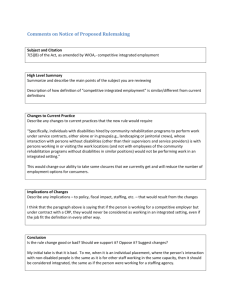
promises kept - Florida Developmental Disabilities Council
advertisement

PROMISES MADE…PROMISES KEPT A Policy Analysis of Public Services Available to Florida Residents with Developmental Disabilities A Report to the Florida Developmental Disabilities Council, Inc. by The University of Miami School of Medicine Mailman Center for Child Development A University Center for Excellence in Developmental Disabilities Education, Research and Service June 2003 FLORIDA DEVELOPMENTAL DISABILITIES COUNCIL, INC. “Sponsored by United States Department of Health and Human Services, Administration on Developmental Disabilities and the Florida Developmental Disabilities Council, Inc.” BACKGROUND ..........................................................................................................................................................4 ACKNOWLEDGEMENTS .........................................................................................................................................5 PART ONE ANALYSIS OF SERVICES INTRODUCTION.........................................................................................................................................................6 I. SERVICES AVAILABLE TO CHILDREN ..........................................................................................................8 THE DEPARTMENT OF HEALTH ..................................................................................................................... 8 THE DEPARTMENT OF CHILDREN AND FAMILIES........................................................................................... 12 THE DEPARTMENT OF EDUCATION .............................................................................................................. 13 SERVICES TO CHILDREN IN OTHER SETTINGS ............................................................................................. 17 AND ANOTHER 12% OR 1269 SHOWED SIGNIFICANT DEFICITS, WHICH SUGGESTED A DEVELOPMENTAL DISABILITY. IN 2001-02, 78 CHILDREN WITH LOW INTELLECTUAL FUNCTIONING WERE PLACED IN SPECIALIZED RESIDENTIAL PROGRAMS, AS A RESULT OF MULTIDISCIPLINARY PLACEMENT STAFFING. SERVICES AVAILABLE TO THESE YOUTH INCLUDE CASE MANAGEMENT SERVICES, BEHAVIOR MODIFICATION, COUNSELING, MENTAL HEALTH SERVICES, SOCIAL SKILLS ENHANCEMENT, PRE-VOCATIONAL AND VOCATIONAL SERVICES, HEALTH SERVICES AND FAMILY INTERVENTION. CONTRACTED PROFESSIONALS PROVIDE THESE SERVICES IN THE RESIDENTIAL TREATMENT COMMITMENT PROGRAMS. ....................................................................................................... 18 SUMMARY OF SERVICES AVAILABLE TO CHILDREN ...................................................................................... 18 POTENTIAL OBSTACLES TO SERVICES FOR CHILDREN. ................................................................................ 18 II. SERVICES FOR CHILDREN TRANSITIONING FROM SCHOOL ............................................................. 19 TRANSITION RESOURCES ........................................................................................................................... 20 HEALTH CARE ........................................................................................................................................... 20 ADULTS WITH SPECIAL HEALTH CARE NEEDS. YET, MEDICAL PROFESSIONALS RECOGNIZE THAT ACCESS TO QUALITY HEALTH CARE FOR CHILDREN IN THIS POPULATION IS CRITICAL FOR A SUCCESSFUL TRANSITION FROM DEPENDENCE TO INDEPENDENCE. FAMILIES OF CSHCNS ALSO REPORT SERIOUS DIFFICULTIES IN FINDING DENTISTS TO CARE FOR THEIR CHILDREN. THIS ISSUE BECOMES MORE PROMINENT DURING THE TRANSITION YEARS....................................................................................................................................................... 21 DENTAL SERVICES..................................................................................................................................... 21 EDUCATIONAL SERVICES ........................................................................................................................... 21 DIVISION OF VOCATION REHABILITATION (DVR). ......................................................................................... 23 ASSISTIVE TECHNOLOGY ........................................................................................................................... 25 DEVELOPMENTAL DISABILITIES PROGRAM (DDP)........................................................................................ 27 SUMMARY OF TRANSITION SERVICES.......................................................................................................... 27 POTENTIAL OBSTACLES TO SERVICES ........................................................................................................ 27 III. SERVICES FOR ADULTS............................................................................................................................... 28 A. HEALTH CARE SERVICES ...................................................................................................................... 29 THE DEPARTMENT OF HEALTH (DOH) ........................................................................................................ 30 THE DEVELOPMENTAL DISABILITIES PROGRAM (DDP)................................................................................. 