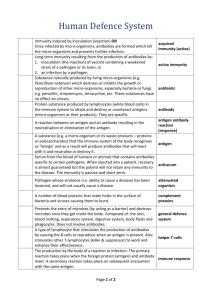
Cell Type
advertisement

ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 17 Integrated Defence System Immune responses can be subdivided into two categories – innate (natural) and acquired (antigen-specific). Innate immunity is present at birth and is not related to previous exposure. Innate immunity involves non-specific defence strategies, which prevent the entry and limit the spread foreign invaders. ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 18 Innate (Non-specific defences) Physical and chemical barriers make up the body’s first line of defence – if you can keep invaders out, they cannot harm the body. Physical barriers include the skin, mucous membranes of the conjunctiva, respiratory tract, as well as gastrointestinal and genitourinary tracts. Chemical barriers include stomach acid, which disables swallowed pathogens, and lysozyme, which attacks and digests bacteria. In addition to physical and chemical barriers, a number of other public safety groups are involved in non-specific defence: phagocytes (neutrophil, monocyte/macrophage, eosinophil) engulf debris and foreign invaders (discussed earlier – link to phagocytosis) specialized lymphocytes known as natural killer (NK) cells perform immunological surveillance in the tissues and destroy abnormal (cancerous) and virus infected cells (air-force surveillance or elite force of marksmen) interactions between specialized lymphocytes that capture foreign antigens (T-lymphocytes or T-cells and “present” them to another specialized type of lymphocyte (B-lymphocytes or B-cells) stimulating antibody production a complex chemical communication system that coordinates defence against viral infection complement – a system of proteins that assist antibodies the inflammatory response that restricts the spread of invasion and is involved in emergency response – paramedics, fire-fighters and police fever accelerates metabolism and enhances immune response Lymphocytes As you will recall, there are three main types of lymphocytes – B-cells, T-cells and NK cells. Link to antibody production: http://www.cellsalive.com/antibody.htm B-cells B-cells are produced in the bone marrow (“b” for bone) and are involved in protection conferred by antibodies (humoral immunity). In the bone marrow, Bcells mature to the point where they express antigen receptors – IgM antibodies – on their surfaces. Once matured (trained and armed), they move out of the bone marrow (training center) to lymphoid organs (military bases such as the spleen and lymph nodes). Link to B-cell maturation: http://www.bio.davidson.edu/Courses/immunology/Flash/Bcellmat.html ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 19 The surface of each B-lymphocyte is coated with as many as 100,000 nonsensitized antibody molecules attached to the B-cell surface by their Fc ends (base of the “Y” structure of the antibody molecule), and arms (Fab segments) extended like antennae sniffing out foreign antigens. B-lymphocyte antibodies bind to viruses and bacterial toxins to prevent them from affecting host cells and begin production of antibodies specific for the antigen detected. Link to Antibody molecule: http://www.biology.arizona.edu/immunology/tutorials/antibody/structure.html There are millions of different populations of B-cells in the body, each population binds to specific antigens circulating in the blood stream and becomes activated (sensitized). The IgM antibodies expressed on the surface of the B-cells are capable of responding to one specific antigen or to a few closely related antigens. Once dispatched to an alert (chemical communication forces at site of invasion – phagocytes, memory cells) resulting from detection of foreign antigen in the home nation, B-cells become activated by contact with the foreign antigen and confirmation provided by T-cell binding to the target cell surface – T-cells provide the second key or code for weapons use. Activated B-cells (pleural) begin cloning two forms of it-self (singular) – memory cells and plasma cells. Plasma cell production greatly outnumbers memory cell production at this point, and following initial activation, B-cells generally change their antibody class from IgM to IgG, IgA, and sometimes IgE (Link to page 15 – Antibody classes and link from page 15 back to page 9). Changes in antibody class are directed by cytokines produced by T-cells. Memory cells do not take part in the initial direct battle – they persist, travelling the nation after the enemy has been defeated providing rapid preliminary defence and calling out new forces (chemical communication) if the antigen ever attempts to re-enter. B-cells also possess a variety of receptors on their surface including complement receptors and glycoproteins. The structure of these glycoproteins is genetically