(See Power point lecture for additional information on the NOTES
advertisement

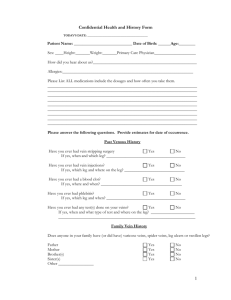
Venography Rt 255 Spring rev 2010 Week 10 (11)– Mon D. Charman pg 1 (See Power point lecture for additional information on the NOTES preview) Purpose of Venography Venography is an x-ray exam that provides an image of the veins (leg) after a contrast is injected into a vein in the patient's foot Enables the condition of the deep leg veins to be assessed Primarily performed to diagnose deep vein thrombosis DVT Indications Distinguish blood clots from obstructions in the veins Evaluate congenital vein problems Assess the functioning of deep leg vein valves Identify a vein for arterial bypass grafting (CABG) Deep vein thrombosis (DVT) is a common but elusive illness that can result in suffering and death if not recognized and treated effectively. DVT occurs in ~2 million Americans each year. Death can occur when the venous thrombi break off and form pulmonary emboli, which pass to and obstruct the arteries of the lungs. DVT and pulmonary embolism (PE) most often complicate the course of sick, hospitalized patients but may also affect ambulatory and otherwise healthy persons. Deep vein thrombosis is a major complication in orthopedic surgical patients and patients with cancer and other chronic illnesses. DVT can be a chronic disease. Patients who survive the initial episode of DVT are prone to chronic swelling of the leg and pain because the valves in the veins can be damaged by the thrombotic process, leading to venous hypertension. LOWER LIMB DVT Venous thrombosis in the lower limb can involve the superficial leg veins, the deep veins of the calf (calf vein thrombosis), the more proximal veins, including popliteal veins, PE: the superficial femoral, common femoral, and iliac veins. Less commonly, thrombosis involves other veins in the body Pulmonary Embolism It is estimated that each year 600, 000 patients develop PE and that 60,000 die of this complication. This number exceeds the number of American women who die each year from breast cancer. PE is now the most frequent cause of death associated with childbirth. Women are a prime target for PE, being affected more often than men. Occurs when a clot forms or becomes lodged in the pulmonary artery Most commonly thrombus originates in the lower limbs and migrates Can lead to resp distress, heart failure or cardiogenic shock Symptoms are acute: Sudden coughing SOB Chest pain DVT vs. PE DVT usually occurs in lower leg. Impedes normal blood flow. DVT is stationary. PE is the result of a DVT breaking apart. Venography Rt 255 Spring rev 2010 Week 10 (11)– Mon D. Charman pg 2 The Danger of PE’s: 3rd leading cause of cardiovascular death in U.S. Venous Thrombosis : CH 8 Pathology venous thrombosis- the formation of blood clots within a vein These clots commonly form in the veins of the lower extremities and result from a slowing of the blood return to the heart. The contraction of the leg muscles assists with venous blood return; therefore, postoperative or bedfast patients are especially prone to this disorder. Phlebitis, an inflammation of the vein, is often associated with venous thrombosis - the combination of these disorders is thrombophlebitis. The thrombus formation generally begins in the valves of the deep calf veins where thromboplastin traps red blood cells to create the blood clot. Patients may be placed on anticoagulant drugs or receive thrombolytic therapy. Venous Thrombosis Cause Thrombus Incidence Thrombophlebitis Phlebitis Deep Vein Thrombosis Primarily involves lower limbs Major source of fatal PE Risks Restricted mobility Surgery Obesity Pregnant BC pills trips Plane Car Long Thrombosis & Embolism Intravascular clot Commonly in veins more than arteries 3 factors Where blood is slow Change in the wall of vessels Change in the blood itself Thrombus that becomes detached from the vessel wall Can easily flow to heart causing PE Severity depends on location of embolism Varicose Veins are diseased blood vessels that have become permanently dilated and can no longer efficiently carry blood back to the heart Dilated, elongated and tortuous vessels Most common to superficial veins of leg Multiple bluish nodules just under skin Development of collateral veins Valves are unable to prevent backflow Valves cease to function increasing blood volume is these veins Arteries carry blood away from the heart while veins return blood back to the heart. Varicose veins can arise when this system gets backed up Multiple round and oval calcifications in soft tissues (phleboliths) represent calcified thrombi Shows the degree of collateral circulation Demonstrates patency of the deep venous system Venography Rt 255 Spring rev 2010 Week 10 (11)– Mon D. Charman pg 3 Spider Veins Risk factors for spider veins are similar to those for varicose veins – age, heredity, pregnancy, hormonal changes, obesity and extended periods of standing – as well as sun exposure, particularly in fair-skinned people, and injuries to the skin surface. Some physicians believe that exercise, weight loss and the wearing of support hose and flat shoes instead of high heels can reduce the incidence of spider veins. Phlebitis Inflammation of a vein Often associated with venous thrombosis US usually used to diagnose Treated with anticoagulants Prior to Procedure Pt should fast or drink only clear fluids for four hours before the test - WHY Thorough PT history obtained Informed consent If pt is nervous about