31 DEVELOPMENTAL SERVICES HOME AND COMMUNITY BASED SERVICES W AIVER. ......................................... 34 FUNDING AND INDIVIDUALS SERVED IN 2001-02 .......................................................................................... 36 SERVICES PROVIDED ................................................................................................................................. 38 SERVICES PROVIDED. ................................................................................................................................ 40 RESIDENTIAL SERVICES ............................................................................................................................. 41 2 SERVICES PROVIDED/RESIDENTIAL TRENDS ............................................................................................... 43 C. EMPLOYMENT AND DAY ACTIVITY SERVICES .......................................................................................... 48 SERVICES PROVIDED/EMPLOYMENT TRENDS .............................................................................................. 49 DVR SERVICES ......................................................................................................................................... 50 SERVICES PROVIDED. ................................................................................................................................ 52 D. TRANSPORTATION SERVICES ................................................................................................................ 54 W AIVER TRANSPORTATION SERVICES PROVIDED ........................................................................................ 56 COMMUNITY AND FAMILY SUPPORTS .......................................................................................................... 58 POTENTIAL OBSTACLES TO SERVICES FOR ADULTS ..................................................................................... 60 IV. SERVICES FOR OLDER ADULTS ................................................................................................................ 61 OLDER ADULTS WITH DEVELOPMENTAL DISABILITIES .................................................................................. 61 A. HEALTH CARE SERVICES ...................................................................................................................... 62 B. RESIDENTIAL SERVICES ........................................................................................................................ 63 C. DAY ACTIVITIES.................................................................................................................................... 64 DOEA SERVICES PROVIDED ...................................................................................................................... 67 D. TRANSPORTATION SERVICES ................................................................................................................ 67 SERVICES PROVIDED ................................................................................................................................. 67 POTENTIAL OBSTACLES TO SERVICES ........................................................................................................ 67 PART TWO CONCLUSIONS AND RECOMMENDATIONS I. INTRODUCTION ................................................................................................................................................... 68 II. GENERAL RESPONSES TO FOCUS GROUPS AND SURVEYS .............................................................. 70 III. SPECIFIC RESPONSES FROM FOCUS GROUPS AND SURVEYS ...................................................... 73 IV. CONCLUSIONS AND RECOMMENDATIONS FROM THIS STUDY ........................................................ 77 V. EMERGING NATIONAL TRENDS AND THEIR IMPACT IN FLORIDA ..................................................... 83 REFERENCES USED IN THIS REPORT ............................................................................................................. 88 3 Promises Made…Promises Kept PA R T O N E A NALYSIS OF S ERVICES BACKGROUND Only in recent years have better funding streams, new legislation and improved public attitudes fostered the enhancement of services for people with severe and long-term disabilities around the country. Like most states, over the last decade Florida has been moving steadily towards the goal of providing individuals with developmental disabilities the services they need within their own homes and communities. Part of this effort entails moving individuals out of large institutions. Four state developmental service institutions (DSI) remain in Florida, though one is being phased down and is scheduled for closure. Residents of private intermediate care facilities (ICF/DD) also have the option of receiving services in home and community-based settings. With a more aggressive pursuit of Medicaid Waiver funds, the State of Florida has nearly doubled (a 94% increase) the amount of money spent on services for individuals with developmental disabilities over the last several years, from $503M for 1988-89 to a total of $975M in 2002-03. (This compares to an average U.S. increase of about 14% during the same four-year period.) The number of people served in Florida also increased during the same time period from a total of 9219 to more than 26,000 (a 182% increase). The