Residency Redesign in Internal Medicine: Summary
advertisement
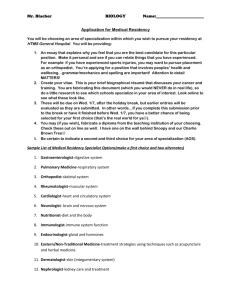
Residency Redesign in Internal Medicine: Summary The Internal Medicine community has just published three articles that consider problems with Internal Medicine residency training and suggest solutions. The articles represent the views of The Society of General Internal Medicine (SGIM; Holmboe ES, Bowen JL, Green M et al. Reforming Internal Medicine Training. J Gen Intern Med 2005; 20:1165– 1172.), the Association of Program Directors in Internal Medicine (APDIM; Fitzgibbons JP, Bordley DR, Berkowitz LR et al. Redesigning resident education in Internal Medicine: a position paper from the Association of Program Directors in Internal Medicine. Ann Intern Med. 2006;144:920-926) and the American College of Physicians (ACP; Weinberger SE, Smith LG, Collier, VU Ann Intern Med. 2006;144:927-932). They note with concern a declining interest in general internal medicine and speculate that an important reason is the character of residency training. They observe that continued emphasis on inpatient medicine is outmoded. The long lengths of stay that once made the inpatient setting attractive for learning are no more; most primary and subspecialty care is ambulatory. Although the organizations suggest more block ambulatory experience, they acknowledge that the quality of resident ambulatory experiences is often unsatisfactory, with dysfunctional clinics caring for exceptionally complex patients. They note the lack of a core curriculum of knowledge, skills and attitudes and the lack of specification as to the level of competence required for specific elements of a curriculum. All express the conviction that high-quality training must be linked to high-quality patient care in an environment that emphasizes clinical quality awareness and improvement, and patient safety. They emphasize the need for close, graded supervision of residents and better assessment of performance. They suggest specific instruction in quality of care and patient safety, health disparities, cultural sensitivity, professionalism and lifelong learning. They comment on the importance of multidisciplinary teams and the need for resident experience with such teams. They support continuation of a three-year residency. The ACP and APDIM recommend two years of “core” training with the third year tailored to the goals of the individual. The ACP and SGIM note the need for reconsideration of medical school curriculum. The SGIM remarks on the need to consider alternatives to current certification practices. All ask for assignment of residents only on the basis of educational need. The APDIM acknowledges that this carries the risks that residents may become peripheral and therefore expendable and that they may become more observers than participants. Finally, they ask for reforms in promotion, rewards and professional development for teaching faculty and for reforms in the funding of graduate medical education. The culture and history of Internal Medicine and Pediatrics residency training are not identical, but they have much in common. The thoughts, representing many hours of research and discussion, in these documents are valuable and instructive for the R3P project.