Allergic Rhinitis Guidelines - Supporting
advertisement
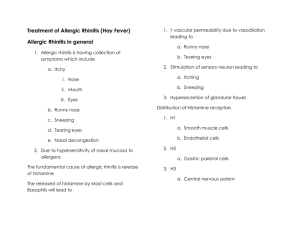
. Area Prescribing Committee Guideline . Allergic Rhinitis Management ; Part 2 This document contains the background supporting information to the document Allergic Rhinitis Management ; Summary Produced March 2010 (amended September 2010) Reviewed and updated May 2012. (Review date: May 2014) 1. Introduction Allergic rhinitis (AR) manifests as either seasonal allergic rhinitis (SAR), perennial allergic rhinitis (PAR) or as episodic AR occurring sporadically after specific exposures. The prevalence of SAR is between 10-30% for adults, up to 40% for children and continues to rise. Children of school age and adolescents are most commonly affected by SAR and poorly controlled symptoms may contribute to learning problems and sleep disturbance [van Cauwenburge et al, 2000; ARIA, 2001a]. Adults are more likely than children or adolescents to have PAR. Allergic rhinitis can be described by the timing of symptom occurrence (seasonal, perennial, episodic or occupational), by severity (mild or moderate to severe) and by persistence of symptoms (intermittent or persistent) [ARIA, 2001a]. 2. Aetiology and Diagnosis Allergic rhinitis is an inflammatory disorder of the nose which occurs when the membranes lining the nose become sensitised to allergens. Sensitisation results in allergen-specific immunoglobulin (Ig)E production which binds to the surface of mast cells in the lining of the nose. Re-exposure to the allergen results in allergen binding to IgE on the surface of mast cells triggering the release of histamine and other inflammatory mediators from the mast cells. Histamine and other inflammatory mediators act on cells, nerve endings, and blood vessels to produce the characteristic symptoms of of allergic rhinitis: sneezing, itching, nasal discharge (rhinorrhoea), and nasal blockage. Most cases of allergic rhinitis are diagnosed by identifying its characteristic features and excluding infectious and irritant causes of rhinitis. An allergic cause for rhinitis is more likely when there is a personal or family history of atopy (asthma, eczema, or allergic rhinitis). Examination is backed by skin prick or specific IgE allergy tests when necessary. 3. Prognosis Epidemiological studies have shown that allergic rhinitis is a risk factor for the development of asthma and many people develop asthma following the development of allergic rhinitis. Optimal management of allergic rhinitis may improve coexisting asthma and may prevent its development [ARIA, 2001b]. 4. Clinical management AR is highly responsive to treatment, and in most patients 1) education, 2) allergen avoidance and 3) appropriate use of medication can significantly reduce or eliminate symptoms [Farooque, 2009]. Standardised allergy education has been shown to improve disease specific quality of life. Education about the nature of the disease and available treatments, including general information about the symptoms, causes and mechanisms of rhinitis, relevant allergens and possible avoidance should be given. Patients also need information on pharmacotherapy: including how, when and how long to use it; details about safety and potential side effects should be provided. Patients should understand that complete cure is unlikely and that long term treatment may be needed. Patients should be made aware of the potential negative impact of rhinitis on their quality of life, on possible co-morbidities and benefits of complying with therapeutic recommendations. 5. Allergen identification and avoidance Avoidance of confirmed animal allergens is considered important to control symptoms of allergic rhinitis and reduce the risk of asthma developing [Scadding et al, 2008]. ]. Allergy testing should be considered when it is not possible to distinguish from the history the type of rhinitis present Page 1 of 9 (infective, irritant or allergic) or the likely allergen causing allergic rhinitis. Skin tests are more simple, sensitive, faster, and more cost effective than in vitro IgE testing. Antihistamines should be stopped 7-10 days before skin testing, but do not need to be stopped prior to IgE serum tests. 