Word Doc 103 KB - Endocrine Pathology Society
advertisement

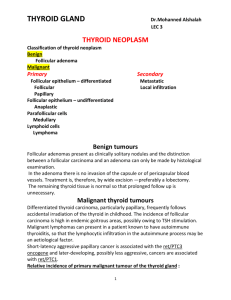
PROGNOSTIC FACTORS OF CLINICAL INTEREST IN POORLY DIFFERENTIATED CARCINOMAS OF THE THYROID. Mauro Papotti, Marco Volante – University of Turin Background. The term “poorly differentiated (PD) carcinoma” has been proposed twenty years ago to define non-follicular, non-papillary thyroid carcinomas, which produced thyroglobulin and were unrelated to anaplastic carcinoma, showing an intermediate behavior between follicular/papillary and anaplastic carcinomas. Different terms were selected to refer to these tumors, including solid (1), trabecular (2), insular (3,4), poorly differentiated (1,5-6), intermediate type (7), primordial cell (8), less well differentiated (9) carcinoma, or follicular carcinoma with insular component (10). On the one hand these tumors have been defined according to their growth pattern, being among the variable histological patterns recognized in such tumors, trabecular/insular/solid (TIS) areas usually predominant. Conversely, some authors pointed out that PD carcinomas are characterized by unequivocal high grade histology, with atypias, high mitotic count and necrosis, rather than by a specific growth pattern (11-14), thus including in some instances high grade variants (i.e. tall cell or columnar) of papillary carcinomas in the PD tumors group (11,14). As a consequence, there are several different criteria that define PD carcinoma and most published series are not easily comparable. Additional source of controversies on PD carcinomas comes from some studies (6,8,15), following the original observation of Carcangiu and coworkers (3), which incorporated in the PD carcinoma group both follicular-derived and papillaryderived tumors, whereas others (14,16,17) considered solid papillary carcinoma as a tumor separate from PD carcinoma, unless necrosis is present within the tumor (17). Recent molecular evidence have shown that a link of PD carcinoma and papillary carcinoma exists also from a genetic point of view, since the RET/PTC1 rearrangement (typical of papillary carcinoma) was also found in a fraction of PD carcinomas having the nuclear features of papillary carcinoma and/or some (residual) foci of papillary carcinoma (18). Moreover, very recently activating BRAF mutations, specific of papillary carcinomas, have been detected in a series of PD carcinomas having residual papillary carcinoma foci (19). This indicates that PD carcinoma may de-differentiate from either well differentiated conventional follicular or even papillary carcinoma. Another source of debate concerning the histogenetic relationship between PD carcinomas and other thyroid tumors refer to the presence of an oxyphilic phenotype in PD carcinomas. Oxyphilic carcinomas have long been considered a separate entity based on their apparently higher malignant potential, and therefore excluded from several studies. Others (20-22) have shown that oxyphilic tumors by no means differ from conventional follicular or even solid/trabecular carcinomas, except for their mitochondrion1 rich cytoplasm. Concerning the extent of TIS growth patterns which have to be recognized to make a diagnosis of PD carcinoma, it is generally accepted that a PD carcinoma is defined by the presence of 75% or more of such areas. However, if even a minor TIS component could affect the prognosis of an otherwise folicular/papillary carcinoma is still a matter of discussion. In fact, the observation that even a minor insular component was associated with a prognosis worse than that of the control well differentiated follicular carcinoma had already been reported by Nishida and coworkers (6), while not confirmed by other Authors (10). On the search of prognostic factors. As already mentioned above, it is well known that the group of PD carcinomas behave intermediately between well differentiated and anaplastic carcinomas. However, in this tumor group no data were available on large case series concerning prognostic factors. Recently, some authors (23,24) analyzed the influence of histological parameters such as atypias, mitoses and necrosis on the prognosis of well differentiated papillary carcinoma. It was shown that a malignant behavior was significantly associated with the presence of such high grade features rather than related to the pattern of growth. Since some PD carcinomas have a fatal outcome and others follow an indolent course, we decided to apply the same approach. The influence of clinical and histological parameters on prognosis was analyzed in a large series of 183 PD carcinomas of the thyroid, in which TIS patterns of growth were more or less extensively represented (165 cases) or were only focally recognized (18 remaining cases). Clinico-pathological features such as sex, age, tumor diameter, stage, therapy administered, extent