Animal_Biosafety_Procedures_Infectious_Agents_Non
Inoculation of Infectious Agents in
Non-Rodent Species
Animal
Biosafety
Procedures
1. Purpose and Scope
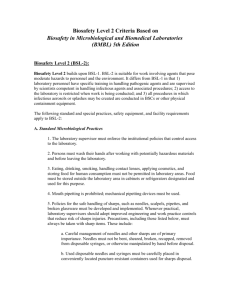
This Animal Biosafety Procedure (ABP) describes prudent practices, procedures, and equipment to reduce risk when inoculating infectious agents in non-rodent animal species that cannot be manipulated inside a biosafety cabinet (e.g., goats, cows, dogs, cats). The practices and procedures outlined in this document are in accordance with those described for Animal Biosafety Level 2 (ABSL-2) in the CDC/NIH Biosafety in
Microbiological and Biomedical Laboratories (BMBL), 5 th edition
( http://www.cdc.gov/biosafety/publications/bmbl5/index.htm
).
***Alternative practices, procedures, and equipment may be used, but they must be described in a user-generated standard operating procedure, and approved by EHS and the IACUC before use.***
2. Responsibilities
The Principal Investigator will ensure that personnel are made aware of the hazards associated with the infectious agent and that they receive training commensurate with their activities, including handling techniques for the particular animal species, prior to commencing ABSL-2 experiments. Personnel will comply with the safe work practices and procedures described within this Animal Biosafety Procedure.
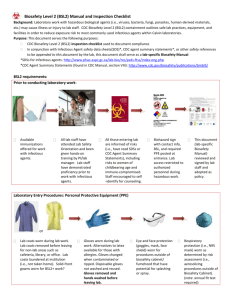
3. Administrative Controls
3.1 Training
3.1.1 Receive laboratory-specific training for safe manipulation of the infectious agent, symptoms associated with accidental exposure, and spill and exposure response procedures.
3.1.2 Receive training in safe handling techniques for the specific animal species.
3.1.3 CARE and EHS will provide additional on-site training, as necessary.
3.2 Access and Signage
3.2.1 Inform the facility manager prior to introducing infectious agents in animals.
3.2.2 Review the hazards and potential risks of the experiment, and complete IACUC module 2 before accessing the animal facility.
3.2.3 The facility supervisor will post a hazard sign at the entrance to the animal room. Research,
EHS, and CARE staff will develop information contained in the sign, which will include:
The biohazard symbol and ABSL-2 designation
The name of the Principal Investigator and IACUC protocol number
Name of infectious agent, as well as human and animal clinical signs of infection
Potential shedding of the agent by the animal
Personal protective equipment
Disinfectant to be used
Contact information for CARE, EHS, and Gannett Health Services
3.3 Medical Surveillance
3.3.1 Participate in the Animal Users Health and Safety Program (AUHSP).
4. Work Practice and Procedure Controls
4.1 Inoculation of animals
4.1.1 See Section 6.1 for specific personal protective equipment.
4.1.2 Use an appropriate manual restraint or physical restraint device. If the procedure or conditions of inoculation pose too high a risk with an awake animal (e.g., animal species difficult to handle, inexperienced individual performing the procedure), sedate the animal prior to inoculation.
Approved by: Institutional Biosafety Committee 12/13/11
Last revised by: Frank A. Cantone
Revision date: 12/07/2011
726983907
Page 1 of 3
The most recent version of this document is available electronically at: http://sp.ehs.cornell.edu/lab-research-safety/bios/animalresearch/Pages/default.aspx
Inoculation of Infectious Agents in Non-Rodent Species
4.2 Sharps Handling
4.2.1 Substitute plasticware for glassware whenever possible, and implement the following safe practices for handling sharps:
Limit the use of sharps to when no other alternatives are available
Keep all sharps in full view at all times
Use only Luer-lock syringes and needles or units where the needle is integral to the syringe
Implement safety engineered sharps where practical
Dispose of sharps directly, without manipulation (i.e., do not bend, shear, break, recap, or use hands to remove needles from syringes or blades from scalpels), in an approved sharps disposal container. Maintain disposal container in animal room within arm’s reach
Handle broken glass or other sharps with a secondary device such as forceps or broom and dustpan- not your hands
4.2.2 Do not recap needles. However, if recapping must be done first receive approval by EHS and the
IACUC, and use one of the following two methods: one handed scoop technique; forceps or tongs to place the cap on the needle.
4.3 Hygiene
4.3.1 Eating, drinking, smoking, handling contact lenses, applying cosmetics, storing food for human consumption, and mouth pipetting are strictly prohibited in animal facilities.
4.3.2 Wash hands thoroughly with soap and water after removing gloves. Use an alcohol-based hand sanitizer if sink is not readily available.