6. Intranasal steroids • Intranasal corticosteroids are the most potent medications available for treating allergic rhinitis [A]. They control itching, sneezing, rhinorrhea, and obstruction in most patients, but do not completely alleviate ocular symptoms. They have a relatively good long-term safety profile. •When comparing the available intranasal corticosteroids, the overall clinical response does not appear to vary significantly between products irrespective of the differences in topical potency, lipid solubility, and binding affinity [C]. Choice is therefore based on cost and patient preference. •Intranasal corticosteroids may provide significant relief of symptoms of seasonal allergic rhinitis when used not only on a regular basis but also on an as-needed basis [B]. However, as-needed use may not be as effective as continuous use of intranasal corticosteroids [D]. •Their effect is not immediate, however; onset of relief is seen on day 2 to 3 with effects reaching their peak at 2 to 3 weeks. Regular, consistent use is required to maintain a maximum effect. Patient education for the correct use of intranasal pump sprays is essential. Advise people who have recurrent episodes of allergic rhinitis controlled by intranasal corticosteroids to restart treatment at least 7 days before re-exposure to allergen. When the time of re–exposure to antigen is uncertain, such as the start of the pollination season, start treatment several weeks before the most likely time of re–exposure. •Intranasal corticosteroids when given in recommended doses are not generally associated with clinically significant systemic side effects in adults [A]. Systemic effects caused by intranasal corticosteroids are rare as they have relatively short half-lives, topical activity, and rapid first-pass metabolism [Yawn, 2006]. Adverse effects Although local side effects are typically minimal with the use of intranasal corticosteroids, nasal irritation and bleeding may occur. Nasal septal perforation is rarely reported [B]. These can be avoided with proper administration technique. Concomitant use of other corticosteroids When prescribing intranasal corticosteroids, take into account the use of other systemic and topical corticosteroids (e.g. creams, ointments, and inhalers). The effect of these drugs is probably additive and therefore requires close monitoring. Recommendations for children In children, an effect of intranasal corticosteroids on growth has been demonstrated, although an effect on the HPA axis has not been demonstrated and no reduction in bone density or other systemic effects have been reported. Growth Concerns about possible adverse effects on growth raise special considerations. Growth suppression, assessed by stadiometer height measurement, was detected in children with perennial allergic rhinitis treated with intranasal beclometasone dipropionate for 1 year at twice the usually recommended dose. Growth suppression from intranasal corticosteroids has been reported only with long-term use of beclometasone dipropionate that exceeded recommended doses or administration to toddlers. Similar studies with intranasal budesonide, fluticasone propionate and mometasone furoate show no effects on growth compared with placebo (at recommended doses) and reference values (at as much as 2 times recommended doses), except in toddlers. The CSM recommends that the height of children receiving prolonged treatment with nasal corticosteroids is monitored; if growth is slowed, referral to a paediatrician should be considered. Budesonide, mometasone furoate and fluticasone propionate are recommended first line for children based on these studies. Page 2 of 9 Nasal drops Betamethasone and fluticasone drops may be useful short-term, for treating nasal polyps, and for the relief of severe nasal congestion [Scadding et al, 2008]. The risk of systemic effects may be greater with nasal drops than with nasal sprays; drops are administered incorrectly more often than sprays. To administer nasal drops correctly the following procedure should be adopted: Advise the patient to either tilt their head backwards, ensuring it is supported, or lie flat on their back with the head tilted backwards. Place as many drops as has been prescribed into the nostril. If necessary, squeeze the bottle gently to allow the drops to fall. Keep the head tilted and encourage the patient to sniff gently to let the drops penetrate. If required repeat for the other nostril. Oral corticosteroids A short course (5-7 days) of oral corticosteroids may be appropriate for the treatment of very severe or intractable nasal symptoms or to treat significant nasal polyposis. 