need continues to grow exponentially. Even as the latest budget request was being formulated to include services to those remaining on an initial waiting list of 10,000 people, a second and larger group of 10,000 individuals surfaced and now also awaits services. Responding to the urgent demands of consumers, families and disability advocates—as well as recognition of the need by administrators and legislators—the Developmental Disabilities Program is currently in the throes of a complete re-design. Guided by a representative group of the aforementioned stakeholders, the aim is that the revamped system will better provide the service flexibility and choices required by individuals and their families. Within this evolving environment of expanded expectations, the Florida Developmental Disabilities Council, Inc. contracted the Mailman Center -- a University Center of Excellence in Developmental Disabilities (UCEDD)-- at the University of Miami to conduct a policy analysis and review of public services available to Floridians with disabilities. 4 ACKNOWLEDGEMENTS In preparing this report, data was gathered from Florida departments and offices that provide social services to all residents. These include: Department of Children and Families/Developmental Disabilities Program (DDP); Department of Education; Department of Health; Department of Children and Families/Alcohol, Drugs and Mental Health Program; Department of Education/Vocational Rehabilitation Program; Office of Disadvantaged Transportation; Department of Elder Affairs; and, The Medicaid Office, within the Agency for Health Care Administration. We would like to thank the employees in these offices who patiently provided assistance in obtaining the data and information requested. Important input was also provided by consumers, families and service providers who participated in a series of focus groups held around the state, as well as in written surveys that were distributed at disability conferences and meetings. To these individuals who took the time to share their opinions and perspectives, we are also grateful. Much of the descriptive and statistical information contained in this report was gleaned from direct contact with relevant agency staff or from Florida’s public information web sites, including some of the wide variety of reports and publications listed at the end of this report. Project Consultants who contributed to this report include: Rae Alfassa-White, M.S. Linda Friedman, M.S.W. Martha Sheldon, M.S.W. Grateful appreciation is also extended to the organizations whose kind cooperation made the project’s focus groups possible: District Seven Family Care Council People First, South Florida Chapter Florida Association of Support Coordinators, Jacksonville area. ………………………….. Daniel Armstrong, Ph.D., Director of the Mailman Center Jean Sherman, Ed.D., R.N., Author 5 INTRODUCTION Florida is a state populated by more than 16 million people. The latest update of the 2000 census contains the following information about people with disabilities who do not live in institutions. For ages 6-20 there are 284,514 individuals; there are 1,914,507 individuals between ages 21-64; and, the over 65 age group holds 1,075,545 people. All told, there are more than 3.2 million Floridians with some sort of disability. Within this population there is a group of people whose lifelong or developmental disabilities are sufficiently severe that they require ongoing services and support. The range of needed services will likely vary throughout the individuals’ lifetimes and some supports may be provided by the voluntary sector, primarily by families. However, the vast majority of these individuals’ service needs must be filled by the public sector. The total number of Floridians with severe developmental disabilities is 240,000. The number of persons who will need services from the Developmental Disabilities Program is approximately 80,000. The number of Floridians with developmental disabilities. Several factors confound attempts to estimate the number of Floridians with developmental disabilities who need services from the system. These include: 1) the total state population of people with developmental disabilities can be obtained by using research-based formulas. However, this total is different from the number of people whose severity of disability causes/will cause them to seek services. A study by Larson and colleagues (2001) may be helpful in interpreting these estimates. Using data from this complex study of methods, ages, definitions and population surveys, they determined that an accurate, combined prevalence rate of mental retardation and developmental disabilities in the non-institutionalized U.S. population is 1.49%. 2) The ESE school population cannot be used to project a number, since not all children with developmental disabilities are clearly identified and, of the total number of students with retardation, some portion will “age out” or increase their IQ scores by graduation and thus become ineligible for services. 3) The DDP currently uses the number of known individuals as a prevalence number, but that does not take into account people who are currently not being served, for whatever reason. 4) Some large states (e.g., Texas) estimate the prevalence of one unknown person with a disability needing service for each one that is known. 