the doctor may give a sedative. Explanation of Procedure: Legs The catheter is inserted into PT vein (usually a vein in the foot) Contrast is slowly injected. Tourniquet may be tied around the ankle of the foot the contrast is injected into - may also place one on the thigh The procedure takes about 30 - 45 minutes Contrast injected into top of foot Local anesthetic May be unilateral or bilateral FILMING VARIES WITH RADIOLOGIST MAY NEED SCOUT FILMS 14 X 17 Cassettes starting at Ankles, Knees, Femurs, Pelvis, Abdomen & Chest may also be taken What will the ABD film demonstrate? Flush with saline mark syringe w/ band aid The patient is asked to keep the leg still Radiologist may use fluoroscopy A series of images taken via fluoro and/or overheads films are taken fill the deep venous system with contrast The body may be tilted (Delay 15 Min – IVP Film) Overheads or 14x14 Fluoro Cassettes Or Digital Images taken With & Without Tourniquet Atherosclerosis Left Leg: Arterial Study CONTRAST MEDIA Contrast Injectable Water Soluable Ionic Vs Non Ionic Venous Injection Saline Strength Sterile Labeled Stings during injection Aftercare Patients should drink large amounts of fluids to flush the remaining contrast solution from their bodies. The area around the incision will be sore for a few days. If there is swelling, redness, pain, or fever, the doctor should be notified. Pain medication may be needed. In most cases, the patient can resume normal activities the next day. Venography Rt 255 Spring rev 2010 Week 10 (11)– Mon D. Charman Risks & Complications phlebitis / infection at injection site tissue damage Formation of deep vein thrombosis in a healthy leg. A rare side effect in up to 8% of cases is a severe allergic reaction to the contrast. This usually happens within 30 minutes after injection Congestive heart failure Acute renal insufficiency Venous thrombosis in a healthy leg Dislodging a clot, perhaps resulting in pulmonary embolus or other complications pg 4 Abnormal results Abnormal venography results show well-defined filling defects in veins Findings include: Blood clots Major deep veins that are unfilled Consistent filling defects Contrast flow that is diverted - These results An abrupt end of a vessel confirm a diagnosis of deep vein thrombosis. Types of Other Venogram Procedures Leg (lower extremity) MOST COMMON Arm (upper extremity) Inferior Vena Cavagram Superior Vena Cavagram Adrenal Renal Saphenous Vein Catheter injection directly for upper leg DVT of Iliac Vein: On x-ray appears as a constant filling defect Largely replaced by duplex color doppler ultrasound - Demonstrates the velocity of the venous blood flow Post Femoral Vein Puncture Orders Bed rest for 2-4 hours with affected leg straight. (Physician will specify) Check puncture site for sign of bleeding. Check B.P. q 1 hour x 4 hours. fluids. Resume pre-venography activity Encourage Arteriogram – subclavian injection Review Anatomy of Upper Limb (RT 255 & 93 Inferior Vena Cavogram To view the inferior vena cava to determine strictures, tumor blockage and location of blood clots. A catheter is inserted in the femoral vein & positioned in the common iliac vein or the inferior aspect of the inferior vena cava. •The contrast is injected through a multiple side hole catheter. An IVC Filter is a “wire basket” that is used to trap emboli. Several types available Indications for IVC Filter Existing deep vein thromboses, history of pulmonary embolism. Surgical weight loss. Some cancer patients. anticoagulation therapy is contraindicated. Prolonged bed rest/ immobility. When Venography Rt 255 Spring rev 2010 Week 10 (11)– Mon D. Charman pg 5 IVC Filter Placement therapy contraindicated. •Utilized to trap deadly This Procedure SAVES Lives. Pulmonary Embolism’s RISKS – CAN PUNCTURE! •Filter placed when anticoagulation Use of carbon dioxide (CO2) as a contrast medium is demonstrated (appearing white along the right of the spine) on a frail 75-year-old man. Superior VenaCavogram example Post- Procedure CareApply pressure to puncture site 5-20 min. Patient monitored 6-8 hours in hospital. BEDREST. Watched Minimal for hematoma. activity for the 1st couple of days after discharge. Leg Venography & Other Modalities is nearly 100% sensitive and specific in making this diagnosis (pulmonary embolism is diagnosed in other ways).= HOW? Accuracy is crucial since deep vein thrombosis can lead to pulmonary embolism, a condition that can be fatal. It is especially useful when there is a strong suspicion of deep vein thrombosis, but non-invasive tests (ultrasound) have failed to identify the disease. Doppler U.S. used to determine presence of DVT. MRI & CT can also be used. Fluoroscopy in the Angio suite used for insertion of filters for IVC. Venography is not used often, because it is painful & expensive Venography takes between 30-45 minutes + up to 10 min of beam on – fluoro time May be done in a physician's office, or a hospital. US – Now modality of choice Unless results are inconclusive PROCEDURES DONE w/ US Peripheral Vascular Ultrasound Carotid Ultrasound Upper/Lower Arterial Evaluation Renal Duplex Imaging Upper/Lower Venous Evaluation It VASCULAR ULTRASOUND: non-invasive - no contrast no radiation BENEFITS RISKS Less Expensive ? Non Invasive/Painless (If No Health Problems) Soft Tissue Visualized Tortuous Veins Well Visualized Sometimes Inconclusive or Unclear Has Replaced Venography Vein Is Totally Closed Off Or Not? Capable Of Replacing Angio Someday (?) Unable To See Deep Vessels