7. Oral antihistamines •Second-generation antihistamines are generally preferred over first-generation (sedating) antihistamines for the treatment of allergic rhinitis. First-generation antihistamines have significant potential to cause sedation, performance impairment, and anticholinergic effects. Although occasionally advantageous (eg, sleep induction when taken at bedtime or a reduction in rhinorrhea), these properties are usually undesirable and are potentially dangerous. Secondgeneration antihistamines have less or no tendency to cause these effects [B]. •Non-sedating antihistamines prevent and relieve itching, sneezing, and rhinorrhea, but tend to be less effective for nasal congestion [A]. Among the non-sedating antihistamines, no single agent has been has conclusively found to achieve superior overall response rates [C]. •There are important differences among the second-generation antihistamines in regard to their sedative properties: fexofenadine (non- sedating active metabolite of terfenadine), loratadine, and desloratadine do not cause sedation at recommended doses; loratadine and desloratadine may cause sedation at doses exceeding the recommended dose; cetirizine and intranasal azelastine may cause sedation at recommended doses [A] • Loratadine. cetirizine and fexofenadine are recommended 1st line for the treatment of allergic rhinitis. •Desloratadine (a metabolite of loratadine) and levocetirizine (an isomer of cetirizine) are more recently marketed products, but there is little evidence to confirm whether they confer any additional benefit over the more established non-sedating antihistamine. Mizolastine and rupatidine have been implicated in causing an abnormal prolongation of the QT interval and are therefore not recommended as a first-line treatment option. Intranasal antihistamines • Intranasal antihistamines have been associated with a clinically significant effect on nasal congestion [A] but are generally less effective than intranasal corticosteroids for treatment of allergic rhinitis [A]. • Intranasal azelastine has demonstrated efficacy for seasonal allergic rhinitis superior or equal to oral second-generation antihistamines [A] and a clinically significant onset of action has been reported at 15 minutes. Intranasal azelastine (applied two to four times daily) is the only intranasal antihistamine that is available and licensed in the UK for the treatment of allergic rhinitis. • Intranasal antihistamines may be considered for use as first line treatment for allergic rhinitis [A] 8. Douching with nasal saline Page 3 of 9 •Topical saline is commonly used as a treatment for rhinitis and rhinosinusitis in both children and adults. There is evidence that it is beneficial in the treatment of the symptoms of chronic rhinorrhea when used alone or for adjunctive treatment [A]. •Although less effective than intranasal corticosteroids and no more effective than other active agents for rhinitis, isotonic and hypertonic saline solutions, used as either single or adjunctive agents, are of modest benefit for reducing symptoms and improving the QOL in patients with allergic rhinitis. Therefore, saline solution can be an effective adjunctive medication for mild-tomoderate allergic rhinitis. •Various mechanisms, such as improvement in mucus clearance; enhanced ciliary beat activity; removal of antigen, biofilm, or inflammatory mediators; and a protective effect on sinonasal mucosa, have been proposed but not confirmed to explain the reported symptom improvement. Saline solutions also contain magnesium, which possibly reduces inflammation in the nasal mucosa. The use of topical saline is associated with minimal side effects, such as burning, irritation, and nausea; has low cost; and has overall good patient acceptance. •In one 4-week study, the use of saline as a wetting agent for perennial rhinitis demonstrated reduced sneezing and nasal stuffiness, reduced nasal blockage (measured by peak flow), and a reduction in eosinophils (nasal biopsy). Overall, there is no difference in symptom or radiologic scores when comparing isotonic with hypertonic saline. 9. Decongestants •Oral decongestants, such as pseudoephedrine and phenylephrine, are α-adrenergic agonists that produce vasoconstriction and decrease swelling of the nasal mucosa to reduce nasal congestion but can result in side effects such as insomnia, irritability, and palpitations [A]. Oral and topical decongestants agents should be used with caution in older adults and young children, and in patients of any age who have a history of cardiac arrhythmia, angina pectoris, cerebrovascular disease, hypertension, bladder neck obstruction, glaucoma, or hyperthyroidism [C]. Oral decongestants are contraindicated in patients using monoamine oxidase inhibitors (MAOIs) or having uncontrolled hypertension or severe coronary artery disease. •Oral decongestants, when used in appropriate doses, are usually very well tolerated in children over 6 years of age. However, use in infants and young children has been associated with agitated psychosis, ataxia, hallucinations, and even death. At times, even at recommended doses these agents may cause increased stimulatory effects resulting in tachyarrhythmias, insomnia, and hyperactivity, especially when combined with other stimulant medications, such as stimulants used in attention