodological data (e.g. was the intervention randomized) and outcome data (e.g. TIA, stroke, death, restenosis, stenosis criteria). Combined outcomes for neurological morbidity (TIA + stroke) and morbimortality (neurological morbidity + death) were also calculated and analysed. Only 8 articles(16-23) had information about both techniques and these were introduced in RevMan software (version 5.0.18)(24). Test for overall effects was performed through MantelHaenszel fixed effects model and relative risks (RR) are shown with 95% confidence intervals (CI). Heterogeneity of the measures obtained from elected studies was assessed through a Chi2 test, allowing us to determine if there is variation across studies was due to differences in surgical procedure, study subjects or design rather than chance. Studies reporting only one of the techniques (n = 46)(15, 25-62), after pooling data from all studies and including results from studies reporting both procedures into groups of eversion or patch CEA, were analysed by calculating the prevalence of each outcome, RR and comparing with Chi2 tests on SPSS software (version 17.0.0)(63). Differences were considered statistically significant when P < 0.05. RESULTS Data was analysed in two stages, as described previously. Data from studies reporting either Dacron patch OR eversion CEA (n = 46) were pooled into two groups of results regarding each technique. From studies which had information about both techniques, data from Dacron patch or eversion CEA were grouped with data of the corresponding group collected from studies that described either procedure. This is referred to as “pooled data”. Afterwards, the 8 studies that reported simultaneously results from Dacron patch and eversion CEA were analysed separately using more sophisticated and powerful analysis. This later group is referred to as “studies with patch and eversion” Pooled data A total of 25 studies reported outcomes for Dacron patch CEA, involving a total number of operations of 4110, while 32 presented outcomes for eversion CEA representing 20998 operations. In studies reporting Dacron patch CEA, 16 studies defined a carotid artery stenosis criteria as at least 50% occlusion of the lumen of the vessel, 1 study used 60%, 3 studies considered 70% and 3 studies used 80% and the remaining did not define stenosis criteria. Studies reporting eversion CEA, 3 defined restenosis as an occlusion lower than 50%, 12 defined restenosis as 50% occlusion or higher, 2 considered 60, 1 defined 70%, 3 used 80% and the remaining did not define stenosis criteria. Pooled data analysis revealed that, for all outcomes analysed, eversion CEA seems to be associated with fewer risks (Table 1). Restenosis, at least one year after surgery occurred in 8.85% (n = 300) of patients undergoing Dacron Patch CEA (n = 3390) and in 2.94% (n = 574) of patients undergoing eversion CEA (n = 19184). The RR of restenosis associated with eversion CEA in comparison to Dacron Patch CEA was 0.332 (P < 0.01). Eversion CEA was also associated with fewer cases of TIA (2.97 and 1.97%, respectively) as compared to CEA with patch closure (5.93 and 3.91, respectively), the RR of suffering the outcomes being 0.551 (P < 0.01) and 0.504 (P < 0.01). Combining the data from these two outcomes and computing the new variable neurological morbidity we found a RR of 0.605, (P < 0.01) for this outcome when undergoing eversion in comparison to patch CEA. The same protective effect of the surgical procedures through eversion was associated with mortality (RR = 0.337, P < 0.01) and for the outcomes of death and neurological morbidity combined as morbimortality (RR = 0.472; P < 0.01). Studies with patch and eversion CEA When studies reporting both procedures were analysed, we found no significant difference between the two surgical procedures regarding the outcome restenosis (Figure 1). However, this analysis tended to attribute fewer cases of restenosis to patch closure CEA (RR = 1.31, 95% CI [0.96, 1.78], P = 0.09). Furthermore, there was statistically significant heterogeneity among studies (P < 0.01). Regarding the