POORLY DIFFERENTIATED THYROID
advertisement

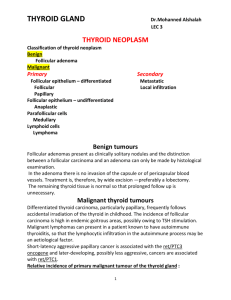
POORLY DIFFERENTIATED THYROID CARCINOMA: INTRODUCTION TO THE ISSUE, ITS LANDMARKS, AND CLINICAL IMPACT Juan Rosai, M.D. From the Department of Pathology, National Cancer Institute, Milan, Italy 1 In his book on Human Tumors, Pierre Masson lamented that "No classification is more difficult to establish than that of thyroid [carcinomas]. Their pleomorphism is almost the rule; very few are adapted to a precise classification" [1]. There are few issues that support this statement as strongly as those concerning the existence and definition of poorly differentiated thyroid carcinoma (PDTC). Since the idea was first proposed, some authors have enthusiastically endorsed it, others have grudgingly accepted it after some initial hesitation, and still others remain profoundly skeptical [2-6]. Since it would be ludicrous to think that these various positions are in any way influenced by other than scientific considerations, it is only those that we will address in this brief contribution. Let's start by saying that nobody who has seen a typical case of insular thyroid carcinoma will deny that the tumor has a distinctive appearance, almost to the point of instant pattern recognition, and that it would be inaccurate and misleading to designate such a tumor either as a follicular or papillary carcinoma without a qualifier, or as an undifferentiated (anaplastic) carcinoma. Alas, to provide a satisfactory definition of a poorly differentiated carcinoma has proved an almost insurmountable task. It reminds one of the famous crack about pornography to the effect that "I don't know how to define it, but I have no proplems in recognizing it when I see it". Much of the trouble concerning the identify of PDTC can be traced back to the original proposals. Independently and almost simultaneously, Carcangiu et al [7] and Sakamoto et al [8] proposed the concept using a similar terminology but widely disparate criteria. Carcangiu et al [7] described a tumor with a distinctive set of architectural and cytologic features, which included insular pattern of growth (hence the name), small cell size, round hyperchromatic nuclei, mitotic activity, and frequent necrosis. Sakamoto et al [8] based instead their proposal exclusively on the pattern of growth: tumors with a follicular or papillary pattern were regarded as well-differentiated (although the latter assumption can be challenged, since the normal thyroid does not make papillae), whereas tumors with a solid, trabecular, or sclerotic ("scirrhous") pattern of growth were categorized as poorly differentiated. It should obvious that the first proposal is an attempt at the description of a distinct "entity", whereas the latter is a grouping of a morphologically diverse group 2 of tumors on the basis of architectural similarities. In this context, the fact that Carcangiu et al [7] entitled their paper poorly differentiated ("insular") carcinoma was not particularly fortunate, since this could be taken to imply that the two terms are synonymous, when what was meant was that insular carcinoma was a type (one may say the prototypical expression) of a poorly differentiated carcinoma composed of follicular cells. Unfortunately, this dualistic approach has not only persisted but become accentuated in recent years. Whereas some authors restrict the term PDTC to tumors that fulfill to the original description of insular carcinoma (whether using that designation or others, such as primordial cell carcinoma) [9-11], others include not only insular carcinomas, but also any type of carcinoma with a predominantly solid/trabecular pattern of growth, as well as tumors that have been found to be more aggressive than the usual papillary or follicular carcinoma even if their morphology is, strickly speaking, not poorly differentiated (such as columnar cell carcinoma or mucoepidermoid carcinoma) [5, 12-15]. The quandary is obvious. Another criticism that has been raised is that the use of the term insular carcinoma implies the existence of a distinct tumor type for what may be instead a lesser differentiated form of one or another of the two major types of well-differentiated thyroid carcinoma, i.e., papillary and follicular [5]. According to this view, there is not a single PDTC (not even if one restricts the term to the prototypical insular carcinoma) but rather poorly differentiated forms of either papillary or follicular carcinoma. It should be noted that this position is not too different from that espoused in the article by Carcangiu et al [7], as graphically depicted by the diagram shown in Fig.1, which in its utter simplicity tells this story: (1) thyroid tumors of follicular cells show a wide range of differentiation, which tends to correlate with their degree of aggressiveness; (2) the two major types are papillary and follicular carcinoma, a distintion originally defined on morphologic grounds and now supported by molecular markers; (3) the differences among those two major types are obvious among the well-differentiated forms, but become increasingly blurred as the tumors become less differentiated, to disappear altogether in the undifferentiated forms. The corollary of this scheme is that there may 3 be well be two kinds of poorly differentiated carcinomas, but that the very fact that they are poorly differentiated matters much more than to the subtype they may belong. What practical messages emerge from these considerations, where one to accept their premises ? The first is that insular carcinoma is not to be equated with PDTC but rather regarded as one of its subsets. The second is that both typing and grading play an important role in the evaluation of thyroid tumors (as they do in several other classification systems, such as breast carcinoma and soft tissue sarcoma), and that there is nothing intrinsically wrong with combining them in a classification scheme on the basis of their relative clinical significance. The third and most important message – as usual – is the realization that much still needs to be done. As above stated, the original description of insular and other types of PDTCs included a long list of morphologic features, both of architectural and cytologic type. When all of them are present in a given tumor, an aggressive behavior can be anticipated. But what if one or another of those features are missing, as is often the case? Are some of them prognostically more significant than others? Let's illustrate the point with some concrete examples: 1) Is a tumor with an insular pattern of growth but the nuclear features of papillary carcinoma more or less aggressive than a tumor showing a papillary configuration but composed of small, hyperchromatic, mitotically active nuclei? 2) Is it worse to have an architecturally and cytologically typical insular carcinoma that shows minimal or no invasion or a better differentiated tumor with widespread invasion? 3) What is the clinical significance of the presence of focal poorly differentiated features in a predominantly well-differentiated thyroid carcinoma? [16, 17] 4) What role will special techniques (read: molecular) play in this determination? In conclusion, it seems to me that the concept of PDTC has stood the test of time and proven its validity, at least on general grounds. For whatever it is worth, it has received the imprimatur of the 4 latest WHO Committee on Thyroid Tumors and has been incorporated into their classificaton scheme [18]. However, its definition remains blurred. It will be the task of the current generation of thyroid pathologists to put it in focus. PAPILLARY CARCINOMA POORLY DIFFERENTIATED CARCINOMA UNDIFFERENTIATED CARCINOMA FOLLICULAR CARCINOMA FIGURE 1 Position of poorly differentiated carcinoma in the scheme of thyroid carcinoma composed of follicular cells. 5 REFERENCES 1. Masson P. Human tumors. Histology, diagnosis and technique, 2nd Edition, Detroit, Wayne State University Press, p.589, 1970. 2. Akslen LA, LiVolsi V. Poorly differentiated thyroid carcinoma – it is important (letter to the editor). Am J Surg Pathol 24: 310, 2000. 3. Mizukami Y, Nonomura A, Michigishi T, Noguchi M, Ohmura K, Nakamura S, Hoso M. Poorly differentiated (“insular”) cacinoma of the thyroid. Pathol Int 45: 663-668, 1995. 4. Nishiyama RH. Another dissertation on poorly differentiated carcinoma. Is it really necessary? Adv Anat Pathol 6: 281-286, 1999. 5. Pilotti S, Collini P, Mariani L, Piacucci M, Bongarzone I, Vigneri P, Cipriani S, Falcetta F, Miceli R, Pierotti MA, Rilke F. Insular carcinoma: A distinct de novo entity among follicular carcinomas of the thyroid gland. Am J Surg Pathol 21: 1466-1473, 1997. 6. Sobrinho-Simoes M. Poorly differentiated carcinomas of the thyroid. Endocr Pathol 7: 99102, 1996. 7. Carcangiu ML, Zampi G, Rosai J. Poorly differentiated (“insular”) thyroid carcinoma: A reinterpretation of Langhans’ “Wuchernde struma”. Am J Surg Pathol 8: 655-668, 1984. 8. Sakamoto A, Kasai N, Sugano H. Poorly differentiated carcinoma of the thyroid. A clinicopathologic entity for a high-risk group of papillary and follicular carcinomas. Cancer 52: 1849-1855, 1983. 9. Decaussin M, Bernard MH, Adeleine P, Treilleux I, Peix JL, Pugest M, Tourniaire J, Berger N. Thyroid carcinomas with distant metastases: A review of 111 cases with emphasis on the prognostic significance of an insular component. Am J Surg Pathol 26: 1007-1015, 2002. 6 10. Papotti M, Botto Micca F, Favero A, Palestini N, Bussolati G. Poorly differentiated thyroid carcinomas with primordial cell component: A group of aggressive lesions sharing insular, trabecular, and solid pattern. Am J Surg Pathol 17: 291-301, 1993. 11. Pellegriti G, Giuffrida D, Scollo C, Vigneri R, Regalbuto C, Squatrito S, Belfiore A. Cancer 95: 2076-2085, 2002. 12. Mizumani Y, Nakajima H, Annen Y, Michigishi T, Nonomura A, Nakamura S. Mucinproducing poorly differentiated adenocarcinoma of the thyroid. A case report. Pathol Res Pract 189: 608-611, 1993. 13. Papotti M, Torchio B, Grassi L, Favero A, Bussolati G. Poorly differentiated oxyphilic (Hurthle cell) carcinomas of the thyroid. Am J Surg Pathol 20: 686-694, 1996. 14. Sobrinho-Simoes M, Nesland JM, Johannessen JV. Columnar-cell carcinoma; another variant of poorly differentiated carcinoma of the thyroid. Am J Clin Pathol 89: 264-267, 1988-89. 15. Sobrinho-Simoes M, Sambade C, Fonseca E, Soares P. Poorly differentiated carcinomas of the thyroid gland: A review of the clinicopathologic features of a series of 28 cases of a heterogeneous, clinically aggressive group of thyroid tumors. Int J Surg Pathol 10: 123-132, 2002. 16. Ashfag R, Vutch F, Delgado R, Albores-Saavedra J. Papillary and follicular thyroid carcinomas with an insular component. Cancer 73: 416-423, 1994. 17. Sasaki A, Daa T, Kashima K, Yokoyama S, Nakayama I, Noguchi S. Insular component as a risk factor of thyroid carcinoma. Pathol Int 46: 939-946, 1995. 18. Tumors of endocrine organs. Pathology and Genetics, World Health Organization Classification of Tumours, Lyon, 2004 (in press). 7