Practice -9
advertisement
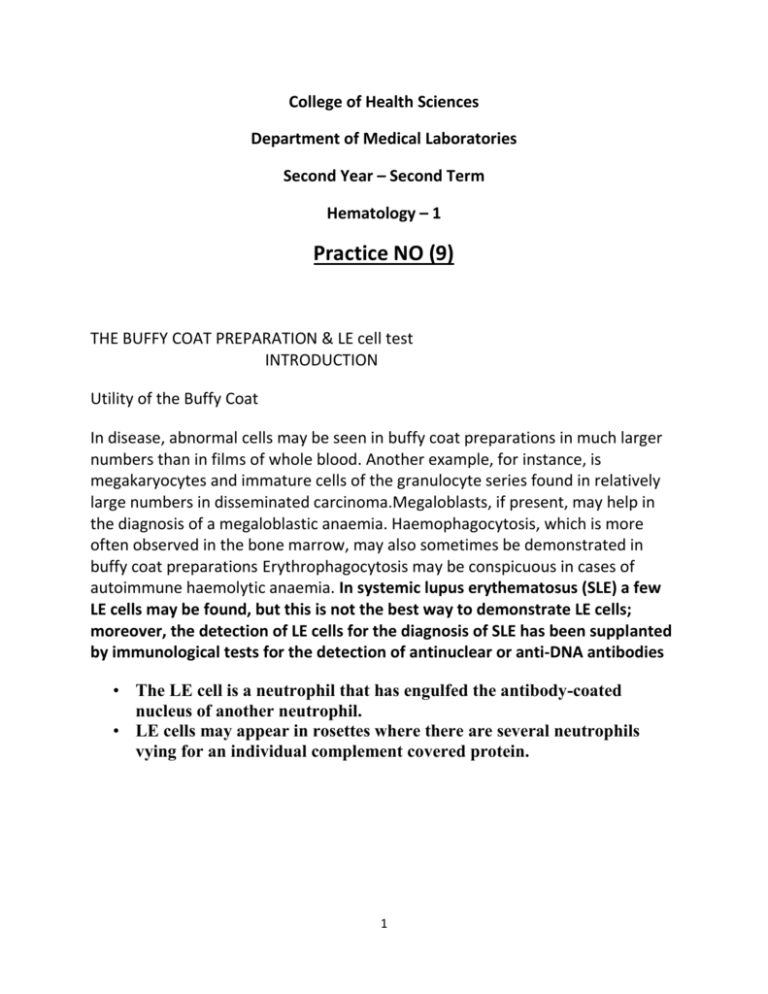
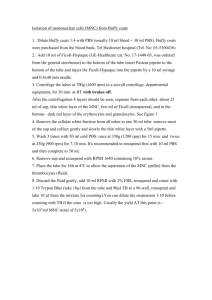
College of Health Sciences Department of Medical Laboratories Second Year – Second Term Hematology – 1 Practice NO (9) THE BUFFY COAT PREPARATION & LE cell test INTRODUCTION Utility of the Buffy Coat In disease, abnormal cells may be seen in buffy coat preparations in much larger numbers than in films of whole blood. Another example, for instance, is megakaryocytes and immature cells of the granulocyte series found in relatively large numbers in disseminated carcinoma.Megaloblasts, if present, may help in the diagnosis of a megaloblastic anaemia. Haemophagocytosis, which is more often observed in the bone marrow, may also sometimes be demonstrated in buffy coat preparations Erythrophagocytosis may be conspicuous in cases of autoimmune haemolytic anaemia. In systemic lupus erythematosus (SLE) a few LE cells may be found, but this is not the best way to demonstrate LE cells; moreover, the detection of LE cells for the diagnosis of SLE has been supplanted by immunological tests for the detection of antinuclear or anti-DNA antibodies • The LE cell is a neutrophil that has engulfed the antibody-coated nucleus of another neutrophil. • LE cells may appear in rosettes where there are several neutrophils vying for an individual complement covered protein. 1 Skin Manifestations • Malar or Butterfly Rash • Discoid Rash – Stimulated by UV light • Skin manifestations only appear in 30-40% of lupus patients. 2 • Lupus = Autoimmunity – Systemic and affects connective tissue • Caused by malfunctions of: – T-cells – B-cells – Complement System – Signal Transduction • Can be lethal or not • Unique to each individual When a tube of blood (regardless of its diameter) is centrifuged the blood will separate from bottom to top in the following layers: erythrocytes (the bottom layer), leukocytes, platelets, and plasma (forming the top layer). The grayishwhite layer that forms above the erythrocyte layer is called the “buffy coat.” Refer to the lab experiment for the manual hematocrit for an illustration of the layered arrangement of the blood components. This concentrated layer of leukocytes (with the platelets) can be removed and formed into a smear for staining. This is the buffy coat smear. The following are advantages in performing this type of examination of stained leukocytes: 01 In leukocytopenia, increased numbers WBC’s may be reviewed with increased chances of identifying anomalies. 02 In aleukemic leukemia, the opportunity of finding immature leukocytes is enhances. 03 it may emphasize the need for a bone marrow biopsy or provide information that nullifies the need for such a procedure. A word of caution is in order. This procedure is not generally recommended for performing differential counts. The presence of nucleated blood cells can alter the randomization of distribution of these cells because such cells have a tendency to sediment into layers according to their cell type. This is a centrifugation anomaly that results in population aggregation areas of the same cell types. It has been advocated by some laboratory specialists that a differential can be performed on leukopenic blood and the differential correlates to that of a standard blood smear. 3 PROCEDURE 01 The buffy coat may be prepared using a capillary tube, Wintrobe tube, or test tube. 02 Blood is collected and the buffy coat should be immediately made. EDTA blood should not be allowed to stand any length of time before preparing the smear. WARNING – Blood that has been allowed to remain in EDTA for an hour or longer is highly likely to display morphological distortions in a buffy coat preparation. In such buffy coat smears, smudge cells and necrobiotic cells are more often encountered. 