risk of occurrence of TIA one year after surgery, we found no statistical difference between the two procedures (RR = 0.27, 95% CI [0.05, 1.64], P = 0.16) although only two studies were used in this analysis as only these two provided information on both techniques (Figure 2). In respect to stroke (Figure 3), although the difference between studies did not reach statistical significance (P = 0.06) there was trend showing more favorable results with eversion CEA (RR = 0.34, 95% CI [0.11, 1.05]). On the other hand, the test for overall effect using the studies which presented simultaneously data from both techniques showed a lower RR for neurological morbidity (Figure 4) and death (Figure 5) in patients undergoing patch CEA in comparison to those patients undergoing correction of carotid stenosis through the eversion technique (RR = 0.30, 95% CI [0.11, 0.81], P = 0.02 and RR = 0.41, 95% CI [0.22, 0.77], P < 0.01, respectively). Furthermore, no statistical significance (P = 0.12) was found when assessing the heterogeneity of samples strengthening the statistical approach used. When the outcomes neurological morbidity and death were analysed in combination as morbimortality, there was no significant difference between the two surgical procedures (RR = 0.9, 95% CI [0.58, 1.39], P = 0.64) and there was significant heterogeneity among studies (P < 0.01). DISCUSSION Although several surgical procedures to correct stenosis of the carotid artery are currently performed, including CEA with synthetic patch angioplasty and eversion CEA there is still controversy on which technique is related to poorer post-operative or long-term complications and whether or not it applies to all clinical situations(51). Thus, surgeon preference and experience with one of the procedures is the reason that often dictates which technique to choose for operation (51). On the other hand, it is more consensual that primary closure CEA results in higher numbers of peri-operative and postoperative complications, including stroke and death(64). As there are many other surgical techniques to perform stenosis correction(9), we were faced with the fact that most studies selected for the present investigation report only one of the techniques that we have aimed to analyze and a different one (for example CEA with saphenous vein patch closure or using synthetic materials other than Dacron to perform angioplasty). We have found only 8 studies that were designed to compare our target procedures and all 46 remaining studies were designed to compare either Dacron patch or eversion CEA with a different technique. For this reason, we chose to perform our analysis in two steps, first pooling data from each procedure and calculating relative risks manually. Afterwards, as we believe should be more informative and reliable, we have compared in a separate analysis studies reporting both techniques at the same time using appropriate computer software. The reasons supporting the assumption that the results from this analysis may be more reliable are that, although only few studies, and consequently a small number of operations, fitted this category, the fact that they were designed specifically to compare these techniques has prompted that ideally this is the single characteristic varying between case groups. Furthermore, most of them were prospective randomized trials, meaning that the decision to perform Dacron patch closure CEA or eversion had no criterion other than random choice. In the pooled data analysis, we found that in patients undergoing CEA eversion all outcomes were significantly less prevalent than in patients treated with Dracon patch CEA. As mentioned there is controversy in the current literature on which one of these two techniques is related to between outcomes(7, 22). The present results show that eversion is associated with fewer cases of restenosis, TIA, stroke, death and the combined outcomes neurological morbidity and morbimortality. However, it is necessary to bear in mind that data collected from studies reporting Dacron patch CEA totalized 4110, while for eversion CEA 20998 