determined and coded by major histocompatability complex (MHC) proteins. There are two classes of MHC protein – Class I and Class II. MHC proteins are also known as human leukocyte antigens (HLA). MHC class I (MHC-I) proteins are found on all nucleated cells, while MHC class II (MHC-II) proteins are found mainly on macrophages, B-cells, and dendritic cells. Link to MHC I antigen http://www.bio.davidson.edu/Courses/immunology/Flash/MHCI.html loading: ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 20 Link to MHC II antigen http://www.bio.davidson.edu/Courses/immunology/Flash/MHCII.html loading: When viruses or bacteria invade a cell, they are ingested and disassembled into fragments inside the cell (weapon destruction program), loaded onto an MHC-I or MHC-II platform, and delivered to the cell surface for display (through a process known as exocytosis). The number of B-cells is enormous – only about one in every 100,000 B-cells will recognize a specific antigen. T-cells T-cells develop in the thymus gland (“t” for thymus) from immature lymphocytes that migrate there from the bone marrow. T-cells may be found in the thymus, lymph nodes and blood circulation. There are three types of T-cells that vary with respect to their function: cytotoxic T-cells (TC-cells) – responsible for cell-mediated immunity helper Tcells (TH-cells) – stimulate T-cell and B-cell response suppressor T-cells (TScells) – moderators of T- and B-cell activity Cytotoxic T-cells (TC cells) TC-cells contain CD8 receptors to recognize foreign antigen fragments (remnants of invasion), displayed on MHC-I containing cells, as infected or cancerous and kill the cells to prevent replication (doesn’t sound very fair, but I suppose you can’t be too careful in protecting against double-agents). Link to Cytotoxic T-cell movie: http://www.cellsalive.com/ctl.htm Link to Cytotoxic T-cell killing http://www.bio.davidson.edu/courses/movies.html its target: Helper T-cells (TH cells) TH-cells are also referred to as T4-cells because they present CD4 on their cell surface. T4-cells recognize foreign antigen fragments displayed on MHC-II containing cells and secrete cytokines to improve immune response. T4-cells are essential for activation of B-cells, additional T-cells, natural killer cells, and macrophages in response to bacterial, viral, parasitic or fungal invasion. T4-cells also bind to B-cells and promote their differentiation into plasma cells and memory cells. There are two subpopulations of TH-cells – TH1 and TH2. CD4 is the receptor for the human immunodeficiency virus (HIV) associated with AIDS. ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 21 Link to Helper T-cell message interpretation: http://www.hhmi.org/biointeractive/animations/tcell/tcell_frames.htm Suppressor T-cells (TS cells) TS-cells act as moderators (United Nations) and inhibit T-cell and B-cell activity when it is excessive. Link to T-cell http://www.bio.davidson.edu/Courses/immunology/Flash/Main.html selection: Immune regulation T-cells act as regulators of the immune system attacking cells that are malignant or defective, stimulating T-cell and B-cell activation, killing foreign pathogens or infected cells, and even suppressing the immune response. Inactive T-cells have receptors that recognize antigens bound to MHC proteins on the surface of citizen cells of the homeland (remnants of infection or abnormal processes). T-cell receptors are protein complexes that bind to MHC-antigen complexes on citizen cells displaying abnormal antigen fragments. T-cells are activated when antigen fragments bind to T-cell receptors. Like antibodies, T-cell receptors are specific for only one antigen and are capable of distinguishing self from non-self. Once antigen attachment has taken place, that cell becomes specific for that antigen and ultimately results in production of clone cells that are also specific for that antigen. As mentioned previously, CD antigens (markers) are uniquely expressed on the surface of all lymphocytes, and serve as biochemical markers characteristic for a particular cell type indicating the lineage or stage of maturity. All T-cells have CD3 receptor complexes and various other CD antigens. CD8 (CD+8) antigens are found on TC-cells and TS-cells. CD8-cells respond to antigens displayed on Class I MHC proteins. CD4 (CD+4) antigens are found on TH-cells, and respond to antigens displayed on MHC II proteins. CD4 and CD8 markers are bound to the CD3 complex on the T-cell surface. Activation does not usually occur until the T-cell encounters and recognizes (binds) a second antigen of the same type. The “double-signature” is a double-check before destruction. CD8 cell activation There are two types of CD8 cells – one type results in rapid response stimulating large numbers of TC-cells (killer T-cells) and memory T-cells. Once