deficit hyperactivity disorder management. Therefore, the risks and benefits must be carefully considered before using oral decongestants in children below age 6 years. •Topically applied sympathomimetic decongestant α -adrenergic vasoconstrictors, are catecholamines, such as phenylephrine, or imidazoline agents, such as oxymetazoline or xylometazoline. These medications cause nasal vasoconstriction and decreased nasal oedema to reduce nasal obstruction but have no effect on antigen provoked nasal response and do not affect itching, sneezing, or nasal secretion. •Topical decongestants can be considered for short-term (3-5 days typically and no more than 7 days) and possibly for intermittent or episodic therapy of nasal congestion, but are inappropriate for regular daily use because of the risk for the development of rhinitis medicamentosa [C] [ARIA, 2001a; Saleh and Durham, 2007]. •The development of rhinitis medicamentosa is highly variable; it may develop within 3 days of use or fail to develop after 6 weeks of daily use. Topical decongestants can be associated with local stinging or burning, sneezing, and dryness of the nose and throat. Intermittent use of topical decongestants is frequently prescribed; however, the efficacy and safety of this approach have not been formally studied. 10. Oral leukotriene receptor antagonists (LTRAs) • Leukotriene inhibitors are effective in the treatment of seasonal and perennial allergic rhinitis but less effective than intranasal corticosteroids (even when combined with antihistamines) [A]. Leukotriene inhibitors are the newest class of medications used for allergic rhinitis. They reduce allergy symptoms through inhibition of inflammation and also have proven efficacy for control of Page 4 of 9 asthma. Montelukast (Singulair®), the only LTRA licensed for AR in the UK, has an excellent safety profile and several large studies have shown a reduction in itching, sneezing, rhinorrhea, and congestion. The onset of action occurs by the second day of daily treatment. •As many as 40% of patients with allergic rhinitis have coexisting asthma. Because montelukast has been improved for both rhinitis and asthma, it may be considered in such patients. There is no significant difference in efficacy between LTRA and antihistamines (with loratadine as the usual comparator), and their concomitant use may be additive. •Montelukast is a safe and effective treatment for the management of allergic rhinitis in children. It is approved for perennial allergic rhinitis in children as young as 6 months and for seasonal allergic rhinitis in children as young as 2 years. •The Scottish Medicines Consortium has advised (June 2007) that Singulair® chewable tablets and granules are restricted for use as an alternative to low-dose inhaled corticosteroids for children 2– 14 years with mild persistent asthma who have not recently had serious asthma attacks that required oral corticosteroid use and who are not capable of using inhaled corticosteroids; Singulair® chewable tablets and granules should be initiated by a specialist in paediatric asthma [BNF 58, 2010]. 11. Intranasal sodium cromoglicate •Sodium cromoglicate, an inhibitor of mast cell degranulation, is effective in the prevention of symptoms and in the treatment of AR. It has a strong safety profile and has a reported onset of action of 4 to 7 days for seasonal or perennial rhinitis. When used to treat symptoms of seasonal allergic rhinitis, sodium cromoglicate should be started as early in an allergy season as possible. It can be used as an alternative treatment option to antihistamines and intranasal corticosteroids (e.g. if people do not tolerate them) but it is less effective in most patients than corticosteroids and has not been adequately studied in comparison with LT antagonists and antihistamines [A]. •Some people may experience local irritation on application; however, sodium cromoglicate is very well tolerated and is the safest drug recommended for allergic rhinitis in the first 3 months of pregnancy [ARIA, 2001a; Scadding et al, 2008]. A disadvantage from a patient preference and compliance perspective is that it requires frequent dosing (up to 4 times a day) to be effective. 