operations contributed to this analysis. This disparity in number of operations may also have played in favour of supporting the eversion procedure. Although we attribute more value to the analysis obtained with studies reporting simultaneously both techniques, for the reasons presented earlier, we should mentioned that we were settled to find that the same evidence or tendency was obtained for most outcomes analysed. The most surprising finding was that concerning restenosis. Even though the result obtained was not significant, we found that restenosis occurrence tended to be less frequent in CEA with patch angioplasty. One of the possible explanations for this discrepancy lies in the fact that criteria for stenosis was strongly uneven among groups of eversion and patch CEA, and usually the criteria for stenosis was more loose in patch CEA. As a consequence, since restenosis was considered only after 50%, 60%, 70% or 80% artery occlusion in patients operated with patch CEA, in the case of eversion CEA, some studies considered a 35% occlusion as restenosis. We believe that this may be one of the strongest reasons to explain this apparent lack of consistency. Concerning the outcomes TIA and morbimortality, no statistically significant difference between the two surgical techniques was found. In the later case, the heterogeneity of the study may have contributed to the lack of a statistically significant association. However, regarding stroke, eversion CEA tended to be related with less cases of this complication. Perhaps the most interesting results obtained are related to neurological morbidity and death that were significantly less in patients operated with eversion CEA. Although those results may seem to be in contrast with those obtained for restenosis, one should remember that for the occurrence of neurological events the diameter of the blood vessel is not the only variable to take into account(40). We propose that, independently of artery lumen diameter, the reactivity of the components of the blood to Dacron could be different, possibly enhanced, compared to when the vessel is restored after eversion, which may be associated with a higher number of thromboembolic events. We should stress that this systematic review and meta-analysis was methodologically challenging because of the variations in definition of stenosis as well as other differences in design among studies. Other factors that may obscure the results obtained in the present analysis is that in studies used in the analysis did not take into account surgeon preferences(64). This would be important as individual surgeons tend to use the technique they are more comfortable with, what makes it difficult and artificial to separate the effects of the technique from those of the surgeon. Notwithstanding, in the present study we found that eversion CEA is associated with fewer cases of neurological morbidity and death and may result in less cases of stroke one year after surgery. However, concerning restenosis there is still doubt on which surgical procedures may offer advantage. Acknowledgments We would like to acknowledge the fundamental scientific advices in every manuscript production phase of Prof. Sérgio Sampaio that were pivotal to the conveyance of the present study. We would also like to thank the helpful criticisms of Prof. Altamiro Pereira. REFERENCES 1. Debakey, S., Medical writing as we would like to make it; for authors, editors and professional writers; introductory remarks. Miss Valley Med J 1959, 81, 49-52. 2. Heberer, G.; Rau, G.; Löhr, H., Enfermedades oclusivas crónicas de las arterias: Arteria carótida interna. In Enfermedades de la aorta y de las grandes arterias, Heberer, G.; Rau, G.; Löhr, H., Eds. Editorial Científico-Médica: Barcelona, 1970; pp 316-324. 3. Sumner, D. S., Essential Hemodynamic Principles. In Vascular Surgery, 5th ed.; Rutherford, R. B., Ed. W.B. Saunders Company: Pennsylvania, 2000; Vol. 1, pp 78-79. 4. Hallett, J. W.; D.C., B.; Rasnussen, T. E., Cerebrovascular Disease. In Handbook of Patient Care in Vascular Diseases, 4th ed.; Hallett, J. W.; D.C., B.; Rasnussen, T. E., Eds. Lippincott Williams & Wilkins: Philadelphia, 2001; pp 131-136. 