Poorly Differentiated Thyroid Carcinoma

2
Historic Background
In order to answer the question posed in the title of my presentation, I would like first to briefly review the concept of poorly differentiated thyroid carcinoma with a follicular phenotype.
The concept of poorly differentiated thyroid carcinoma began to emerge in 1983 when Sakamoto et al (1) analyzed 258 malignant thyroid neoplasms and on the basis of solid, trabecular and scirrhous patterns, were able to segregate a group of carcinomas that they interpreted as poorly differentiated. Surprisingly, the cytologic features of these poorly differentiated carcinomas were not described. However, the tall cell variant of papillary carcinoma and papillary thyroid carcinomas with stromal sclerosis were illustrated and included in the poorly differentiated group. The authors emphasized that the prognosis of these poorly differentiated thyroid carcinomas was worse than that of well differentiated thyroid carcinomas, and therefore, their separation was fully justified.
Hawk and Hazard (2) first described the tall cell variant of papillary thyroid carcinoma as having an aggressive clinical course and as being microscopically characterized by tall cells (cell height at least twice the width) with abundant oxyphilic cytoplasm that formed papillae. Because of its aggressive clinical behavior and the fact that this variant often has a prominent trabecular pattern, some pathologists have included it in the poorly differentiated category. However, the nuclear features and thyroglobulin immunoreactivity of the tall cell variant are similar to those of conventional papillary thyroid carcinoma. (3) In fact, the only difference between the tall cell variant and conventional papillary carcinoma is cell height. Moreover, the clinical course appears to
3 best correlate with stage of disease, especially extrathyroidal extension rather than histology alone.
In 1984 Carcangiu et al (4) recognized a distinctive form of thyroid carcinoma associated with a poor prognosis and with a characteristic insular pattern that was regarded as poorly differentiated. According to the authors, this unusual form of thyroid carcinoma was originally described by Langhans in 1907. In addition to the insular pattern, the tumor often showed follicles, and trabecular and sheet-like growth patterns.
Many of the neoplastic cells had nuclear features that were similar to those of papillary carcinoma while others exhibited nuclear features that were similar to those of follicular carcinoma. All tumors showed variable thyroglobulin reactivity. The biologic behavior of these insular tumors was thought to occupy an intermediate position between the well differentiated papillary and follicular carcinomas and undifferentiated or anaplastic carcinomas. Eight of the 25 patients reported by Carcangiu, et al had either lymph node or skeletal metastases at presentation. The overall death rate for patients 50 years of age or older was 55.5%.
Soon after the columnar cell variant of papillary thyroid carcinoma was described by Evans (5) in 1986 as an aggressive neoplasm, Sobrinho-Simoes et al (6) expressed the opinion that this tumor fell into the category of poorly differentiated thyroid carcinoma.
Microscopically, the columnar cell variant shares the follicular, papillary, trabecular, solid and cribriform patterns described in other forms of poorly differentiated carcinomas. Moreover, the columnar cells, which show prominent pseudostratification, infrequently exhibit the large clear nuclei with grooves and pseudoinclusions that are characteristic of conventional papillary carcinoma. The thyroglobulin immunoreactivity
4 varies considerably from tumor to tumor and even in different areas of the same tumor.
A few tumors are, in fact, thyroblobulin negative. Originally thought to be an aggressive form of papillary carcinoma, its prognosis correlates best with clinical stage and the presence of extrathyroidal extension appears to be the single most important prognostic parameter. (7) Columnar cell variants of papillary carcinoma that are encapsulated or confined to the thyroid behave as conventional papillary carcinomas.
Papotti et al (8) in 1993 collected 63 examples of thyroid carcinomas considered to be poorly differentiated and characterized by insular, trabecular, solid and/or follicular patterns. Because they demonstrated paranuclear thyroglobulin deposits in the neoplastic cells these were compared to the primordial cells of the developing fetal thyroid. In our experience, however, paranuclear thyroglobulin deposits or “inclusions” can also be seen in both adenomas and well differentiated follicular carcinomas (9).