5) Reluctance of some individuals with unresolved immigration status 6 to attempt to access services may also result in underestimates of the number in need of services. Since they produce approximately the same results, two of these approaches can be useful for planning purposes. First, using a 1.49% prevalence rate (or approximately 1.5%) in the state population of 16 million produces an estimate of about 240,000 Floridians with developmental disabilities. Based on their breadth of experience, the consulting group, Mercer reports that approximately 1 in 3 persons in the actual population comes forward for services. From a population of 240,000 that means a service population of approximately 80,000. Second, assuming the existence of one person unknown for every person known (41,000) to have a severe developmental disability produces a number of approximately 82,000 persons who need or will need services. This is nearly double the current number of people with severe developmental disabilities who are being served or who have requested services in Florida. Tracking People with Developmental Disabilities in the Health and Social Service System. Determining the number of people with developmental disabilities who are served by state programs other than the DDP is not entirely possible, given the current reporting systems in place. Some departments (DOH, TD) track general “disabilities” in the individuals they serve; others do not. Some departments (DOE, DOEA) do track their clients by specific disability, but use functional categories rather than a classification. These functional categories are more encompassing than a developmental impairment and so, cannot be used as an equivalent. Still other agencies (DVR) may use the term “developmental disability,” but interpret it more narrowly to mean clients who have cognitive impairments only. Other clients who have the developmental impairments of cerebral palsy and spina bifida are grouped into another category with all other clients who have “orthopedic impairments.” Limitations of the Findings. Any examination of the service data presented in this report must be viewed within the framework of the reporting disparities just described, and with an understanding of the lack of any interagency accountability for citizens with developmental disabilities. That said, the service data presented in this report serves as a foundation for identifying: 1) certain service trends, 2) barriers to service use and, 3) specific recommendations for enhanced quality, access and availability. These recommendations derive from reviews of existing service policies and eligibility criteria, as well as from the observations and experiences of those who use the services, either as recipients or as providers. 7 Contents of the Report. This report is presented in two parts. Part One illustrates the data findings, both quantitative and qualitative. Because people with developmental disabilities typically require services and supports across their life spans, Part One looks at services for four chronological age groups: infants and children, adolescents in transition, adults, and old adults. Within each section, the appropriate services are discussed and data supplied for the services given. Each section also provides typical consumer profiles and names some service barriers. These barriers are further elaborated in Part Two of the report. Part Two contains the qualitative input of participants in three focus groups and of survey respondents from around the state. Conclusions and recommendations are then presented. The conclusions result from an analysis of the service data collected, and include trends discovered. The recommendations in this report evolved from the study’s conclusions; some are expressed in the words of survey or focus group participants. I. SERVICES AVAI LAB LE TO CHILDREN Of the total population of schoolaged children in Florida, estimates of those with special health care needs, and at least one chronic condition, range from 5 percent to more than 30 percent. Approximately 6 to 15 percent of the state’s children with special health care needs are served with exceptional education programs. Of 2,500,161 students in 2001, 15 percent (376,074) had a special need, not counting gifted students. Subtracting students with specific learning disabilities and speech impairments, 6 % of Florida’s students or 150,142 school-aged children have more severe disabilities and special health care needs. Within the State of Florida, there are several departments and offices concerned with providing services to children with developmental disabilities, from their early childhoods through high school graduations and their transitions from school. The primary entities providing childhood services include the Departments of Health (DOH) and Education (DOE) and, indirectly, the Medicaid Office of AHCA. The respective roles of these entities are detailed below. Health Care. According to the 2002 report, The Health of Florida’s Children and Youth, providing preventive, primary and specialty services for children with special health care needs is a core public health function for DOH. Children with these special needs also receive educational services from DOH from ages 0-3; school aged children receive educational services from DOE. According to the 2002 report, The Health of Florida’s Children and Youth, poverty, a lack of insurance