5. Manuila, L.; Manuila, A.; Lewalle, P.; Nicoulin, M., Dicionário Médico. Climepsi Editores: Lisboa, 1999. 6. Hobson, R. W., 2nd; Mackey, W. C.; Ascher, E.; Murad, M. H.; Calligaro, K. D.; Comerota, A. J.; Montori, V. M.; Eskandari, M. K.; Massop, D. W.; Bush, R. L.; Lal, B. K.; Perler, B. A., Management of atherosclerotic carotid artery disease: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg 2008, 48, 480-6. 7. Byrne, J.; Feustel, P.; Darling, R. C., 3rd, Primary closure, routine patching, and eversion endarterectomy: what is the current state of the literature supporting use of these techniques? Semin Vasc Surg 2007, 20, 226-35. 8. Cao, P.; Giordano, G.; De Rango, P.; Zannetti, S.; Chiesa, R.; Coppi, G.; Palombo, D.; Spartera, C.; Stancanelli, V.; Vecchiati, E., A randomized study on eversion versus standard carotid endarterectomy: study design and preliminary results: the Everest Trial. J Vasc Surg 1998, 27, 595-605. 9. Messina, L. M.; Stoney, R. J., Endarterectomy In Vascular Surgery, 5th ed.; Rutherford, R. B., Ed. W.B. Saunders Company: Pennsylvania, 2000; Vol. 1, pp 488-493. 10. Zarins, C. K.; Gewertz, B. L., Carotid artery surgery. In Atlas of Vascular Surgery, 2nd ed.; Zarins, C. K.; Gewertz, B. L., Eds. Elsevier Philadelphia, 2005; Vol. 1, pp 3-13. 11. Senning, A., Developments in cardiac surgery in Stockholm during the mid and late 1950s. J Thorac Cardiovasc Surg 1989, 98, 825-32. 12. Entz, L.; Jaranyi, Z.; Nemes, A., Comparison of perioperative results obtained with carotid eversion endarterectomy and with conventional patch plasty. Cardiovasc Surg 1997, 5, 16-20. 13. Aburahma, A. F., Patch closure improves results with carotid endarterectomy. Semin Vasc Surg 2004, 17, 243-52. 14. Aburahma, A. F.; Stone, P. A.; Elmore, M.; Flaherty, S. K.; Armistead, L.; AbuRahma, Z., Prospective randomized trial of ACUSEAL (Gore-Tex) vs Finesse (Hemashield) patching during carotid endarterectomy: long-term outcome. J Vasc Surg 2008, 48, 99-103. 15. Ballotta, E.; Da Giau, G.; Saladini, M.; Abbruzzese, E.; Renon, L.; Toniato, A., Carotid endarterectomy with patch closure versus carotid eversion endarterectomy and reimplantation: a prospective randomized study. Surgery 1999, 125, 271-9. 16. Crawford, R. S.; Chung, T. K.; Hodgman, T.; Pedraza, J. D.; Corey, M.; Cambria, R. P., Restenosis after eversion vs patch closure carotid endarterectomy. J Vasc Surg 2007, 46, 41-8. 17. Cao, P.; Giordano, G.; De Rango, P.; Zannetti, S.; Chiesa, R.; Coppi, G.; Palombo, D.; Peinetti, F.; Spartera, C.; Stancanelli, V.; Vecchiati, E., Eversion versus conventional carotid endarterectomy: late results of a prospective multicenter randomized trial. J Vasc Surg 2000, 31, 19-30. 18. Ballotta, E.; Renon, L.; Da Giau, G.; Toniato, A.; Baracchini, C.; Abbruzzese, E.; Saladini, M.; Moscardo, P., A prospective randomized study on bilateral carotid endarterectomy: patching versus eversion. Ann Surg 2000, 232, 119-25. 19. Brothers, T. E., Initial experience with eversion carotid endarterectomy: absence of a learning curve for the first 100 patients. J Vasc Surg 2005, 42, 429-34. 20. Economopoulos, K. J.; Gentile, A. T.; Berman, S. S., Comparison of carotid endarterectomy using primary closure, patch closure, and eversion techniques. American Journal of Surgery 1999, 178, 505-509. 21. Green, R. M.; Greenberg, R.; Illig, K.; Shortell, C.; Ouriel, K., Eversion endarterectomy of the carotid artery: technical considerations and recurrent stenoses. J Vasc Surg 2000, 32, 1052-61. 22. Littooy, F. N.; Gagovic, V.; Sandu, C.; Mansour, A.; Kang, S.; Greisler, H. P., Comparison of standard carotid endarterectomy with Dacron patch angioplasty versus eversion carotid endarterectomy during a 4-year period. Am Surg 2004, 70, 181-5; discussion 185. 23. Winkler, G. A.; Calligaro, K. D.; Kolakowski, S.; Doerr, K. J.; McAffee-Bennett, S.; Muller, K.; Dougherty, M. J., Comparison of intraoperative completion flowmeter versus duplex ultrasonography and contrast arteriography for carotid endarterectomy. Vasc Endovascular Surg 2006, 40, 482-6. 