12. Anticholinergics •Intranasal anticholinergics may effectively reduce rhinorrhea but have no effect on other nasal symptoms. Although side effects are minimal, dryness of the nasal membranes may occur [A]. The concomitant use of ipratropium bromide nasal spray and an intranasal corticosteroid is more effective than administration of either drug alone in the treatment of rhinorrhea without any increased incidence of adverse events [A] •Intranasal ipratropium bromide (Atrovent) is an effective anticholinergic spray add-on option for rhinorrhea associated with allergic rhinitis. It has no adverse effect on physiologic nasal functions (eg, sense of smell, ciliary beat frequency, or mucociliary clearance) and has a low incidence of adverse events, in particular epistaxis and nasal dryness. •The nasal anticholinergic ipratropium bromide is effective in reducing rhinorrhea caused by allergic rhinitis, Ipratropium bromide is only approved (down to the age of 5 years) for the treatment of rhinorrhea. Ipratropium needs to be sprayed twice into each nostril, two or three times daily. Localised adverse effects such as nosebleed, irritation, soreness and nasal dryness are common but not usually severe [BNF 54, 2007; Scadding et al, 2008]. Ipratropium should be used with caution in people at risk of closed angle glaucoma as there have been case reports of ipratropium causing this [Baxter, 2006; Scadding et al, 2008]. •Anticholinergics decrease the production of mucus and diminish rhinorrhea. Both topical medications and oral preparations (usually first-generation antihistamines) have been shown to be effective. One therapeutic effect of the first generation antihistamines is related to their anticholinergic properties. Therefore newer, less-sedating antihistamines are less likely to produce this benefit. •Ipratropium bromide nasal spray 0.03% has been approved for use in patients 6 years of age and older on the basis of its effectiveness in treating rhinorrhea caused by perennial allergic and nonallergic rhinitis in adults and children. 13. Ocular medications for eye symptoms Page 5 of 9 •Allergic rhinitis is often accompanied by allergic conjunctivitis [C]. with symptoms of itchy eyes and tearing, typically affecting both eyes. Ocular preparations should be considered for patients with allergic conjunctivitis who are not adequately controlled with or can not tolerate an oral antihistamine. •Intranasal corticosteroids, oral antihistamines, and intranasal antihistamines have similar effectiveness in relieving ocular eye symptoms associated with rhinitis. •Use of cold compresses and irrigation with saline solution or artificial tears has been advocated to relieve mild symptoms of allergic conjunctivitis. A variety of topical ophthalmic agents are indicated for specific treatment of itching or symptoms of allergic conjunctivitis. They contain antihistamines or mast cell stabilisers. Side effects of ocular medications are generally mild and include a brief stinging, burning sensation. Ocular antihistamines can be used as needed for acute symptomatic relief and prophylaxis of allergic symptoms with minimal systemic side effects. •In systematic reviews of randomized controlled studies, intranasal corticosteroids compared with oral antihistamines and intranasal corticosteroids compared with intranasal antihistamines were not significantly different in relieving eye symptoms. •In placebo- controlled studies of adults, fluticasone furoate nasal spray has been demonstrated to reduce significantly ocular symptoms associated with seasonal allergic rhinitis. •Antihistamines (H1-receptor antagonists) are available in OTC and prescription ophthalmic preparations and are sometimes combined with a topical vasoconstrictor for acute relief of ocular allergy symptoms. The combination of an antihistamine and a vasoconstrictor works better than either agent alone. •Mast cell stabilizers have a slow onset of action and may require several days of treatment before optimal symptom relief is achieved, making them more suitable for prophylactic or longer-term treatment of chronic ocular allergies than for acute symptom relief. They are also approved for chronic ocular allergy conditions involving corneal defects including vernal keratoconjunctivitis and atopic keratoconjunctivitis. •Topical NSAIDs reduce prostaglandin production involved in mediating ocular allergy. Ketorolac is indicated for temporary relief of ocular itching caused by seasonal allergic conjunctivitis. •Multiple-action agents possess both antihistamine and mast cell stabilizer activities, generally have onset of action within 30 minutes, and are suitable for acute and longer-term treatment of allergic conjunctivitis symptoms. •Ocular corticosteroids should be reserved for more severe symptoms of allergic conjunctivitis in consideration that ocular side effects from their use can be vision-threatening, and include cataract formation, elevated IOP, and secondary infections. 