SPRING IS IN THE AIR - The COSHAR Foundation
advertisement

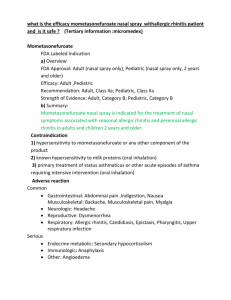
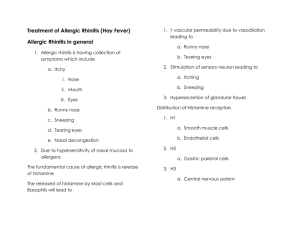
SPRING IS IN THE AIR Watch out for Allergic Rhinitis (Seasonal Allergies) Greater than 15 % of the North American population suffer from allergic rhinitis, commonly known as seasonal allergies or hay fever. This estimate is considered low because so many people mislabel their sniffling and sneezing as symptoms of a cold or sinus problems. Therefore, allergic rhinitis is undoubtedly underdiagnosed. The most common allergic reaction is caused by pollen in the spring, grasses in the summer, and ragweed in the fall. Other causes of year round symptoms include dust and household mites that are found on your linen and carpets. Do you suffer from seasonal allergies? Common Symptoms (Check all that apply) Nasal Congestion Runny Nose Sneezing Itching (especially around your eyes and on the roof of your mouth) Watery, Swollen Eyes Headache Fatigue (Extreme tiredness) There are other causes of the symptoms which could be as a result of exposure to “Irritants” including cigarette smoke, strong perfumes/colognes, perfumed soaps, cosmetics, household cleaning products/detergents, hairspray, outside dust, exhaust from cars, trucks and/or buses, gasoline fumes. Further symptoms may be caused by changes in the weather including windy, cold, damp days and/or any humidity changes. Finally there are certain foods that you may ingest that may trigger the symptoms such as alcoholic beverages (beer, wine) and spicy foods. Rhinitis associated with any of these irritants is diagnosed as “Vasomotor Rhinitis”. However, many people have a “Mixed Rhinitis” as they have symptoms to both allergens (molds, grass, etc…) and irritants (fumes, weather changes, etc…). The diagnosis can only be made by a complete evaluation by your physician; you can greatly help with the evaluation by bringing in a written list of your observations, which should include: 1. When your symptoms began 2. When and how often you get symptoms 3. Where your symptoms appear (i.e. at school, outside, at home) 4. What medicines you are taking, including over-the- counter products (non-prescription and herbal) 5. Any personal or family history of allergies and/or asthma There is hope and treatment available to help with these symptoms. Prevention and proper diagnosis is key. Preventive measures include avoiding “triggers” by covering mattresses and pillows with plastic covers, remove dust collecting items in the house such as carpet, drapes and wicker furniture, air purification systems and dust filters may also be effective. Another good idea is to ban tobacco smoking from your home. Tobacco smoke can irritate nasal passages that are clogged, throats that are scratchy and raw, and eyes that are red and watery already from allergens. It is often impossible to totally avoid your triggers; for example if your trigger is pollen, it is very difficult to prevent reactions unless you confine yourself to your home, which is not practical for most persons. In this instance you would need to limit your exposure to the outdoors during days with high pollen counts, leave for work early and come home later in the evening, keep your windows closed during high pollen seasons and use air conditioning in your home and in your car, avoid drying your clothes by hanging them up outside—you would to use the dryer or hang them inside. Further preventive measures would include avoiding mowing the lawn as that sirs up the pollen, limit your time near fresh-cut grass and if your must mow, wear a mask. It is generally recommended that you keep your lawn short (under 2” high) to keep the weeds from flowering and increasing your pollen exposure. In addition to preventive measures, a simple but effective nonpharmalogic intervention is the use of steam inhalation to relieve the congestion and stuffy nose. This can be achieved by running hot water in a sink basin or bowl and putting a towel over your head, creating a covering as you put your head over the basin and taking nice, slow deep breaths. A spoonful or two of mixed honey and lemon juice is noted for soothing scratchy throats. Gargling with a strong solution of table salt and warm water can also bring you some relief. Other medical options to use inconjunction with preventive measures will need to be discussed with your physician. Your options may include over the counter antihistamines and/or decongestants (ex. Sudafed, Actifed), prescription antihistamines and/or decongestants (ex: Allegra, Zyrtec and/or Claritin), saline nasal sprays, steroid nasal sprays, and other medications. There are some herbal remedies that may help with relief of symptoms, for example, goldenseal. As with all medications there are side effects and you should consult your physician before taking any medication including over the counter and herbal remedies. Seasonal allergic rhinitis do not require antibiotic treatment, however often persons will develop a sinus infection during this period. You will need to pay close attention to any signs of bacterial infection, which may include fever, yellow or greenish nasal discharge along with the other symptoms. If you do develop these symptoms or are unsure of infection, contact your physician and he/she will decide if antibiotic therapy is indicated. Further treatment options for allergic rhinitis include allergy shots (immunotherapy), which are usually reserved for very severe cases. Generally, a good evaluation by your Internist or family physician should be sufficient for evaluation and treatment. However, in more severe cases, you may be referred to an allergy specialist. Don’t let seasonal allergies rob you of a wonderful spring and summer, get the help you need.