of TIS patterns, presence of oxyphilic features, presence of necrosis, mitotic count, cell size, extent of vascular invasion, and type of associated component (follicular vs papillary) were studied by univariate and multivariate overall survival analysis and compared with the clinical outcome. Subgroups included tumors having predominant oxyphilic features (n=66) and (residual) papillary carcinoma features (n=24). Control groups of papillary (n=68), follicular (n=71) and anaplastic (n=35) carcinomas were also included for overall survival analysis. Our data (25), showed that PD carcinomas had an intermediate behavior between papillary/follicular and anaplastic carcinomas (p<0.0001). Univariate and multivariate statistical analysis demonstrated that age >45 years (p=0.007), presence of necrosis (p<0.0001) irrespective of its extent (focal versus extensive), and mitotic count >3x10HPF (p=0.01) were associated with poor outcome. No statistically significant differences were observed comparing the patient’s sex, tumor size (cutoff 4 cm) and radioiodine therapy administered and the overall survival. No significant differences in behavior were observed between minimally and widely invasive TIS carcinomas. Relating the extent of the TIS component with clinical behavior, we did not find any statistically significant difference in the overall survival of carcinomas having only minor TIS component (102 50%) versus those with a well represented (50-75%) component versus virtually “pure” TIS carcinomas (> 75%), although a better prognosis was observed in cases with minor TIS component compared to the latter two groups considered together (p=0.08). From a practical point of view, we suggest that the presence of a TIS component must appear in the final pathological report of a thyroid carcinoma. If the tumor also shows aggressive features (large tumor size, necrosis, mitoses), then the diagnosis of “poorly differentiated” carcinoma with TIS patterns is appropriate. Prognostic scoring system. Overall, these findings indicate that combining the statistically significant parameters into a scoring system, PD carcinomas can be grouped into three prognostic categories (p<0.0001). Group 1 (score 0-1) had a survival overlapping to that of well differentiated papillary and follicular carcinomas. Group 3 (score 4-5) showed a clinical course closer to that of anaplastic carcinoma, while group 2 (score 2-3) had a survival curve intermediate between the former two. From a practical point of view, since PD carcinomas all together represent a clinically heterogeneous group of tumors, we suggest that this scoring system may be useful to identify those tumors which have a higher risk of an unfavourable clinical outcome. Proposed scoring system: Presence of necrosis (either focal or diffuse): Age > 45 years: Mitotic count > 3/10HPF: SCORE 3 SCORE 1 SCORE 1 Prognostic groups: Group 1: score 0-1 Group 2: score 2-3 Group 3: score 4-5 Cumulative proportion surviving Histological diagnosis 1 FC Group 1 PTC 0,8 0,6 Group 2 0,4 Group 3 p < 0.0001 0,2 AC Scoring system: Group 1: score 0-1 Group 2: score 2-3 Group 3: score 4-5 0 0 60 120 180 240 Time (months) 300 360 3 Concluding remarks. In this study, we have confirmed that poorly differentiated TIS carcinomas of the thyroid have a clinical behavior intermediate between follicular/papillary carcinoma and anaplastic carcinoma. This is in agreement with the literature data (3,26-28) and with our previously reported findings (8). We here show that in PD carcinomas, age >45 years, presence of necrosis and mitotic index > 3 were significantly affecting prognosis. The classification of PD carcinomas into a separate group (also encompassing solid/trabecular oxyphilic carcinomas) appears justified, irrespective of the label which these tumors are to be referred to. Moreover, three different prognostic categories can be specifically identified by a scoring system applied to clinicopathological parameters as age of patient, presence of necrosis and mitotic count. In more general terms, in agreement with LiVolsi and coworkers (24,29), our data suggest that the grading of thyroid carcinoma is of high prognostic and clinical value. A scheme defining the proposed spectrum of follicular-derived thyroid carcinomas as compared to their differentiation and clinical behaviour is shown below. Well diff. FTC Minimally invasive PTC Classical Follicular Undiff. DIFFERENTIATION FTC Widely invasive PTC Aggressive variants TISC Necrosis absent Mitoses < 3 Age < 45 TISC Necrosis present Mitoses >3 Age > 45 AC Good PROGNOSIS Poor 4 REFERENCES 1. Sakamoto A, Kasai N, Sugano H. Poorly differentiated carcinoma of the thyroid. A clinicopathologic entity for a high-risk group of papillary and follicular carcinomas. Cancer. 1983;52:1849-55. 