03 Using the plain capillary tube (wear gloves for this procedure): A. Fill the capillary tube about 80% full with well mixed anticoagulated blood. B. Plug one end of the capillary tube and place in a hematocrit tube. C. Centrifuge for about 2 minutes (less that the normal packing time for a manual hematocrit) to minimize cellular distortion. D. Score the capillary tube at a point just below the buffy coat layer (just in the RBC layer) with a diamond point pencil or special file. E. Hold the tube with fingers of both hands and break the tube at the scored mark, avoiding glass fragments. F. Discard the section with RBC’s and hold the upper capillary tube (with the buffy coat layer) and touch the scored end to a clean glass slide. a. You may need to hold the fore finger over the tube to control the flow of the plasma. b. A special capillary bulb may be use to control the flow. c. Allow the thin layer of RBC’s, buffy coat, and small amount of plasma to flow onto the slide. G. Using the end of the capillary tube, gently rotate and mix the cells and plasma. H. Lay aside the piece of capillary tube and using a second slide, make a wedge shaped film. I. Allow air dry, then stain with Wright’s stain. After staining, you may “coverslip” the buffy coat smear and examine the slide. J. NOTE: If the capillary tube is heparinized, then expect to see an increase in the number of leukocytes and platelets that are adhering 4 to each other. Additionally, the staining of the WBC’s may appear to be more basic (blue). K. If the patient is significantly leukopenic, then two or more capillary tubes may be used to increase the amount of buffy coat material. A. Express the buffy coat layers and plasma into a watch glass or other suitable device. Mix the samples with a Pasteur pipette and after mixing, place a drop on a slide and proceed as directed in step “I”. 04 Technique with the Wintrobe tube (this is the preferred and recommended method). A. With well-mixed EDTA blood, using a long tipped Pasteur pipette, fill the Wintrobe hematocrit tube . B. Centrifuge at one of the following speeds (higher speeds may cause cellular distortion): a. 5 minutes at 2000 rpm b. 10 minutes at 1000 rpm C. Using a long-tipped Pasteur pipette, remove the plasma layer until only a small interface layer lies above the buffy coat. Discard this plasma layer. D. With the Pasteur pipette, remove the buffy coat layer and also the topmost layer (as thin as possible). E. The amount of mixture will be too large to express onto a slide to make a smear. Proceed with the following steps: a. Express the mixture into a watch glass (or something similar) and rinse the mixture back and forth (gently) several times. This will mix the mixture and remove many of the cells that tend to stick to the glass sides of the pipette. b. Transfer a drop of the mixture to a 3 × 1 inch glass slide and prepare a push-type wedge smear. F. Air dry and stain with Wright’s stain. The smear may fixed with a glass coverslip before viewing. G. A larger concentrate can be prepared in a manner similar to that describe for the capillary procedure. Things to think about when evaluating the buffy coat stained blood smear. 01 The preparation process represents potentially significant manipulations and in most cases a buffy coat smear should not be used to: A. estimate relative or absolute leukocyte counts. B. evaluate mature erythrocyte morphology. 5 02 03 C. quantitate thrombocytes. The buffy coat smear may be used to: A. describe which leukocyte populations are predominant. B. describe the presence of nucleated cells (both WBC’s and RBC’s). C. locate and describe abnormalities in the blood cell populations. Remember this about the buffy coat preparation that is from a normal/healthy individual: A. If is very possible that you may find an occasional or rare myelocyte, metamyelocyte, metarubricyte, or megakaryocyte fragments in these smears.....and it does not mean that something abnormal is taking place. Also, most often, an immature RBC is a highly unlikely finding. B. Monocytes tend to behave oddly. They tend to form clusters in the buffy coat. When you have finished with the laboratory exercise, complete the following: 01 On a sheet of typing paper, write your name in the upper right corner and below your name, include the type of lab experiment, and date. 02 For the first item (#1), Draw a capillary tube, divide the blood column into its layers and label the layers. 6