or rural location place a family with a child with a disability and chronic condition at greater risk. Children with special health care needs are also at increased risk for child abuse and neglect, when compared to the general population. THE DEPARTMENT OF HEALTH Within the Department of Health, the Division of Children’s Medical Services (CMS) is the most significant service entity for children with developmental disabilities. CMS serves 77 percent of all children in Florida who are enrolled in publicly supported health insurance programs. The CMS program provides children with special health 8 care needs with a family centered, managed system of care. Children with special health care needs are those children under age 21 whose serious or chronic physical or developmental conditions require extensive preventive and maintenance care, beyond that required by typically healthy children. During 2001-02, CMS served over 155,000 children with special health care needs. Families are usually required to pay a monthly insurance premium of $15, but there is no cost for services. Most services are provided at or coordinated through CMS offices in 22 local communities throughout the state. When necessary, children are referred to CMS-affiliated medical centers. These centers provide many specialty programs with follow-up care provided at local CMS offices. In some rural areas of the state, county health departments provide primary care services and conduct the prevention activities. To enhance access to specialty care in rural areas, CMS implemented a specialists’ telemedicine initiative through the University of Florida. CMS has two main divisions: Prevention and Intervention (EI) and The Network. The scope of Prevention and Intervention includes the Child Protection Team, the Early Intervention and Prevention System and, Regionalized Perinatal Intensive Care. The Network is a statewide healthcare delivery system for children 021 years old with chronic or physical or developmental conditions. The CMS Network provides a Medicaid Plus benefit package, which includes primary care, specialty care, hospitalization, dental services, mental health services, pharmaceuticals, transportation, home health care, therapy services, care coordination by specially trained nurses, social services, health education, family counseling and community resource linkages. The Network is also authorized to provide early intervention services, parent support, respite, and genetic and nutritional counseling to the children enrolled. It is recognized as a Medicaid managed care option and a KidCare (the State Children’s Health Insurance Program - SCHIP) program through federal Medicaid waivers and state plan amendments. As of 10/02 the Behavioral Health Network was serving 329 children with severe emotional disturbances and substance related disorders; another 79 were waiting. Other available aspects of The Network include a Behavioral Health Network, a Children’s Multidisciplinary Assessment Team (CMAT) and Medical Foster Care. Behavioral services include both mental health and substance abuse services. Program Eligibility. To be eligible for the CMS Network, children must meet both financial and medical requirements. They must have special health care needs that require medical services, therapies, supplies or equipment due to a chronic physical, behavioral or developmental condition. These children often need complex care requiring multiple providers, rehabilitation services and specialized equipment, in a number of different settings. 9 Children must also be financially eligible by being either a Medicaid recipient, a Florida KidCare enrollee under 19 years old, or a member of a family that meets certain financial criteria. Three categories of children are served: 1) those covered by Medicaid (Title XIX -71%); 2) those covered by SCHIP (Title XXI - 13%); and, 3) those not covered by either of those two funding sources (16%). This latter category is referred to as the Safety Net program. NOTE: A capped amount of funding is available for participants in the safety net program, and medically necessary services are provided until age 21, to the extent that resources continue to exist. For the period of July 1, 2001 – June 30, 2002, a total of 54,173 children were enrolled in the CMS Network via one of the three funding categories. It should be noted, however, that disability data are not collected by type for children served through The Network. Therefore these 54,173 enrollees are not necessarily all children with developmental disabilities. They are children with special health care needs (CSHCNs), some of which may include developmental disabilities. An Increase in Enrollment. Enrollment in the CMS Title XXI program is on the increase. In March 2002 it was 7051; by March 2003 it was 8622. The following graph displays the enrollment trends in the three main funding sources/categories of the CMS Network. CMS Enrollment Trend Statewide Title XIX, XXI, and Safety Net FY 01- 02 30,000 Title XIX 25,000 Total Enrollees 20,000 15,000 Title XXI 10,000 5,000 Safety Net Title XIX Title XXI Safety Net The EI Program. In contrast to the Network, the CMS Infants and Toddlers Early Intervention Program (EI) specifically serves children with developmental disabilities. The $39.7 M program has two 10 Jun-02 May-02 Apr-02 Mar-02 Feb-02 Jan-02 Dec-01 Nov-01 Oct-01 