In 1994, our group studied 41 thyroid carcinomas that had an insular component
(10). We have now examined 11 additional cases and have expanded our original observations related to these carcinomas. Based on nuclear features and growth patterns, we classified these tumors as follicular carcinomas or as follicular variants of papillary carcinomas. (figs.1-6). In most tumors, the cells lining the follicles were similar to those arranged in nests, trabecular and cribriform structures. Cells with clear nuclei, grooves, and pseudoinclusions were identified in the papillary carcinomas, whereas, cells with round or oval nuclei having granular chromatin were recognized in the follicular carcinomas. (figs.2-6). Occasionally, however, papillary carcinomas had cells with nuclei which were less clear or even hyperchromatic and similar to those of follicular carcinoma. The insular pattern predominated in most tumors and was focal in others.
5
Achitecturally and cytologically, the tumors were heterogeneous. A variable proportion of trabecular, solid and, occasionally, cribriform structures were also indentified. (figs.7-
8). A predominance of clear cells was recognized in three tumors and collections of oncoytic cells were seen in another. (fig. 9). Abundant extracellular alcian blue positive mucin was seen in two tumors. The majority of carcinomas (57%) with insular, trabecular and cribriform patterns showed diffuse immunoreactivity for thyroglobulin.(Figs. 10-12). We have now seen a conventional papillary carcinoma, rich in clear cells, in which, the metastases had predominantly trabecular, solid and insular growth patterns but the population of clear cells was similar to that of the primary tumor.
We have also seen the opposite situation, that is, a papillary carcinoma with trabecular, solid and insular growth patterns that metastasized as a conventional papillary carcinoma.
None of the 41 patients we reported had distant metastases at presentation and the overall mortality rate was 9.4%. In our series, the biologic behavior of these tumors appeared to correlate with stage of disease rather than with the presence of an insular growth pattern. Other authors, however, have found that the insular component is an independent risk factor in thyroid carcinomas. (11) Likewise, the extent of the insular pattern appears to correlate with prognosis. A focal insular pattern in an otherwise conventional papillary or follicular carcinoma does not alter prognosis. (12)
In 1999, Nishida et al (13) reported 302 thyroid carcinomas of which 102 (33.7%) were interpreted as poorly differentiated. Included in the poorly differentiated group were carcinomas with solid, trabecular or scirrhous patterns as well as insular carcinomas, columnar cell carcinomas and tall cell carcinomas. This heterogeneous group classified as poorly differentiated thyroid carcinomas were subdivided into focal-
6 poorly differentiated (<10% of poorly differentiated component) and diffuse-poorly differentiated. (> 10% of poorly differentiated component). The authors concluded that the diffuse poorly differentiated thyroid carcinoma was associated with a poor prognosis and, therefore, was an important clinicopathological entity. (13) It is unjustified to include the focal tall cell or columnar cell variants of papillary carcinoma in the poorly differentiated carcinoma category because the definition of those tumors do not fulfill the established morphologic criteria for the tall cell and the columnar cell variants of papillary carcinomas.
We recently described a rare but distinctive form of thyroid neoplasm that we believe fullfilled the morphologic criteria for poorly differentiated carcinoma. It was characterized by nodular, trabecular and sheet-like growth patterns and a small number of follicles (5% of the tumor), (figs.13-14). The neoplastic cells had large vesicular nuclei with prominent nucleoli. In addition, 10 to 30% of the neoplastic cells had rhabdoid inclusions (14) (Fig.15). Focal immunoreactivity for thyroglobulin was detected in about 20% of cells. We have now seen two additional neoplasms with similar features except for the rhabdoid inclusions.
Discussion
Under the category of poorly differentiated thyroid carcinoma a variety of malignant thyroid neoplasms have been described. The morphologic criteria employed to define poorly differentiated thyroid carcinoma in most publications have been trabecular, solid, insular, cribriform and scirrhous growth patterns. These growth patterns, however, lack specificity and can be seen in hyperplastic lesions and benign thyroid tumors. For
7 example, insular, trabecular, nodular and solid patterns have long been recognized in dyshormonogenetic goiters as, well as in sporadic and endemic adenomatous goiters. (15)
Likewise, trabecular, solid and insular patterns are characteristic features of some thyroid adenomas. (16, 17) On the other hand, oncocytic (Hürthle cell) carcinoma, which is regarded as a form of follicular carcinoma, often shows trabecular, solid, nodular and nesting patterns, and yet, the term poorly differentiated carcinoma is not employed for this tumor probably because their characteristic cytologic features are the same in both the follicular and non-follicular areas. (17) Thyroid carcinomas that occur in patients with familial adenomatous polyposis coli characteristically show focal papillary architecture, cribriform features, solid, trabecular and spindle cell areas as well as squamoid morules. Moreover, these tumors express only focal thyroglobulin reactivity yet they are not included in the poorly differentiated category. They are considered to be variants of papillary carcinoma with atypical histology. (18, 19) In one study poorly differentiated thyroid carcinomas were identified on the bases of cytologic atypia, mitotic activity and necrosis (20); features which do not reflect cell differentiation, especially in endocrine tumors.