24. Review Manager, version 5.0.18; The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, 2008. 25. AbuRahma, A. F.; Hopkins, E. S.; Robinson, P. A.; Deel, J. T.; Agarwal, S., Prospective randomized trial of carotid endarterectomy with polytetrafluoroethylene versus collagenimpregnated dacron (Hemashield) patching: late follow-up. Ann Surg 2003, 237, 885-92; discussion 892-3. 26. AbuRahma, A. F.; Robinson, P. A.; Hannay, R. S.; Hudson, J.; Cutlip, L., Prospective controlled study of carotid endarterectomy with hemashield patch: is it thrombogenic? Vasc Surg 2001, 35, 167-74. 27. Ali, T.; Sabharwal, T.; Dourado, R. A.; Padayachee, T. S.; Hunt, T.; Burnand, K. G., Sequential cohort study of Dacron patch closure following carotid endarterectomy. Br J Surg 2005, 92, 31621. 28. Archie, J. P., Carotid endarterectomy outcome with vein or Dacron graft patch angioplasty and internal carotid artery shortening. J Vasc Surg 1999, 29, 654-64. 29. Archie, J. P., Jr., Reoperations for carotid artery stenosis: role of primary and secondary reconstructions. J Vasc Surg 2001, 33, 495-503. 30. Asciutto, G.; Geier, B.; Marpe, B.; Hummel, T.; Mumme, A., Dacron patch infection after carotid angioplasty. A report of 6 cases. Eur J Vasc Endovasc Surg 2007, 33, 55-7. 31. Bhattacharya, V.; Ghali, R.; El-Massry, S.; Saad, E.; Zammit, M.; Rodriguez, D.; Spencer, M. P.; Sauvage, L. R., A clinical comparison of Dacron patch closure of small-caliber carotids compared with primary closure of large-caliber carotids after endarterectomy. Am Surg 1999, 65, 378-82. 32. Goldman, K. A.; Su, W. T.; Riles, T. S.; Adelman, M. A.; Landis, R., A comparative study of saphenous vein, internal jugular vein, and knitted Dacron patches for carotid artery endarterectomy. Ann Vasc Surg 1995, 9, 71-9. 33. Golledge, J.; Cuming, R.; Davies, A. H.; Greenhalgh, R. M., Outcome of selective patching following carotid endarterectomy. Eur J Vasc Endovasc Surg 1996, 11, 458-63. 34. Jacobowitz, G. R.; Kalish, J. A.; Lee, A. M.; Adelman, M. A.; Riles, T. S.; Landis, R., Long-term follow-up of saphenous vein, internal jugular vein, and knitted Dacron patches for carotid artery endarterectomy. Ann Vasc Surg 2001, 15, 281-7. 35. Johnson, C. A.; O'Donnell, S.; Gillespie, D.; Goff, J. M., Early recurrent carotid artery stenosis. Current Surgery 1999, 56, 420-422. 36. Johnson, C. A.; Tollefson, D. F.; Olsen, S. B.; Andersen, C. A.; McKee-Johnson, J., The natural history of early recurrent carotid artery stenosis. Am J Surg 1999, 177, 433-6. 37. Katz, S. G.; Kohl, R. D., Does the choice of material influence early morbidity in patients undergoing carotid patch angioplasty? Surgery 1996, 119, 297-301. 38. Naylor, R.; Hayes, P. D.; Payne, D. A.; Allroggen, H.; Steel, S.; Thompson, M. M.; London, N. J.; Bell, P. R., Randomized trial of vein versus dacron patching during carotid endarterectomy: long-term results. J Vasc Surg 2004, 39, 985-93; discussion 993. 39. Perler, B. A.; Ursin, F.; Shanks, U.; Williams, G. M., Carotid Dacron patch angioplasty: immediate and long-term results of a prospective series. Cardiovasc Surg 1995, 3, 631-6. 40. Verhoeven, B. A. N.; Pasterkamp, G.; de Vries, J. P. P. M.; Ackerstaff, R. G. A.; de Kleijn, D.; Eikelboom, B. C.; Moll, F. L., Closure of the arteriotomy after carotid endarterectomy: Patch type is related to intraoperative microemboli and restenosis rate. Journal of Vascular Surgery 2005, 42, 1082-1088. 41. Assadian, A.; Rotter, R.; Assadian, O.; Senekowitsch, C.; Hagmuller, G. W.; Hubl, W., Homocysteine and early re-stenosis after carotid eversion endarterectomy. Eur J Vasc Endovasc Surg 2007, 33, 144-8. 42. Ballotta, E.; Da Giau, G., Selective shunting with eversion carotid endarterectomy. J Vasc Surg 2003, 38, 1045-50. 43. Ballotta, E.; Da Giau, G.; Baracchini, C.; Abbruzzese, E.; Saladini, M.; Meneghetti, G., Early versus delayed carotid endarterectomy after a nondisabling ischemic stroke: a prospective randomized study. Surgery 2002, 131, 287-93. 