2. Cabanne F, Gerard-Marchant R, Heimann R, Williams ED. Tumeurs malignes du corps thyroide. Problèmes de diagnostic histopathologique. A propos de 692 lèsions recuilles par le groupe coopèrateur de l’O.E.R.T.C. Ann Anat Pathol. 1974;19:129-48. 3. Carcangiu ML, Zampi G, Rosai J. Poorly differentiated ("insular") thyroid carcinoma. Am J Surg Pathol. 1984;8:655-68. 4. Pilotti S, Collini P, Mariani L el al. Insular carcinoma: a distinct de novo entity among follicular carcinomas of the thyroid gland. Am J Surg Pathol. 1997;21:1466-73. 5. Sobrinho-Simoes M, Sambade C, Fonseca E, Soares P. Poorly differentiated carcinomas of the thyroid gland: a review of the clinicopathologic features of a series of 28 cases of a heterogeneous, clinically aggressive group of thyroid tumors. Int J Surg Pathol. 2002;10:123-31. 6. Nishida T, Katayama S, Tsujimoto M, Nakamura J, Matsuda H. Clinicopathological significance of poorly differentiated thyroid carcinoma. Am J Surg Pathol. 1999;23:205-11. 7. Ljungberg O, Bondeson L, Bondeson AG. Differentiated thyroid carcinoma, intermediate type: a new tumor entity with features of follicular and parafollicular cell carcinoma. Hum Pathol. 1984;15:218-28. 8. Papotti M, Botto Micca F, Favero A, Palestini N, Bussolati G. Poorly differentiated thyroid carcinomas with primordial cell component. A group of aggressive lesions sharing insular, trabecular, and solid patterns. Am J Surg Pathol. 1993;17:291-301. 9. Byar DP, Green SB, Dor P, Williams ED et al. A prognostic index for thyroid carcinoma. A study of the E.O.R.T.C. Thyroid Cancer Cooperative Group. Eur J Cancer. 1979;15:1033-41. 10. Ashfaq R, Vuitch F, Delgado R, Albores-Saavedra J. Papillary and follicular thyroid carcinomas with an insular component. Cancer. 1994;73:416-23. 11. Sobrinho-Simões M. Poorly differentiated thyroid carcinomas. Endocr pathol. 1996;2:99102. 12. Akslen LA, LiVolsi VA. Poorly differentiated thyroid carcinoma--it is important. Am J Surg Pathol. 2000;24:310-3. 13. Nishiyama RH. Another dissertation on poorly differentiated carcinomas: is it really necessary? Adv Anat Pathol. 1999;6:281-6. 5 14. Pilotti S, Collini P, Manzari A, Marubini E, Rilke F. Poorly differentiated forms of papillary thyroid carcinoma: distinctive entities or morphological patterns? Semin Diagn Pathol. 1995;12:249-55. 15. Tallini G, Garcia-Rostan G, Herrero A et al. Downregulation of p27KIP1 and Ki67/Mib1 labeling index support the classification of thyroid carcinoma into prognostically relevant categories. Am J Surg Pathol. 1999;23:678-85. 16. Mizukami Y, Noguchi M, Michigishi T ed al. Papillary thyroid carcinoma in Kanazawa, Japan: prognostic significance of histological subtypes. Histopathology. 1992;20:243-50. 17. Nikiforov YE, Erickson LA, Nikiforova MN, Caudill CM, Lloyd RV. Solid variant of papillary thyroid carcinoma: incidence, clinical-pathologic characteristics, molecular analysis, and biologic behavior. Am J Surg Pathol. 2001;25:1478-84. 18. Santoro M, Papotti M, Chiappetta G et al. RET activation and clinicopathologic features in poorly differentiated thyroid tumors. J Clin Endocrinol Metab. 2002;87:370-9. 19. Nikiforova MN, Kimura ET, Gandhi M, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas. J Clin Endocrinol Metab. 2003;88:5399-404. 20. Papotti M, Torchio B, Grassi L, Favero A, Bussolati G. Poorly differentiated oxyphilic (Hurthle cell) carcinomas of the thyroid. Am J Surg Pathol. 1996;20:686-94. 21. Evans HL, Vassilopoulou-Sellin R. Follicular and Hurthle cell carcinomas of the thyroid: a comparative study. Am J Surg Pathol. 1998;22:1512-20. 22. Heffess CS, Thompson LDR. Minimally invasive follicular thyroid carcinoma. Endocrine Pathol 2001;12:417-22. 23. Decaussin M, Bernard MH, Adeleine P et al. Thyroid carcinomas with distant metastases: a review of 111 cases with emphasis on the prognostic significance of an insular component. Am J Surg Pathol. 2002;26:1007-15. 24. Akslen LA, LiVolsi VA. Prognostic significance of histologic grading compared with subclassification of papillary thyroid carcinoma. Cancer. 2000;88:1902-8. 25. Volante M, Landolfi S, Chiusa l, et al. Poorly differentiated carcinomas of the thyroid with trabecular, insular and solid patterns. A clinico-pathological study of 183 cases. Cancer. 2004 (in press) 26. Rosai J, Carcangiu ML, De Lellis RA. Tumors of the thyroid gland. In: Atlas of tumor pathology. Washington: Armed Forces Institute of Pathology, 1992:161-82. 6 27. Pellegriti G, Giuffrida D, Scollo C et al. Long-term outcome of patients with insular carcinoma of the thyroid: the insular histotype is an independent predictor of poor prognosis. Cancer. 2002;95:2076-85. 28. Sasaki A, Daa T, Kashima K, Yokoyama S, Nakayama I, Noguchi S. Insular component as a risk factor of thyroid carcinoma. Pathol Int. 1996;46:939-46. 29. LiVolsi VA, Baloch ZW. Predicting prognosis in thyroid carcinoma: can histology do it? Am J Surg Pathol. 2002;26:1064-5. 7