Deep vein thrombosis
advertisement

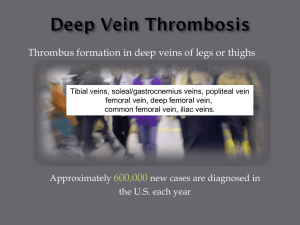
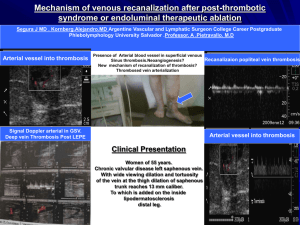
is the formation of a blood clot ("thrombus") in a deep vein. It is a form of thrombophlebitis (inflammation of a vein with clot formation). Deep vein thrombosis commonly affects the leg veins (such as the femoral vein or the popliteal vein) or the deep veins of the pelvis. Occasionally the veins of the arm are affected (if spontaneous, this is known as Paget-Schrötter disease). DVTs occur in about 1 per 1000 persons per year. It is estimated that approximately 350,000 to 600,000 Americans each year suffer from DVT and pulmonary embolism and at least 100,000 deaths may be directly or indirectly related to these diseases. DVT is much less common in the pediatric population. About 1 in 100,000 people under the age of 18 experiences deep vein thrombosis, possibly due to a child's high rate of heart beats per minute, relatively active lifestyle when compared with adults, and fewer comorbidities . Iincluding : *the use of estrogen-containing methods of hormonal contraception, *recent long-haul flying (economy class syndrome),( risk of DVT is higher in travellers who smoke, are obese, or are currently taking contraceptive pills) * intravenous drug use . *a history of miscarriage (which is a feature of several disorders that can also cause thrombosis). Women have an increased risk during pregnancy and in the postnatal period A family history can reveal a hereditary factor in the development of DVT. Approximately 35 percent of DVT patients have at least one hereditary thrombophilia, including deficiencies in the anticoagulation factors protein C, protein S, antithrombin, or mutations in the factor V and prothrombin genes. *The most common risk factors are recent surgery or hospitalization. 40% of these patients did not receive heparin prophylaxis. *Other risk factors include advanced age, obesity, infection, immobilization, tobacco usage *certain inflammatory diseases and specific conditions such as stroke, heart failure or nephrotic syndrome. *Immobilization (such as when orthopedic casts are used). *certain drugs (such as estrogen or erythropoietin) . According to Virchow's triad, venous thrombosis occurs via three mechanisms: 1-decreased flow rate of the blood, 2-damage to the blood vessel wall and 3-an increased tendency of the blood to clot (hypercoagulability). Several medical conditions can lead to DVT, such as compression of the veins, physical trauma, cancer, infections It is recognized that thrombi usually develop first in the calf veins, "growing" in the direction of flow of the vein. DVTs are distinguished as being above or below the popliteal vein. Very extensive DVTs can extend into the iliac veins or the inferior vena cava. The risk of pulmonary embolism is higher in the presence of more extensive clots There may be no symptoms referable to the location of the DVT, but the classical symptoms of DVT include pain, swelling and redness of the leg and dilation of the surface veins. In up to 25% of all hospitalized patients, there may be some form of DVT, which often remains clinically inapparent (unless pulmonary embolism develops). There are several techniques during physical examination to increase the detection of DVT, such as measuring the circumference of the affected and the contralateral limb at a fixed point (to objectivate edema), and palpating the venous tract, which is often tender. Physical examination is unreliable for excluding the diagnosis of deep vein thrombosis the leg is pale and cool with a diminished arterial pulse due to spasm. It usually results from acute occlusion of the iliac and femoral veins due to DVT. there is an acute and nearly total venous occlusion of the entire extremity outflow, including the iliac and femoral veins. The leg is usually painful, cyanosed and oedematous. Venous gangrene may supervene. It is vital that the possibility of pulmonary embolism be included in the history, as this may warrant further investigation . I-Physical examination: Homans' test: Dorsiflexion of foot elicits pain in posterior calf. However, it must be noted that it is of little diagnostic value and is theoretically dangerous because of the possibility of dislodgement of loose clot. Pratt's sign: Squeezing of posterior calf elicits pain. However, these medical signs do not perform well and are not included in clinical prediction rules that combine best findings in order to diagnose DVT. Active cancer (treatment within last 6 months or palliative) -- 1 point Calf swelling >3 cm compared to other calf (measured 10 cm below tibial tuberosity) -- 1 point Collateral superficial veins (non-varicose) -- 1 point Pitting edema (confined to symptomatic leg) -- 1 point Swelling of entire leg - 1 point Localized pain along distribution of deep venous system— 1 point Paralysis, paresis, or recent cast immobilization of lower extremities—1 point Recently bedridden > 3 days, or major surgery requiring regional or general anesthetic in past 4 weeks—1 point Alternative diagnosis at least as likely—Subtract 2 points Score of 2 or higher - deep vein thrombosis is likely. Consider imaging the leg veins. Score of less than 2 deep vein thrombosis is unlikely. Consider blood test such as d-dimer test to further rule out deep vein thrombosis. II- intravenous