44. Ballotta, E.; Da Giau, G.; Guerra, M.; Toffano, M., Carotid eversion endarterectomy and reimplantation: a safe and simple technique to prevent acute thrombosis-occlusion and/or early and late restenosis. Cardiovasc Surg 1997, 5, 473-80. 45. Ballotta, E.; Meneghetti, G.; Da Giau, G.; Manara, R.; Saladini, M.; Baracchini, C., Carotid endarterectomy within 2 weeks of minor ischemic stroke: a prospective study. J Vasc Surg 2008, 48, 595-600. 46. Ballotta, E.; Meneghetti, G.; Manara, R.; Baracchini, C., Long-term survival and stroke-free survival after eversion carotid endarterectomy for asymptomatic severe carotid stenosis. J Vasc Surg 2007, 46, 265-70. 47. Darling, R. C.; Mehta, M.; Roddy, S. P.; Paty, P. S. K.; Kreienberg, P. B.; Ozsvath, K. J.; Chang, B. B.; Shah, D. M., Eversion carotid endarterectomy: a technical alternative that may obviate patch closure in women. Cardiovascular Surgery 2003, 11, 347-352. 48. Darling, R. C., 3rd; Paty, P. S.; Shah, D. M.; Chang, B. B.; Leather, R. P., Eversion endarterectomy of the internal carotid artery: technique and results in 449 procedures. Surgery 1996, 120, 635-9; discussion 639-40. 49. Iseli, T. A.; Puttaswamy, V.; Campbell, W. A.; Atkinson, N. R., Eversion carotid endarterectomy. ANZ J Surg 2001, 71, 570-3. 50. Jones, C. E.; Jescovitch, A. J., Jr.; Kahn, A.; Walters, G. K.; Johnson, C. J., Technical results from the eversion technique of carotid endarterectomy. Am Surg 1996, 62, 361-5. 51. Katras, T.; Baltazar, U.; Rush, D. S.; Sutterfield, W. C.; Harvill, L. M.; Stanton, P. E., Jr., Durability of eversion carotid endarterectomy: comparison with primary closure and carotid patch angioplasty. J Vasc Surg 2001, 34, 453-8. 52. Koskas, F.; Kieffer, E.; Bahnini, A.; Ruotolo, C.; Rancurel, G., Carotid eversion endarterectomy: short- and long-term results. Annals of Vascular Surgery 1995, 9, 9-15. 53. Mehta, M.; Rahmani, O.; Dietzek, A. M.; Mecenas, J.; Scher, L. A.; Friedman, S. G.; Safa, T.; Ohki, T.; Veith, F. J., Eversion technique increases the risk for post-carotid endarterectomy hypertension. J Vasc Surg 2001, 34, 839-45. 54. Peiper, C.; Nowack, J.; Ktenidis, K.; Reifenhauser, W.; Keresztury, G.; Horsch, S., Eversion endarterectomy versus open thromboendarterectomy and patch plasty for the treatment of internal carotid artery stenosis. Eur J Vasc Endovasc Surg 1999, 18, 339-43. 55. Radak, D.; Radevic, B.; Sternic, N.; Vucurevic, G.; Petrovic, B.; Ilijevski, N.; Radicevic, S.; Neskovic, A. N.; Bojic, M., Single center experience on eversion versus standard carotid endarterectomy: a prospective non-randomized study. Cardiovasc Surg 2000, 8, 422-8. 56. Radak, D. J.; Ilijevski, N. S.; Nenezic, D.; Popov, P.; Vucurevic, G.; Gajin, P.; Jocic, D.; Kolar, J.; Radak, S.; Sagic, D.; Matic, P.; Milicic, M.; Otasevic, P., Temporal trends in eversion carotid endarterectomy for carotid atherosclerosis: single-center experience with 5,034 patients. Vascular 2007, 15, 205-10. 57. Reigner, B.; Reveilleau, P.; Gayral, M.; Papon, X.; Enon, B.; Chevalier, J. M., Eversion endarterectomy of the internal carotid artery: midterm results of a new technique. Ann Vasc Surg 1995, 9, 241-6. 58. Schneider, J. R.; Droste, J. S.; Golan, J. F., Carotid endarterectomy in women versus men: patient characteristics and outcomes. J Vasc Surg 1997, 25, 890-6; discussion 897-8. 59. Shah, D. M.; Darling, R. C., 3rd; Chang, B. B.; Kreienberg, P. B.; Paty, P. S., Carotid endarterectomy by eversion technique. Adv Surg 1999, 33, 459-76. 60. Shah, D. M.; Darling, R. C.; Chang, B. B.; Paty, P. S. K.; Kreienberg, P. B.; Lloyd, W. E.; Leather, R. P., Carotid endarterectomy by eversion technique - Its safety and durability. Annals of Surgery 1998, 228, 471-476. 61. Szabo, A.; Laki, J.; Madsen, H. O.; Dosa, E.; Prohaszka, Z.; Rugonfalvi-Kiss, S.; Kokai, M.; Acsadi, G.; Karadi, I.; Entz, L.; Selmeci, L.; Romics, L.; Fust, G.; Garred, P.; Cervenak, L., Early rise in serum VEGF and PDGF levels predisposes patients with a normal MBL2 genotype to restenosis after eversion endarterectomy. Stroke 2007, 38, 2247-53. 62. Ziaja, K.; Krupowies, A.; Kuczmik, W.; Ziaja, D.; Kazibudzki, M.; Ludyga, T.; Geborski, J., Treatment of critical stenosis of internal carotid artery in octogenarians. Chirurgia Polska 2006, 8, 27-32. 