Sep-01 Aug-01 Jul-01 0 components: early intervention and infant metabolic screening, which identifies infants with potential developmental disabilities, due to inborn errors of metabolism. Early Intervention (PART C) provides entitled services to children who have a developmental disability or an established medical condition that has a likelihood of resulting in a developmental delay. The CMS “EI” program is an umbrella program with three components: IDEA, Part C; Developmental Evaluation and Intervention; and, the Developmental Disabilities Program. The eligibility criteria for participation in each of these programs consist of the following: 1) IDEA, Part C – Infants and toddlers who have been diagnosed with an established condition associated with developmental delay (metabolic/genetic disorder, neurological disorder, severe sensory impairment, or a severe attachment disorder, such as Autism Spectrum Disorder) and those who have a developmental delay. A developmental delay is said to be present when an appropriate evaluation/assessment or informed clinical opinion shows a delay in at least one of the following areas: 1) Cognition; 2) Physical/motor; 3) Communication; 4) Social/emotional; or 5) Adaptive development. Such delay must be of 1.50 standard deviation for greater below the mean or 25% delay or greater in term of months of age. Eligibility is from birth to the child’s third birthday; services are provided regardless of family income. This program does not serve the at-risk population of infants and toddlers, but only those who have been diagnosed with a developmental delay. 2) Developmental Evaluation and Intervention Program (DEI) - DEI is a coordination of services program intended to enhance a family’s ability to maximize their child’s potential when there is a high risk of developmental disabilities. The DEI program provides comprehensive assessments of the needs of infants born or transferred into a DEI designated hospital and served in the neonatal intensive care unit (NICU) for five or more days. It also serves infants identified as hearing impaired or at high risk of hearing impairment and infants who have been referred by the CMS Genetics/Screening Program. Infants identified in the NICU must meet medical and family income eligibility criteria to receive services under this program component. Services provided include evaluations and assessments, service coordination, referrals for parent support and training services, and periodic evaluations after hospital discharge. DEI also includes the Infant Hearing Impairment Program, a program component that provides infant hearing services to maximize the developmental potential of infants with impaired hearing. These services are provided for infants born or served in a DEI designated hospital, regardless of the family’s income. Services include the provision of audiometric screening, diagnosis 11 and referral services to those infants identified as a high risk for hearing loss. Services provided under this program component are coordinated with the local school districts that provide for the educational management of children with hearing impairments. 3) Developmental Disabilities Program – This Program provides services authorized under Chapter 393, Florida Statutes, only for infants and toddlers who meet eligibility criteria established under the Infants and Toddlers EI Program (Part C). Again, these children must be diagnosed with a developmental delay or an established condition that places them at high risk for a developmental delay. NOTE: This is the only program in the Department of Health that specifically serves individuals with developmental disabilities. Evaluation. The Institute for Child Health Policy conducts an annual evaluation of the Florida KidCare Program, which includes CMS, for the Agency for Health Care Administration. The latest evaluation covers the time period of July 1, 2001 through June 30, 2002 and reviews families’ participation and satisfaction with the various components of KidCare. Overall, as in the prior year, a significantly higher percentage of CSHCNs remained enrolled in CMS (77%) when compared with those children who remained enrolled in other parts of the KidCare program (71%). The report concludes that it is possible that parents who do not perceive their children to have special health care needs are more likely to disenroll from the program. It is also possible that some children’s health improved and they no longer need the program. A certain percentage of these families may also have moved from the state. THE DEPARTMENT OF CHILDREN AND FAMILIES Mental Health Services. The Alcohol, Drug Abuse and Mental Health (ADM) program provides subcontracted mental health services to children who have been diagnosed as Severely Emotionally Disturbed (SED), Emotionally Disturbed (ED) or are at risk of ED. During the fiscal year 2001-02, with a budget of $294 Million, a total of 77,803 children were served. These include: SED = 48,785 ED = 25,667 At risk = 3,351 77,803 Under this program, children are able to receive services and remain in the community. Last year, SED children spent an average of 347 days per year in the community and were in school 90% of the time. ED children spent an average of 358 days in the community and were in school 93% of the time. 12 THE DEPARTMENT OF EDUCATION Health Care - Once a child reaches