venography, which involves injecting a peripheral vein of the affected limb with a contrast agent and taking X-rays, to reveal whether the venous supply has been obstructed. Because of its invasiveness, this test is rarely performed. D-dimer In a low-probability situation, current practice is to commence investigations by testing for D-dimer levels. This cross-linked fibrin degradation product is an indication that thrombosis is occurring, and that the blood clot is being dissolved by plasmin. A low Ddimer level should prompt other possible diagnoses (such as a ruptured Baker's cyst, if the patient is at sufficiently low clinical probability of DVT. Other blood tests : Other blood tests usually performed at this point are: complete blood count Primary coagulation studies: PT, APTT, Fibrinogen liver enzymes renal function and electrolytes . Impedance plethysmography, Doppler ultrasonography, compression ultrasound scanning of the leg veins, combined with duplex measurements (to determine blood flow), can reveal a blood clot and its extent (i.e. whether it is below or above the knee). Duplex Ultrasonography,due to its high sensitivity, specificity and reproducibility, has replaced venography as the most widely used test in the evaluation of the disease. This test involves both a B mode image and Doppler flow analysis. 1-The most serious complication of a DVT is that the clot could dislodge and travel to the lungs, which is called a pulmonary embolism (PE). DVT is a medical emergency, present in the lower extremity there is 3% chance of a PE killing the patient 2- A late complication of DVT is the post-phlebitic syndrome, which can manifest itself as edema, pain or discomfort and skin problems. Therapy: Treatment at home is an option . Hospitalization should be considered in patients with more than two of the following risk factors as these patients may have more risk of complications during treatment: bilateral DVT, renal insufficiency, body weight >70 kg/154 lbs, recent immobility, chronic heart failure, and cancer. Anticoagulation is the usual treatment for DVT. In general, patients are initiated on a brief course (i.e., less than a week) of heparin treatment while they start on a 3- to 6-month course of warfarin (or related vitamin K inhibitors). Low molecular weight heparin (LMWH) is preferred, though unfractionated heparin is given in patients who have a contraindication to LMWH (e.g., renal failure or imminent need for invasive procedure). In patients who have had recurrent DVTs (two or more), anticoagulation is generally "life-long." An abnormal D-dimer level at the end of treatment might signal the need for continued treatment among patients with a first unprovoked proximal deepvein thrombosis Thrombolysis is generally reserved for extensive clot, e.g. an iliofemoral thrombosis. But there may be an increase in serious bleeding complications. Elastic compression stockings should be routinely applied "beginning within 1 month of diagnosis of proximal DVT and continuing for a minimum of 1 year after diagnosis". Starting within one week may be more effective. Most trials used kneehigh stockings. Inferior vena cava filter reduces pulmonary embolism and is an option for patients with an absolute contraindiciation to anticoagulant treatment (e.g., cerebral hemorrhage) or those rare patients who have objectively documented recurrent PEs while on anticoagulation An inferior vena cava filter (also referred to as a Greenfield filter) may prevent pulmonary embolisation of the leg clot. However these filters are themselves potential foci of thrombosis,IVC filters are viewed as a temporizing measure for preventing life-threatening pulmonary embolism. Post-phlebitic syndrome occurs in 15% of patients with deep vein thrombosis (DVT). It presents with leg oedema, pain, nocturnal cramping, venous claudication, skin pigmentation, dermatitis and ulceration (usually on the medial aspect of the lower leg). is advised in many medical and surgical inpatients using anticoagulants, graduated compression stockings (also known as thromboembolic deterrent stockings) or intermittent pneumatic compression devices. Clinical practice guidelines by the American College of Chest Physicians (ACCP) provide recommendations on DVT prophylaxis in hospitalized patient: "In acutely ill medical patients who have been admitted to the hospital with congestive heart failure or severe respiratory disease, or who are confined to bed and have one or more additional risk factors, including active cancer, previous VTE, sepsis, acute neurologic disease, or inflammatory bowel disease, prophylaxis with low-dose unfractionated heparin-LDUH or LMWH is recommended. In patients who have undergone surgery, low molecular weight heparins (LMWH) are routinely administered to prevent thrombosis. LMWH can only currently be administered subcutaneously . Prophylaxis for pregnant women who have a history of thrombosis may be limited to LMWH injections or may not be necessary if their risk factors are mainly temporary. Early and regular ambulation (walking) is a treatment that predates anticoagulants and is still recognized and used today There is clinical evidence to suggest that wearing compression socks or compression tights while travelling also reduces the incidence of thrombosis in people on long haul flights