Tumor Lysis Syndrome - American Association of Critical
advertisement
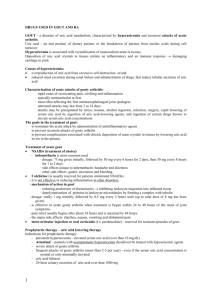
Tumor Lysis Syndrome Carol S. Viele RN, MS Clinical Nurse Specialist Hematology-Oncology-Bone Marrow Transplant Definition Potentially fatal metabolic complication that occurs in some patients with cancer Can result in potentially life threatening metabolic and electrolyte abnormalities Pathophysiology Involves a complex series of events related to the liberation of intracellular contents from tumor cells and inability of the kidneys to excrete and maintain normal serum composition Manifestations Usually occurs within 24-48 hours after initiation of chemotherapy and may persist for 5-7 days post therapy May occur as early as 6 hours post chemotherapy administration Tumor Types Non-Hodgkins lymphoma – Burkitt’s – High grade T-cell Acute Leukemia’s – Acute Promyelocytic leukemia – Acute lymphoblastic leukemia Chronic Lymphoblastic leukemia Solid tumors – Small cell lung cancer – Breast cancer Symptoms Cardiac: – Presence of S3 – Bradycardia – Heart Block – Cardiac Arrest Symptoms Neuromuscular: – Weakness – Lethargy – Cramping – Tetany – Chvostek’s sign – Trousseau’s sign – Convulsions Symptoms Renal: – Oliguria – Renal Insufficiency – Flank pain – Weight gain – Edema – Renal failure Symptoms Gastrointestinal: – Nausea – Vomiting – Diarrhea – Constipation Hyperuricemia Results from tumor cell destruction Most common signs and symptoms: – Nausea and vomiting – Azotemia – Oliguria – Anuria – Decreased urine pH – Uric acid crystals found in urinalysis Hyperkalemia Results from rapid destruction of cells Most common signs and symptoms – EKG changes Peaked t waves Flat p waves Wide QRS complexes Bradycardia Ventricular tachycardia Ventricular fibrillation Asystole Pulseless electrical activity Hyperkalemia Results from rapid destruction of cells Most common signs and symptoms – Weakness – Twitching – Increased bowel sounds – Nausea – Diarrhea Hyperphosphatemia Most common signs and symptoms – Hypocalcemia – Renal failure Azotemia Ologuria Anuria – Hypertension – Edema Hypocalcemia Results from hyperphosphatemia and the inverse relationship between calcium and phosphorous Most common signs and symptoms – EKG changes Prolonged QT Inverted T waves Ventricular dysrhythmias Heart block Cardiac arrest Hypocalcemia Neuromuscular signs and symptoms – Tetany – Twitching – Paresthesias – Seizures GI Symptoms – Diarrhea Diagnostic Tests Chvostek – Tapping the cheek below the temple where the facial nerve emerges Diagnostic Tests Trousseau Sign – Occluding the arterial blood flow in the arm with the blood pressure cuff for one to five minutes, if the thumb adducts and the phalangeal joints extend the test is positive Prevention Identify patients at risk Monitor for all electrolyte abnormalities Administer allopurinol, – Decrease uric acid levels by interfering with purine metabolism through the inhibition of the enzyme xanthine oxidase that is essential for the conversion of nucleic acids to uric acid Alkalinization of the urine – Prevent as much as possible renal damage Sodium bicarbonate solution – Decreases the risk of renal obstruction, however urinary alkalinization should be used cautiously because of risk of precipitation in the kidneys of calcium-phosphorous binding and the risk of hypocalcemic induced neuromuscular irritability Prevention Rasburicase- recombinant urate oxidase– Reduces the uric acid pool – Reduces existing uric acid – Prevents the accumulation of xanthines and hypoxanthine – Does not require alkalinization – Facilitates phosphorous excretion – Dosing: – IV over 30 minutes – 0.2 mg/kg IV QD or BID Management Hydration – 3 Liters daily – Aggressive hydration starting 1-2 days prior to chemotherapy and continuing for a few days post chemotherapy Management Diuretics: – Furosemide Renal dose Dopamine- 2-4 mcg/kg Prevents: – Fluid overload – Electrolyte imbalance – Complications of uric acid buildup Management Hyperkalemia – Kayexalate with sorbitol PO Rectal – Calcium Gluconate – Sodium bicarbonate – Hypertonic dextrose and regular insulin – Albuterol (Ventolin) or another beta stimulant Management Dialysis: Hemodialysis/CVVH/CRRT( Requires ICU Care) – Used for patients unresponsive to preventive measures and electrolyte corrections – Used to remove uric acid – Used in patients with: Serum potassium >6 mEq/L Uric acid >10 mg/dl Phosphorous > 10 mg/dl Symptomatic hypocalcemia Presence of volume overload Medication Management Avoid nephrotoxic medications Avoid agents which block tubular reabsorption of uric acid – Aspirin – Probencid – Thiazide diuretics – Radiographic contrast containing iodine Nursing Interventions Symptom management Maintenance of fluid status Review of systems – Cardiac via EKG – Neurologic – Neuromuscular – Gastrointestinal – Renal Nursing Interventions Monitor weights at least daily Daily EKG’s Monitor for altered level of consciousness Strict I&O Check pH of urine with each void, goal is to keep pH >7.0 Monitor for signs and symptoms of nausea and vomiting, administer antiemetics as ordered References Jeha,S., Pui, C. ‘Recombinant Urate Oxidase (Rasburicase) in the Prophylaxis and Treatment of Tumor Lysis Syndrome, Ronco,R. Rodeghiero, F. (eds) Hyperuricemic Syndrome: Pathophysiology and Therapy, Contrib Nephrol, Basel,Karger,2005,Vol 147,pp69-79 References Reid-Finlay,M. Kaplow, R. ‘Leukemia and Bone Marrow Transplantation’, Schell,H., Puntillo, K., Critical Care Nursing Secrets, Hanley and Belfus, Inc, Philadelphia 2001,p. 209-215 Zobec,A., ‘Tumor Lysis Syndrome’, Oncology Nursing Secrets, Hanley and Belfus, 2008, p. 557-560