14. Immunotherapy (hyposensitisation) •Refer for consideration for immunotherapy when symptoms of allergic rhinitis persist on maximal medical therapy. Immunotherapy is carried out in secondary care. It is suitable treatment for people sensitised to certain allergens but not suitable for people with multiple sensitivities. •It involves administering increasing quantities of an allergen to an allergic person in order to reduce their allergic response to that allergen with subsequent exposure [ARIA, 2001a]. Immunotherapy is the only treatment which alters the course of disease and is very effective for severely affected patients with one or two major allergens who are insufficiently responsive to pharmacotherapy [A]. Well controlled clinical trials have demonstrated its effectiveness for seasonal and perennial allergic rhinitis, seasonal asthma, and ocular allergy. It may prevent polysensitisation to other allergens in children and prevent the development of asthma [B]. Allergen immunotherapy is effective in both adults and children. Its efficacy is confirmed for the treatment of inhalant allergy caused by pollen, fungi, animal allergens, dust mite, and cockroach. No long term effects have been reported. •Unlike pharmacotherapy, the clinical benefits may be sustained years after discontinuation of treatment. Immunotherapy is usually not more costly than pharmacotherapy over the projected course of treatment. •Subcutaneous immunotherapy (e.g. Pollinex® for grasses and rye or tree pollen allergy) carries the potential for severe systemic side effects and so is only available in specialised centres with trained personnel and the availability of cardio-pulmonary resuscitation. Subjects must be observed for an hour post each injection. Three years treatment is associated with a good reduction in symptoms for several years thereafter. •Sublingual immunotherapy is probably less effective but considerably safer since the reaction is local rather than systemic. The recommendation is for the first dose to be administered under Page 6 of 9 observation, with subsequent doses being taken daily at home. In the UK at present only one form is licensed -tablets for grass pollen allergy (Grazax®). •Allergen specific subcutaneous immunotherapy has been associated with a reduction in nonspecific bronchial hyperresponsiveness (BHR) in patients with perennial allergic rhinitis. Several controlled studies have also reported a reduction in the incidence of asthma in pediatric patients with allergic rhinitis treated with subcutaneous immunotherapy, and this effect appears to be sustained at least 2 years after discontinuing immunotherapy. •Contraindications for allergen immunotherapy include patients with medical conditions that would reduce their ability to survive allergen immunotherapy systemic allergic reactions or the resultant treatment. Examples include severe asthma uncontrolled by pharmacotherapy and significant cardiovascular disease. Clinical improvement can be demonstrated very shortly after the patient reaches a maintenance dose. •In general, there is insufficient evidence to support the efficacy of immunotherapy for IgEdependent occupational rhinitis, and it is inappropriate to use immunotherapy to treat occupational rhinitis caused by low-molecular-weight chemical allergens. 15. Pregnancy •If possible, medication should be avoided in the first trimester because of the potential risk of congenital malformations in the first trimester, when organogenesis is occurring [D]. •For mild to moderate nasal symptoms of allergic rhinitis, nasal saline irrigation is safe and effective. •A sufficient amount of human observational data has now been accumulated to demonstrate safety for second-generation as well as first-generation antihistamines [C]. First-generation antihistamines, such as chlorphenamine, have previously been recommended as first-choice agents because of their observed safety and longevity of use. However, their undesirable sedative qualities and possible effect on performance may make them less desirable choices. The safety of second-generation antihistamines used during the first trimester of pregnancy has now been confirmed through large birth registries, case-control studies, and cohort studies. The accumulated safety data during pregnancy on the second-generation antihistamines are comparable to those of the first-generation antihistamines. •The oral antihistamines chlorphenamine, loratadine and cetirizine are recommended by many experts for use in pregnancy if an oral antihistamine is required [Schaefer et al, 2007], and loratadine and cetirizine are recommended for use in breastfeeding [Schaefer et al, 2007]. If prescribing an oral antihistamine, the provider should choose either: • second-generation agents, loratadine or cetirizine (both category B) or • first-generation antihistamine chlorphenamine (category B) •loratadine is recommended as first-line because there is more safety data available than for cetirizine, and it is not