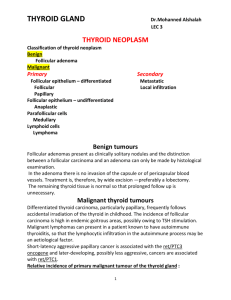
With minimal variations, the cytologic features of the vast majority of “poorly differentiated carcinomas” are similar to or overlap with those of the conventional varieties of papillary or follicular thyroid carcinomas including the expression of thyroglobulin and TTF-1. As a result of the inconsistencies in the definition of poorly differentiated thyroid carcinoma and the inclusion of several different types of carcinoma in the poorly differentiated category, the term poorly differentiated carcinoma has led to considerable confusion and remains controversial.
8
An important clinical feature that has justified the attempts to characterize poorly differentiated thyroid carcinoma as a distinct entity is its aggressive clinical course. It is unclear however, whether the aggressive clinical course of these tumors correlates with their morphologic features or with other well established prognostic factors such as gender, age, size of the tumor, extrathyroidal extension and distant metastases (21-24). A large series from the AFIP has shown that minimally invasive follicular carcinomas, regardless of their growth patterns (with or without trabecular, insular or solid patterns), are very low grade malignant tumors that rarely recur and seldom metastasize (23). The death rate in this series was less than 1%. We have now seen four minimally invasive follicular carcinomas with predominant insular growth patterns that have not metastasized despite long term follow-up (mean follow-up 9 years).
There have been numerous immunohistochemical and molecular pathology studies on poorly differentiated thyroid carcinoma that have had conflicting results. The use of different morphologic criteria and the inclusion of different types of carcinomas such as the columnar and the tall cell variants in the poorly differentiated group makes it difficult to compare results and to reach valid and definitive conclusions. It is unlikely that a single, or a panel of immunohistochemical or molecular markers will allow a distinction between well and poorly differentiated thyroid carcinomas since the latter tumors have not been well defined (21,25). Immunohistochemical markers such as high molecular weight cytokeratins, HBME-1, galectin-3, CD44v6, p53,PAX8-PPARﻻ1 and
Bcl-2 do not reliably distinguish well differentiated from poorly differentiated follicular and papillary carcinomas. Likewise, the molecular abnormalities described in anaplastic or poorly differentiated follicular and papillary carcinomas can also be detected in well
9 differentiated thyroid carcinomas with follicular phenotype. (26-29) However, with the use of DNA microarray technologies, the discovery of new markers might help surgical pathologists clarify the controversial issue of poorly differentiated thyroid carcinoma.
(30)
We would like to emphasize that an aggressive clinical course does not justify the inclusion of a carcinoma in a poorly differentiated category. Clinical behavior is not necessarily related to cell differentiation. In fact, cell differentiation is a complex biological phenomenon related to gene expression and other factors. The actin cytoskeleton which participates in locomotion also maintains cell morphology. Several cell to cell adhesion molecules are involved in cell differentiation and molecules involved in cell interaction with the extracellular matrix also play a role in cell differentiation. (31)
The demonstration that conventional papillary carcinoma can develop metastases that grow predominantly in trabecular and insular patterns and, viceversa, that a primary papillary carcinoma that shows predominantly insular and trabecular patterns can develop metastases that grow as conventional papillary carcinoma, suggests that the microenviroment may play a role in the development of these growth patterns.