63. Statistical Package for the Social Sciences, version 17.0.0; SPSS Inc. Headquarters: Chicago, 2008. 64. Rockman, C. B.; Halm, E. A.; Wang, J. J.; Chassin, M. R.; Tuhrim, S.; Formisano, P.; Riles, T. S., Primary closure of the carotid artery is associated with poorer outcomes during carotid endarterectomy. J Vasc Surg 2005, 42, 870-7. TABLES Table 1 – Summary of results from the comparison of studies reporting outcomes related to restenosis, neurological morbidity and mortality associated with Dacron patch CEA or eversion CEA. Pooled data Studies with Patch and Eversion Prevalence Restenosis TIA Stroke Stroke+TIA Death Morbi-mortality number of events/total Relative % risk* Patch Eversion 300 / 3390 574 / 19184 8.85% 2.94% 58 / 1077 383 / 12940 5.39% 2.97% 107 / 2738 360 / 18499 3.91% 1.97% 175 / 2620 745/18602 6.68% 4.02% 98 / 2310 294 / 20512 4.24% 1.43% 275 / 2620 1044 / 20998 10.5% 4.96% Pa Relative risk* [95% CI] Pb 0.332 < 0.01 1.31 [0.96, 1.78] 0.09 0.551 < 0.01 0.27 [0.05, 1.64] 0.16 0.504 < 0.01 0.34 [0.11, 1.05] 0.06 0.605 < 0.01 0.30 [0.11, 0.81] 0.02 0.337 < 0.01 0.41 [0.22, 0.77] < 0.01 0.472 < 0.01 0.90 [0.58, 1.39] 0.64 *Risk involving eversion carotid endarterectomy in comparison to endarterectomy with patch closure. aChi2; bMantelHeanszel fixed effects. TIA - transient ischemic attack, CI – confidence interval. FIGURES Figure 1 – Forest plot showing the relative risk calculated from data collected from the 8 selected studies that presented outcomes for restenosis both after patch and eversion carotid endarterectomy. Data was analysed using Mantel-Haenszel fixed effects model and heterogeneity of the measures obtained from selected studies was assessed through a Chi 2 test. Differences were considered statistically significant when P < 0.05. Figure 2 – Forest plot showing the relative risk calculated from data collected from the 2 selected studies that presented outcomes for transient ischemic attack both after patch and eversion carotid endarterectomy. Data was analysed using Mantel-Haenszel fixed effects model and heterogeneity of the measures obtained from selected studies was assessed through a Chi2 test. Differences were considered statistically significant when P < 0.05. Figure 3 – Forest plot showing the relative risk calculated from data collected from the 7 selected studies that presented outcomes for stoke both after patch and eversion carotid endarterectomy. Data was analysed using Mantel-Haenszel fixed effects model and heterogeneity of the measures obtained from selected studies was assessed through a Chi 2 test. Differences were considered statistically significant when P < 0.05. Figure 4 – Forest plot showing the relative risk calculated from data collected from the 7 selected studies that presented outcomes for neurological morbidity (transient ischemic attack and stroke combined) both after patch and eversion carotid endarterectomy. Data was analysed using Mantel-Haenszel fixed effects model and heterogeneity of the measures obtained from selected studies was assessed through a Chi2 test. Differences were considered statistically significant when P < 0.05. Figure 5 – Forest plot showing the relative risk calculated from data collected from the 7 selected studies that presented outcomes for death both after patch and eversion carotid endarterectomy. Data was analysed using Mantel-Haenszel fixed effects model and heterogeneity of the measures obtained from selected studies was assessed through a Chi2 test. Differences were considered statistically significant when P < 0.05. Figure 6 – Forest plot showing the relative risk calculated from data collected from the 7 selected studies that presented outcomes for morbimorbidity (neurological morbidity and death combined) both after patch and eversion carotid endarterectomy. Data was analysed using Mantel-Haenszel fixed effects model and heterogeneity of the measures obtained from selected studies was assessed through a Chi2 test. Differences were considered statistically significant when P < 0.05.