associated with having the sedative properties of chlorphenamine. Antihistamine Loratidine (2nd generation) Cetirizine (2nd generation) Chlorphenamine (1st generation) FDA pregnancy category B B B •Both first-generation and second-generation antihistamines in general have excellent safety records and do not show a significant increase in congenital malformations when used during the first trimester. However, caution is still advised for a few antihistamines. Hydroxyzine should be used cautiously during the first trimester based on animal data. Although there are no reports of increased congenital malformations with the use of fexofenadine during pregnancy and animal studies are negative for teratogenicity, no epidemiologic studies in human pregnancy have been published. Currently there are also limited data on desloratadine, azelastine, and levocetirizine. •Intranasal corticosteroids may be used during pregnancy because of their safety and efficacy profile [C] [Demoly et al, 2003]. Clinical and epidemiologic studies on safety in human beings are Page 7 of 9 limited. Although most intranasal corticosteroids are given an FDA Pregnancy Category C rating, gestational risk has not been confirmed in observational human data. A recent meta-analysis concluded that the use of intranasal corticosteroids during pregnancy does not increase the risk of major malformations, preterm delivery, low birth weight, and pregnancy-induced hypertension. •The reported safety data on all intranasal corticosteroids have been reassuring, but beclometasone, budesonide (Pregnancy Category B), and fluticasone propionate have more accumulated data (demonstrating no convincing evidence of congenital defects) than triamcinolone, mometasone, and flunisolide. Because no substantial difference in efficacy and safety has been shown among the available intranasal corticosteroids, it would be reasonable to continue any of the intranasal corticosteroids that have adequately controlled the patient’s symptoms before pregnancy. •If intranasal corticosteroids are started during pregnancy, intranasal budesonide, which is Pregnancy Category B, largely on the basis of extensive human safety data, may be preferred (all other intranasal corticosteroids are rated category C). As with all medication use in pregnancy, intranasal corticosteroids should be administered at the lowest effective dose. •Intranasal corticosteroids may also be used to allow discontinuation of topical decongestants in patients with rhinitis medicamentosa. As with all medication use in pregnancy, intranasal corticosteroids should be tapered to the lowest effective dose. •Oral decongestants should be avoided during the first trimester because of conflicting reports of an association of phenylephrine and pseudoephedrine with congenital malformations such as gastroschisis and small intestinal atresia. Likewise, the data on the safety of topical intranasal decongestants during pregnancy have not been studied. •Sodium cromolyn (Pregnancy Category B) is a safe treatment for allergic rhinitis during pregnancy in view of its topical application and reassuring gestational human and animal data [C]. Unfortunately the need for frequent 4 times a day dosing and reduced relative efficacy compared with other agents limits its acceptance by patients. •Montelukast (Pregnancy Category B) is a safe treatment for allergic rhinitis during pregnancy [C] with reassuring animal reproductive studies and unpublished human safety data. •Immunotherapy for allergic rhinitis may be continued during pregnancy but without dose escalation [C] if it is effective and not causing significant reactions. The benefit/ risk considerations do not generally favour starting immunotherapy during pregnancy. 16. Paediatrics For children with occasional symptoms, antihistamines can be taken on days when symptoms are present or expected. Children experiencing daily symptoms achieve the most relief when taking antihistamines continuously throughout the pollen season. Second-generation, less-sedating, antihistamines should be used for school-age children. Intranasal corticosteroids, especially mometasone, have demonstrated an excellent safety profile in children with minimal systemic absorption and no evidence of growth retardation [A]. Systemic effects caused by intranasal corticosteroids are rare as intranasal corticosteroids differ from oral corticosteroids in that they have relatively short half-lives, topical activity, and rapid firstpass metabolism [Yawn, 2006]. Despite this, the Commission on Human Medicine (formerly Committee on Safety of Medicines) recommends that the height of children receiving high doses over extended periods be frequently monitored, and treatment reviewed if any