4.4 Decontamination and Spill Response
4.4.1 Decontaminate work surfaces and equipment with a suitable disinfectant- allow at least 5-10 minutes of contact time. Suitable disinfectants must be active against the targeted agent, and address factors such as environment (e.g., organic load, surfaces) contact time, application, and safety: http://www.cfsph.iastate.edu/BRM/resources/Disinfectants/CharacteristicsSelectedDisinfectants.pdf
4.4.2 Cover spills of inoculum with absorbent towels/pads and saturate with disinfectant. Allow 5-10 minutes contact time to achieve adequate disinfection. Appropriately segregate waste in red biohazard bags or sharps disposal containers and re-apply disinfectant to spill area.
4.5 Handling of Waste
4.5.1 Dispose of sharps-related items (e.g., needles, syringes, blood tubes) directly in a sharps disposal container.
4.5.2 Dispose of non-sharps items (e.g., gloves, intact plasticware) in a red biohazard bag.
4.5.3 Treat any remaining inoculum with concentrated household bleach to a final volume of 10% bleach and allow at least 30 minutes contact time before disposal in the sanitary waste drain- follow with copious amounts of water.
4.5.4 Coordinate handling of infectious carcasses with animal care staff. Appropriate disposal may include packaging in red biohazard bags or covered carts.
4.6 Transport of Biohazardous Materials
4.6.1 Transport infectious agents and contaminated samples between the laboratory and animal facility in a sealed, secondary container with absorbent toweling, and labeled with the biohazard symbol.
4.7 Tissue Harvest
4.7.1 Arrange with animal care staff for transport of animals to an appropriate room or facility to euthanize animals and harvest tissues (e.g., necropsy floor at the Animal Health Diagnostic
Center). Alternatively, perform euthanasia and tissue harvest in the animal room.
4.7.2 When possible, use only one sharps item (e.g., knife, scissors) at a time and keep in full view.
4.7.3 Place any harvested tissue or fluids in appropriate primary containers (e.g., screw top vial, sealable plastic bag), decontaminate exterior of container, and transport as per section 4.6.
Fixed tissues (e.g., 10% buffered formalin) are no longer considered biohazardous. Use appropriate personal protective equipment when handling these samples and transport in a secondary container.
4.7.4 Follow the sharps handling practices outlined in section 4.2.
Approved by: Institutional Biosafety Committee 12/13/11
Last revised by: Frank A. Cantone
Revision date: 12/07/2011
726983907
Page 2 of 3
The most recent version of this document is available electronically at: http://sp.ehs.cornell.edu/lab-research-safety/bios/animalresearch/Pages/default.aspx
Inoculation of Infectious Agents in Non-Rodent Species
5. Housing and Handling of Infected Animals
5.1 House animals in a holding area with an adjacent anteroom. Prepare inoculum and supplies, and don personal protective equipment (as indicated in section 6) within the anteroom.
5.2 When possible, have someone assist you when inoculating, euthanizing animals, or collecting samples.
6. Personal Protective Equipment (PPE)
6.1 Don the following minimum PPE before entering ABSL-2 animal rooms:
Disposable fluid resistant coveralls
Disposable gloves (nitrile- avoid latex when possible) - Use double gloves when handling the infectious agent or when inoculating animals. Outer glove should overlay cuff of coverall
Boots or shoe covers
6.2 Wear additional PPE when indicated by the agent, animal species, hazards, or experimental conditions:
Face mask and eye protection (e.g., safety glasses or face shield)
Hair net
Cut/bite resistant gloves
Respiratory protection
6.3 Solid toed shoes are required for entry into animal rooms.
6.4 Remove PPE upon exiting the animal room and dispose in red biohazard bag. First remove outer gloves, gown (turning inside out), hair net, facial protection, boots or shoe covers while stepping out of the room
(step-over technique), and finally inner gloves.
7. Response to Accidental Exposures
7.1 Personnel who sustain an overt exposure such as a splash to mucous membranes, direct contact with open wounds, or a sharps injury should:
Wash exposed area with soap and water or rinse in eye wash for at least 10 minutes
Perform first aid, if applicable
Notify supervisor
Seek medical evaluation at Gannett Health Services, Occupational Medicine (255-6960) as soon as possible after an exposure or injury. After hours seek evaluation at Cayuga Medical Center.
Contact Gannett Occupational Medicine if you develop symptoms suggestive of exposure to the hazardous agent.
Document exposures, injuries, and illnesses in the Cornell University Injury/Illness/Exposure Report, http://cfp-rmps.coldfusion.cornell.edu/accinj/ .
8. Emergency Phone Numbers
Police, Fire, and Medical Emergencies: 911
Environmental Health & Safety (EHS): 255-8200 (off hours 255-1111)
Gannett Health Services, Occupational Medicine: 255-6960 (off hours 255-5155)
Cornell Animal Resources and Education (CARE): 253-4378 (off hours 1-800-349-2456 for veterinary medical emergencies)
9. References
9.1 Biosafety in Microbiological and Biomedical Laboratories, 5 th edition. 2009. Centers for Disease Control and Prevention, National Institutes of Health.
Approved by: Institutional Biosafety Committee 12/13/11
Last revised by: Frank A. Cantone
Revision date: 12/07/2011
726983907
Page 3 of 3
The most recent version of this document is available electronically at: http://sp.ehs.cornell.edu/lab-research-safety/bios/animalresearch/Pages/default.aspx