activated, TC-cells seek and destroy cells containing the antigen they are specific for. A variety of weaponry is used by TC-cells against invaders. Chemical agents such as perforin are released, a poisonous chemical known as lymphotoxin is ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 22 secreted, or programmed cell death is activated – a process known as apoptosis (cell suicide). Memory T-cells immediately differentiate to TC-cells resulting in a swift cytotoxic response. The second type results in a slower response and results in production of small numbers of suppressor T-cells (TS-cells). TS-cells produce inhibitory cytokines for T-cells and B-cells. TS-cells are slow to respond and act only after the initial immune response. CD4 cell activation CD4 cells divide to produce TH-cells and memory TH-cells. CD4 markers are found on TH-cells. CD4 stimulates a variety of cytokines that stimulate T-cell division to produce memory T-cells and accelerate TC-cell maturity, attracts macrophages, attracts and stimulates NK cell activity, and promotes B-cell activation. Natural killer cells (NK cells) Natural killer cells perform immunological surveillance of body tissues. NK-cells are extremely versatile lymphocytes that can attack virus-infected cells and cancer cells in interstitial fluids. NK cells respond immediately to contact with any abnormal antigens. NK cells perform “silent hits” by attaching to cells containing abnormal antigens, lining up a secretory apparatus (Golgi apparatus) in the cytoplasm of the NK cell and releasing a chemical (perforin) that creates holes in the membrane of the target cell. Link to animation – NK cell bound to target cell – Be patient, it takes a few minutes for the video to load, but its worth the wait!: http://www.hybridmedicalanimation.com/pages/jjani_pc/NK_ani_pc.html Chemical communication system Small proteins known as interferons are released by activated lymphocytes, activated macrophages, and virus-infected tissue. Interferons stimulate more macrophages and NK-cells, and bind to cell surface receptors of virus-infected cells triggering production of antiviral proteins in the cytoplasm of the target cell that interfere with viral replication. There are three types of interferon: alpha-interferon (-interferon) – attracts and stimulates NK cells beta-interferon (- interferon) – slows inflammation in damaged areas gamma-interferon (-interferon) – secreted by T-cells and NK cells – stimulate macrophage activity ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 23 Most cells other than lymphocytes and macrophages secrete beta-interferon in response to viral infection. Complement system The complement system consists of 11 special proteins (designated C1-C11) that complement the action of antibodies. The complement system has two different pathways – classical and alternative. The classical system is the more rapid of the two pathways. Classical pathway Think about a team of navy seals executing manoeuvres to plant charges on the hull of a marked enemy ship. C1 is a bit like those seals; it binds to antibody that is bound to antigen (antigen-antibody [Ag-Ab] complex) on the target cell surface. The Ag-Ab complex catalyzes a series of chemical reactions that ends with the inactive C3 converting to the active form, C3b, which then binds to the surface of the target antigen. Once bound, C3b stimulates phagocytosis and promotes inflammation. C3b also triggers reactions that lead to the creation of a membrane attack complex (MAC) that creates pores in the membrane of the target cell, like holes blown in the hull of a ship. Alternative pathway When the target is not marked (no Ag-Ab complex), the navy divers do not know where the enemy ship is, so other techniques (alternate pathway) are used to detect and mark the location of enemy ships. The alternative pathway uses communication satellites (complement proteins) suspended in the plasma that become activated on contact with foreign materials. The activated proteins catalyze a series of reactions that result in conversion of C3 to C3b, stimulation of phagocytosis, and formation of membrane attack complex (navy seals). Proteins of the alternative pathway interact in the plasma in response to contact with bacteria, certain parasites and virus-infected cells. However, the alternate pathway results in an overall slower response, because the alternate pathway functions to trigger the classical pathway, which then destroys the target. In addition to destroying foreign invaders, complement causes degranulation of mast cells, and formation of the membrane attack complex – a group of lipidsoluble proteins that punch holes in the cell membrane of pathogens. Inflammation Inflammation involves a localized heat, redness, swelling, and pain in response to a break in one of the physical body barriers (skin, mucous membranes lining the eyes, nose, mouth, respiratory tract, intestinal tract and genital tract). ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 24 Inflammation results in temporary repair of the injury; prevention of additional microorganisms and foreign substances from entering the body; inhibition of invasion; and mobilization of body defences (emergency responders, police forces and possibly military personnel). Link to Splinter - http://www.cellsalive.com/ouch1.htm Degranulation of mast cells and basophils results in the release of histamine, which initiates the inflammatory response. Histamine is one of a number of chemical messengers (cytokines) involved in immune response. Other cytokines include interleukins, interferons, tumor necrosis factors, chemicals that regulate phagocytic activity, and colony-stimulating factors that stimulate blood cell production in bone marrow and lymph tissues. Histamine attracts more leukocytes to the area, and opens pores in capillaries to allow plasma proteins and fluid to pass into the interstitial space causing edema. Histamine also dilates blood vessels increasing blood flow to the area. The result is inflammation. Fever Fever results from the action of pyrogens that are stimulated by microorganisms and bacterial toxins. Ag-Ab complexes can also act as pyrogens and can stimulate pyrogen production by macrophages (interleukin-1). Fever increases body metabolism resulting in increased rates of immune cell activity, and inhibits certain viruses and bacteria. Acquired Immunity (Specific defences) Specific defence forms the special-forces known as acquired or adaptive immunity. There are two types of acquired immunity – active and passive. Specific immunity is conferred by cell-mediated forces provided by two types of lymphocytes – cytotoxic T-cells and helper T-cells, and humoral or antigenspecific forces provided by another type of lymphocytes called B-cells (navy/airforce). The initial immune response takes 7-10 days to develop, and typically lasts a few weeks before taking leave following the battle. Memory T- and B-cells are left behind – surveillance forces – trained to recognize the invader if it is encountered again. Memory cells result in a swift strong response (within 1-2 days of antigen re-exposure) should the invader ever attempt to penetrate “the system” again in the future. These cells do not respond to invasion by nations (antigens) other than the one previously fought. Surveillance for new invaders is provided by NK- cells and phagocytes that routinely patrol for suspicious activity and invasion by foreign antigens. ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 25 Active immunity Active immunity is immunity that results from previous exposure to a microorganism or foreign antigen. There are two types of active immunity – acquired and induced. Active acquired immunity Active acquired immunity results in production of antibodies in response to foreign and abnormal antigens. Active immunity can be acquired naturally through infection or induced. Active acquired immunity could be compared to notoriety due to accumulated minor infractions (invasions) that together result in strong antibody response in the future. Induced active acquired immunity Induced active acquired immunity is obtained by administering vaccine – a process known as immunization. Vaccine is a preparation containing a dead or inactive micro-organism, or antigens from it. The body responds to the administration of vaccine by producing antibodies against the antigens of the micro-organism. Passive immunity Passive immunity is short-term immunity that is acquired from antibodies made by another animal - transfer of antibodies from mother to fetus or immunoglobulin shots like the ones used as prophylactic treatment following blood or body fluid exposure As with active immunity, there are two types of passive immunity – natural and induced. Natural passive immunity results from transfer of maternal antibodies across the placenta or through breast milk. Induced passive immunity results from administration of antibodies produced by another individual or animal. The antibodies provide short-term assistance in fighting infection. Properties of immunity specificity – antibody production against one particular antigen – equivalent human personality trait: attention to detail versatility – ability to respond effectively to different stimuli – equivalent human personality trait: ability to adapt to change memory – excellent memory required to recognize and initiate a rapid, strong and long (or prolonged) response on subsequent exposure to a particular antigen – equivalent human personality trait: long-term memory ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 26 (remembering what happened from birth when someone recalls a