The vast majority of thyroid carcinomas considered to be poorly differentiated have not been well defined and are, in fact, differentiated follicular or papillary carcinomas with unusual growth patterns. Currently, there is agreement that the tall and the columnar cell thyroid carcinomas are variants of papillary carcinoma rather than forms of poorly differentiated carcinomas. (17) When insular and trabecular patterns are present in follicular or papillary carcinomas, we recommend the inclusion of the patterns in the surgical pathology report because, in some series, they have been associated with
10 an aggressive clinical course. The terms follicular or papillary carcinoma with predominantly or focal insular growth patterns can be employed for these tumors.
In our opinion, the ideal definition of poorly differentiated thyroid carcinoma must include cell morphology, cell function measured by thyroblobulin reactivity and growth patterns. The neoplastic cells should be morphologically different from those of differentiated papillary or follicular carcinomas as well as anaplastic carcinomas. Few follicles should be present (<20% of the tumor) and only focal thyroglobulin immunoreactivity should be demonstrated in the tumor (<20% of the tumor). Defined as such, poorly differentiated thyroid carcinoma becomes an exceedingly rare neoplasm.
We believe, however, that more data are needed to reach a concensus and to clearly define this controversial tumor. Once the tumor is defined it might be possible to set the threshold between well differentiated and poorly differentiated follicular carcinoma of the thyroid.
Poorly differentiated carcinomas are difficult to define and characterize not only in the thyroid but in all endocrine organs. For example, the term poorly differentiated has not been adopted for carcinomas that arise in the pituitary gland (32) parathyroid glands
(33) adrenal glands (34) and endocrine pancreas (35). Perhaps cytologic features and growth patterns are insufficient criteria to recognize the degree of cell differentiation in malignant neoplasms in these endocrine organs.
11
REFERENCES
1.
Sakamoto A, Kasai N, Sugano H. Poorly differentiated carcinoma of the thyroid.
A clinicopathologic entity for a high-risk group of papillary and follicular carcinomas. Cancer 52:1849-55, 1983.
2.
Hawk WA, Harzard JB. The many appearances of papillary carcinoma of the thyroid. Cleve Clin Q 43:207-16, 1976.
3.
Ostrowski ML, Merino MJ. Tall cell variant of papillary thyroid carcinoma:
A reassessment and immunohistochemical study with comparison to the usual type of papillary carcinoma of the thyroid. Am J Surg Pathol 20:964-74, 1996
4. Carcangiu ML, Zampi G, Rosai J. Poorly differentiated (“insular”) thyroid
carcinoma. A reinterpretation of Langhans’ “wuchernde struma”. Am J Surg
Pathol 8:655-68, 1984.
5.
Evans HL. Columnar-cell carcinoma of the thyroid. A report of two cases
of an aggressive variant of thyroid carcinoma. Am J Surg Pathol 85:77-80, 1986.
6.
Sobrinho-Simoes M, Nesland J, Johannessen J. Columnar-cell carcinoma.
Another variant of poorly differentiated carcinoma of the thyroid. Am J Clin
Pathol 89:264-7, 1988.
7.
Wening BM, Thompson LD, Adair CF, et al. Thyroid papillary carcinoma of columnar cell type: clinicopathologic study of 16 cases. Cancer 82:740-53, 1998.
8.
Papotti M, Micca B, Favero A, et at . Poorly differentiated thyroid carcinomas with primordial cell component. A group of aggressive lesions sharing insular, trabecular, and solid patterns. Am J Surg Pathol 17:291-301, 1993.
9.
Vardaman JC, Albores-Saavedra J. Cytoplasmic inclusions in thyroid neoplasms of follicular cell origin (abstract). Am J Clin Pathol 96:410, 1991.
10.
Ashfaq R, Vuitch F, Delgado R, Albores-Saavedra J. Papillary and follicular thyroid carcinomas with an insular component. Cancer 73:416-23, 1994.
12
11.
Sasaki A, Daa T, Kashima T, et al. Insular components as a risk factor of thyroid carcinoma. Pathol Int 46:939-46, 1996.
12.
Nishida T, Katayama S, Tsujimoto M, et al. Clinicopathologic significance of poorly differentiated thyroid carcinoma. Am J Surg Pathol 23:205-11, 1999.
13.
Albores-Saavedra J, Housini I, Vuitch F, et al. Macrofollicular variant of
papillary thyroid carcinoma with minor insular component. Cancer 80:1110-
1116, 1997.
14.