effect on growth is observed. Bioavailability of budesonide, fluticasone and mometsaone is negligible, for others INS it is modest (BSACI, 2007). Budesonide, fluticasone, and mometasone are the preferred INS in children. Experts recommend these because there is trial data available that has shown they appear to cause no adverse effects on growth in children [Schenkel et al, 2000; Yawn, 2006]. Two placebo-controlled studies of budesonide aqueous nasal spray and fluticasone propionate nasal spray have shown no significant effects on the speed of growth in children after 1 year of treatment, but similar placebo-controlled trials for other corticosteroids and comparative studies are lacking [Yawn, 2006]. In general, treatment of allergic rhinitis is the same in children as it is in adults (see licenses for age). Oral antihistamines cetirizine and loratadine are licensed for use in children from 2 years of age. Intranasal antihistamines can be used from 5 years of age onwards. Intranasal sodium cromoglicate is suitable for use in children. It is less effective than oral antihistamines and intranasal corticosteroids, but can be used in place of these treatments when they are not acceptable. Intranasal decongestants: some intranasal products are available specifically for children older than 3 months of age but should only be used for up to 7 days duration [BNF 58, 2010]. Page 8 of 9 Levels of evidence reflect the best available literature in support of an intervention or test: A=randomized controlled trials; B=controlled trials, no randomisation; C=observational trials; D=opinion of expert panel. Essential Evidence-based guidelines Angier E, Willington J, Scadding G et al. Management of allergic and non-allergic rhinitis: a primary care summary of the BSACI guideline. Primary Care Respiratory Journal. 2010; 19(3): 217-222. Available at: http://www.thepcrj.org/journ/vol19/19_3_217_222.pdf Accessed <11.10.11> ARIA (2001a) Allergic rhinitis and its impact on asthma. ARIA workshop report. Journal of Allergy and Clinical Immunology 108(5 Suppl), 1-205. ARIA (2001b) Management of allergic rhinitis and its impact on asthma: a pocket guide for physicians and nurses. Allergic Rhinitis and its Impact on Asthma. Scadding, G.K., Durham, S.R., Mirakian, R., et al. (2008) BSACI guidelines for the management of allergic and non-allergic rhinitis. Clinical and Experimental Allergy 38(1), 19-42. University of Michigan Health System (2007) Guidelines for clinical care: allergic rhinitis. University of Michigan Health System. Available on http://cme.med.umich.edu [accessed on 10/03/10] Wallace, D.V., Dykewicz, M.S, Bernstein, D.I., et al. (2008) The diagnosis and management of rhinitis: an updated practice parameter. Journal of Allergy and Clinical Immunology 122(2 Suppl), S1-S84. Other references Al Sayyad, J.J., Fedorowicz, Z., Alhashimi, D. and Jamal, A. (2007) Topical nasal steroids for intermittent and persistent allergic rhinitis in children (Cochrane Review). Issue 1. John Wiley & Sons, Ltd. www.thecochranelibrary.com BNF 59 (2010) British National Formulary. 59th edn. London: British Medical Association and Royal Pharmaceutical Society of Great Britain. CSM (1998) The safety of inhaled and nasal corticosteroids. Committee on Safety of Medicines. Current Problems in Pharmacovigilance 24(May), 8-9. Demoly, P., Piette, V. and Daures, J.P. (2003) Treatment of allergic rhinitis during pregnancy. Drugs 63(17), 1813-1820. Farooque, S. Diagnosis, allergen avoidance and treatment of allergic rhinitis. Prescriber, 19 May 2009, 38-48. Saleh, H.A. and Durham, S.R. (2007) Perennial rhinitis. British Medical Journal 335(7618), 502-507. Schaefer, C., Peters, P. and Miller, R.K. (Eds.) (2007) Drugs during pregnancy and lactation: treatment options and risk assessment. 2nd edn. Oxford: Academic Press. Schenkel, E.J., Skoner, D.P., Bronsky, E.A. et al. (2000) Absence of growth retardation in children with perennial allergic rhinitis after one year of treatment with mometasone furoate aqueous nasal spray. Pediatrics 105(2), E22. Sheikh, A., Panesar, S.S., Dhami, S. and Salvilla, S. (2007a) Seasonal allergic rhinitis in adolescents and adults. Clinical Evidence. BMJ Publishing Group Ltd. www.clinicalevidence.com Sheikh, A., Hurwitz, B. and Shehata, Y. (2007b) House dust mite avoidance measures for perennial allergic rhinitis (Cochrane Review). Issue 1. John Wiley & Sons, Ltd. www.thecochranelibrary.com Yawn, B. (2006) Comparison of once-daily intranasal corticosteroids for the treatment of allergic rhinitis: are they all the same? MedGenMed: Medscape General Medicine 8(1), 23. For clarification of any points within this guidance please contact the Medicines Management Team on 01226 433798 Page 9 of 9