Trauma Flow Sheet Audit: Performance Improvement Tracking
advertisement

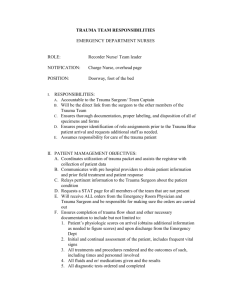
Trauma Flow Sheet Performance Improvement Tracking- January 2008 Objective: Performance Improvement audits of the trauma flow sheet will be done on a weekly basis to ensure accurate and complete written documentation. All missing documentation will be followed up, completed and signed off within one week of receiving the chart audit tool. Can be signed off for completion by the ED Manager, ED Supervisor, ED Educator or the Trauma Program Manager. Procedure: 1. Complete trauma flow sheet charting. 2. Copy Trauma Flow sheet chart twice. Place one copy in the ED MD dictation slot and the other copy goes with the patient for the inpatient chart. 3. The yellow copy of the flow sheet is placed in the Charge leader box for charges to be completed. The Trauma Registrar is given the yellow copy when charges are completed. 4. When the registrar data is completed, the trauma flow sheet copy will be sent to the Trauma Program Manager. 5. Audits will be conducted per the trauma flow sheet audit form weekly. All monthly stats will be obtained. The copy of the trauma flow sheet and the audit tool will be returned to the primary nurse. The audit form will be dated when returned to the primary nurse. 6. The Primary nurse, within one week, will obtain the chart and complete all missing documentation. 7. When the documentation is completed, the form will be returned to the ED Manager, ED Supervisor, or Trauma Program Manager to be checked for completeness. This requires the chart with the original trauma flow sheet and the audit tool. 8. When checked, the audit form will be signed and returned to Trauma Program Manager. 9. The Trauma Program Manager will trend all charts for accuracy and completeness. Any discrepancies or trends will be shared with the ED Manager. 10. Finally, the original chart will be sent to the chart if the patient is still in-house or to Health Information if the patient has been discharged. Attachment: The trauma flow sheet PI tracking/audit tool TRAUMA FLOW SHEET QA Nurse Recorder________________________________________ Charting Complete YES DOCUMENTATION AUDIT NO YES NO COMMENTS Times- Response includes name of MD, time paged and time responded Trauma Blue / Trauma Consult Activation Time Trauma surgeon Response Neurosurgeon Response Orthopedic surgeon Response Assessment: Primary Assessment: ABCDE Secondary Assessment Vital signs, GCS & RTS Temp, P, RR, B/P, SaO2 ETCO2 if intubated GCS X 2 Revised Trauma Score X 2 Meds, Fluids, I&O Tetanus Status (page one) Given? Input Totaled? Output Totaled? Category of Trauma Response: TB, TC, TA Patient Disposition from ED Date, Time, Place Pain Scale Initial Pain Assessment Subsequent Pain Assessment Date given to the Primary Nurse: ________________ Chart documentation completed Date:_______________ Verified chart completion- Signature of ED Leadership staff or TPM __________________ Date_______________