situation) tolerance – not overly sensitive to stimulants so that “self” antigens are not attacked – equivalent human personality trait: positive self-image Antibodies Foreign and abnormal antigens trigger lymphocyte production and stimulate lymphocytes to produce antibodies in response. Once an invader has been recognized, more antibodies are made to attack and neutralize it. When antibodies identify antigens, phagocytes engulf and neutralize or disassemble them. There are more than 1,000,000 different types of antibodies performing surveillance for invading foreign antigens that enter the body. Antibodies circulating in the bloodstream bind to antigens that they recognize and attack it. Antibodies are Y-shaped proteins with two arms that act as antigen-binding sites and a base that determines the class of antibody as described below. Antibodies are also referred to as gamma-globulins or immunoglobulins. Immunoglobulins, and are named according to their functions – agglutinins, precipitins, hemolysins, etc. Animation – Antibody production from: http://www.wellesley.edu/Biology/Concepts/ncwebpage/immunicyto.html Created in 2003 by Giuliana Funkhouser and Cristina Greavu for CarolAnn Paul of the Wellesley College Biology Dept., under the auspices of the Betsy Wood Knapp Technology Intern Program at Wellesley College. The base of the Y is made of heavy chains, while its arms are made of both light and heavy chains. The tips of the arms contain a cavity with a shape unique for the shape of the protein fragment (antigen) that the antibody is specific for. Immunoglobulins There are five general classes of immunoglobulins: IgG - account for 75% of plasma antibody produced in secondary immune response - capable of crossing the placental membrane from mother to fetus IgA - found in secretions such as saliva, tears, intestinal and bronchial mucus, as well as breast milk - disable invaders ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 27 IgE - allergic responses - IgE/antigen complex stimulates mast cells to release histamine IgM - activates complement - reacts to blood group antigens IgD - found on surface of B-lymphocytes - role unclear Response to invasion Bacterial infection When body surface barriers fail and bacteria reach the extracellular fluid, an inflammatory response develops as immune cells defend the body against further penetration and invasion. A series of events occurs: 1. phagocytes and NK-cells migrate to the area in response to chemical messages (cytokines) sent by emergency responders at site of invasion, and ingest and/or destroy bacteria 2. TC-cells appear as T-cells are activated by antigen presentation 3. plasma-cell production increases as activated B-cells differentiate 4. surge in plasma cell production is followed by gradual decrease and sustained levels of circulating antibodies 5. complement system activated by components of bacterial cell wall complement causes degranulation of mast cells and basophils, followed by cytokine release, which attracts more immune cells, dilates blood vessels and increases capillary permeability – increased blood flow to the area results in inflammation, and plasma proteins and water passing into the interstitial spaces results in edema 6. membrane-attack-complex (MAC) molecules blow holes in the bacterial cell wall resulting in plasma influx resulting in lysis and death (navy divers plant charges on hull of ship ultimately sinking the ship) 7. macrophages ingest bacteria opsonization of encapsulated bacteria acquired immune response – antibodies already present act as opsonins and also inactivate bacterial toxins 8. memory B-cells attracted to infection site activated by antigens that they recognize (police line-up) if blood vessels are also damaged, platelets and coagulation proteins help reduce damage ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 28 Viral infections The initial steps in response to viral invasion are different from those involved in bacterial invasion. Phagocytes digest and disassemble viruses and display viral antigen fragments on MHC proteins on the cell surface activating TC-cells and NK-cells. In addition to activation by antigen presenting phagocytes, TC-cells and NK-cells are activated by contact with antigen-presenting phagocytes or virus infected tissue cells. Viruses bind to cell membranes in the body and cross the cell membrane by binding to membrane receptors and triggering endocytosis, a process similar to phagocytosis, except that the cell membrane indents rather than pushing out around the particle to be ingested. Alternatively, the viral envelope fuses with the cell membrane, injecting the virus core into the cytoplasm. Once inside the cell, the virus uses the cell’s resources to replicate – create new viral nucleic acid and viral proteins, which then assemble to new virus