Albores-Saavedra J, Sharma S. Poorly differentiated follicular thyroid carcinoma
with rhabdoid phenotype: a clinicopathologic, immunohistochemical and electron
microscopic study of two cases Mod Pathol 14:98-104, 2001.
15.
Ghossein RA, Rosai J, Heffess C, Dyshormonogenetic goiter: a clinico-
pathologic study of 56 cases. Clin Res 8:238-292, 1997.
16.
Carney JA, Ryan J, Gollmen RR. Hyalinizing trabecular adenoma of the thyroid
gland. Am J Surg Pathol. 11:583-591, 1987.
17. Rosai J, Carcangiu ML, DeLellis RA. Tumors of the thyroid gland. Atlas of
tumor pathology. Series 3. Fascicle 5. Washington, DC: AFIP; 1992.
18. Harach HR, Williams GT, Williams ED. Familial adenomatous polyposis
associated thyroid carcinoma: a distinct type of follicular cell neoplasm. Histo-
pathol 25:549-556, 1994.
19.
Perrier ND, Van Heerden JA, Goellner JR et al. Thyroid cancer in patients with familial adenomatous polyposis World J Surg 22:738-743, 1998.
20.
Wreesmann VB, Ghossein RA, Patel S G, et al. Genome wide appraisal of thyroid cancer progression Am. J. Pathol. 161: 1549-1556, 2002.
21.
Akslen LA, Li Volsi VA. Poorly differentiated thyroid carcinoma-it is important
(letter). Am J Surg Pathol 24:310-3, 2000.
22.
Jorda M, Gonzalez-Campora, Mora J, et at. Prognostic factors in follicular carcinoma of the thyroid. Arch Pathol Lab Med 117:631-5, 1993.
23.
Thompson LDR, Wieneke JA, Paal E, et al. A clinicopathologic study of minimally invasive follicular carcinoma of the thyroid gland with a review of the
English literature. Cancer 91:505-524, 2001.
24.
Schmid KW, Tötsch M, Öfner D. et al. Minimally invasive follicular thyroid carcinoma: a clinicopathologic study. Curr Topics Pathol 91:37-43, 1997.
13
25.
Raphael SJ, The meanings of markers: Ancillary techniques in diagnosis of thyroid neoplasia. Endocrine Pathol. 13:301-311, 2002.
26.
Wiseman SM, Loree TR, Hicks WL, et al Anaplastic thyroid cancer evolved from papillary carcinoma Arch. Otolaryngol Head Neck Surg. 129:96-100, 2003.
27.
Takeuchi Y, Daa T, Kashima K, et al, Mutation of p53 in thyroid carcinoma with an insular component. Thyroid 9:377-381, 1999.
28.
Park KY, Koh JM, Kim Yl et al. Prevalences of G,
ras, p53 mutations and ret/PTC rearrangements in differentiated thyroid tumors in Korean population.
Clin. Endocrinol. 49:317-323, 1998.
29.
Fogelfeld L, Bauer TK, Schneider AB, et al. p53 gene mutations in radiationinduced thyroid cancer. J. Clin. Endocrinol. Metab. 81:3039-3044, 1996.
30.
Owens LV, Xu L, Yang X, et al. Focal adhesion kinase as a marker of invasive potential in differentiated human thyroid cancer. Ann Surg Oncol 3:100-105,
1996.
31.
Gubiner BM. Cell adhesion; the molecular basis of tissue architecture and mor-
phogensis. Cell 84;345-357, 1996.
32. Pernicone PJ, Scheithauer BW, Sebo TJ, et al. Pituitary carcinoma: a clini- copathologic study of 15 cases. Cancer 79;804-812, 1997.
33. Hundahl SA, Fleming ID, Gremgen AM, et al. Two hundred eighty-six cases of
parathyroid carcinoma treated in the US between 1985-1995. Cancer 86:538-
544, 1999.
34.Weiss LM, Madeiros LJ, Vickery AL, Pathologic features of prognostic
significance in adrenocortical carcinoma. Am J Surg Pathol 13:202-06, 1989.
35. Solcia E, Capella C, Klöppel G. Tumors of the pancreas. Atlas of tumor
pathology. Fascicle 20. Third series. Washington D.C. AFIP, 1997.
14