particles that are released and subsequently infect new cells. In the process, host cell function may be disrupted resulting in cell death, or may be temporarily disrupted by viruses which reproduce only sporadically (e.g. Herpes simplex type 1). Other viruses (e.g. HIV) incorporate viral DNA into host cell DNA and reproduce. Viruses are released through cell rupture or they cloak themselves in a capsule of host membrane and escape through the surface unnoticed. Immune Response to Viral Infection Innate immune response and antibodies are involved in defence against acute viral infection. However, once viral particles enter host cells, TC-cells form the main line of defence, searching for infected host cells and destroying them (hitmen locating and killing off traitors). Antibodies play an important role in acute viral infection: - act as opsonins and coat the viral particle to enhance their visibility to macrophages - bind to virus to prevent entry into cells - macrophages ingest viruses and insert fragments in cell membrane bound to MHC molecules and produce cytokines – cytokines initiate the inflammatory response; one of these, interferon, causes host cells to make antiviral proteins that prevent viral replication - TH-cells bind to viral antigen fragments on macrophages and enhance immune cell response - TC-cells recognize viral antigen fragments bound to MHC complexes and induce the cell to commit suicide (apoptosis). ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 29 Diagnostic tests The immune system is one of the most difficult systems to understand, because of its complexity. The easiest way to evaluate the function of various cells of the immune system is by drawing blood from the arm. Other tests are also performed to observe possible complications related to the virus and most importantly to observe possible toxicities (adverse affects) of medications being studied. These tests, referred to as safety bloods (labs), include a CBC/differential, full chemistries and a urinalysis. The CBC consists of the white blood cell count, differential, hemoglobin, hematocrit and platelet count. The differential is the percent of the various types of white cells; lymphocytes, granulocytes, and several others. The full chemistries look at the functioning of the liver, kidneys, heart and many other important functions of the body. The urinalysis also helps determine the function of the kidneys. There is some overlap of safety bloods and immune function studies as may be noted. Immune Function Studies White Blood Cells (WBCs): White blood cells play a major role in defending the body against infections and foreign invaders such as bacteria, fungi, viruses and parasites. There are five types of white blood cells: granulocytes (also known as neutrophils), lymphocytes (lymphs), monocytes, eosinophils and basophils. Normal Value: 3300-9600/mm3 Polymorphonuclear granulocytes (polys): Polymorphonuclear granulocytes are commonly referred to as polys, segs, neutrophils or grans. Mature white blood cells are referred as polymorphonuclear granulocytes, while bands are less mature polys. Neutrophils, both polys and bands, are scavenger cells and are the first immune cells to arrive at a site of infection or injury. When the total neutrophil count (polys + bands) drops to less than 1000/mm3, there is an increased risk for bacterial and certain fungal infections, and severe risk when less than 500/ mm3. Normal Value: 40-78% of WBC or 1200-7800/ mm3. ARO Training & Consulting Bloodborne Pathogens Module 3: Defence – The Immune System at work Page 30 Lymphocytes (Lymphs): Lymphocytes specifically identify foreign substances as being "non-self" or mutant (defective) cells and cause their destruction and elimination preventing cell replication. There are two major classes of lymphocytes, B-lymphocytes and T-lymphocytes, as well as the natural killer cells that fall under the classification of lymphocytes. Normal Value: 14-49% of WBC or 420-4900/mm3. Cell Type Total lymphocytes Total T cells CD4 cells CD8 cells Total B cells NK cells Proportion of total ~ 30% of total WBC count ~ 70% of total lymphocyte count ~ 50% of total T-cell count ~ 20% of total T-cell count ~ 10-15% of total lymphocyte count ~ 10-15% of total lymphocyte count Reference: Hayglass, K. 2003. Immunology Notes – Medical Physiology. Retrieved from http://www.umanitoba.ca/faculties/medicine/units/immunology/medphys.htm on August 4, 2004. B Lymphocytes B cells are programmed to produce immunoglobulins. Each B-cell produces a specific antibody for a specific foreign antigen. Antigen/antibody complexes render the antigen harmless and mark them for destruction. Normal values: 50-250 cells/mL T Lymphocytes Normal values: 600-2,400 cells/mL Normal Values of Immunoglobulins: IgG: 650-1600 mg/dl IgM: 50-320 mg/dl IgA: 65-415 mg/dl