school age, any occupational, physical and speech therapies, that are specifically designed to augment a child’s educational experience, are provided by local school districts in conjunction with the CMS Network. Though the Department of Education is required by statute to provide medical services to these children, the range, number and availability of services can vary across school districts. When shortages of services, e.g., therapies, exist in certain geographic areas, service delivery may be inadequate in those locales. Provision of health care services to school-aged children is through the Medicaid Certified School Match Program. This program is a reimbursement to schools for services to Medicaid eligible students under the age of 21, who are covered under IDEA (Individuals with Disabilities Education Act). These “medically necessary” services are provided or arranged by school districts, which are responsible for ensuring that students with disabilities receive all services necessary for a free and appropriate public education, including health services. All school districts participate in the school match program, though not all provide services each year. In 2001, 41 of 68 districts provided services to students; with great variation in the amount of services provided. Medicaid services most frequently provided are the various therapies (Physical, Occupational, Speech), nursing services, mental health using a psychologist and mental health using a social worker. Transportation to an off-site provider is also offered by a number of districts. The county health department, other public health entities, or contracted Medicaid community providers may deliver these health services. School districts may also enroll to become Medicaid providers themselves. Districts may use some or all or these alternatives. However, they retain the final responsibility for providing necessary health care to all students with disabilities. Health services that may be provided include mental health services (psychological evaluations, behavioral evaluations, functional behavioral assessments, consultation, development of evaluative reports, coordination of services with other agencies, therapy, counseling, crisis intervention and other treatments/interventions related to behavioral services). Other services often provided are occupational/physical and speech/language therapies. All services that a student receives must be specifically designated on the child’s Individual Education Plan (IEP). Educational Services – The federal Individuals with Disabilities Education Act (IDEA) was passed in 1990 and reauthorized in 1997. It replaced the earlier P.L. 94-142, and mandates that all children with disabilities receive appropriate educations in the least restrictive 13 environments. In Florida, the educational programs and services for children with special learning needs is the Exceptional Student Education (ESE) program, sometimes also referred to more generically as “special education.” For the school year 2001-02, there were 376,074 children served in the ESE program, excluding those considered “gifted.” This represents 15% of the state’s public school student population of 2,500,161 for this year. Within the DOE, the Bureau of Instructional Support and Community Services supports the 67 Florida school districts and their ESE programs. Districts and schools develop their own programs to serve their students in the most effective way possible, while the Bureau provides training and technical assistance to school staff and district administrators, gives information on relevant state and federal laws pertaining to ESE, monitors compliance with those laws, and helps resolve conflicts between school districts and families of ESE students. The appeals of district due process hearings are made to the Bureau. In addition, the Bureau’s Clearinghouse Information Center provides disability materials to parents, as well as information about the rights, processes and activities involved in ESE. Parental involvement and parent/professional collaboration are encouraged throughout. The State Department of Education does not use the term “developmental disability” when identifying a child’s impairment. Rather, the DOE uses 18 different categories or groups to describe the type and level of disability and suggest the degree of assistance that students in each category may need. For example, children with mental retardation may be classified as Educable Mentally Handicapped (EMH – mild impairment), Trainable Mentally Handicapped (TMH – moderate or severe impairment) or Profoundly Mentally Handicapped (PMH - profound impairment). All ESE categories, and the number of children served in each group last year, are listed in the accompanying box. [NOTE: These categories and the DOE descriptions in this section are not in “people first” language. The terminology used by DOE is derived from education statutes.] EMH 29,546 TMH 8,809 PMH 3,025 Orthopedically Impaired (OI) 4,934 Speech Impaired (SI) 55,486 Language impaired (LI) 34,389 Deaf or Hard of Hearing (DEAF) 3,628 Visually Impaired (VI) 1,330 Emotionally Handicapped (EH) 30,598 Specific Learning Disabled (SLD) 70,416 Hospital/Homebound (HH) 2,569 Dual Sensory Impaired (DSI) 72 Autistic 5,293 Severely Emotionally Disturbed (SED) 7,183 Traumatic Brain Injured (TBI) 495 Developmentally Delayed (DD) 10,162 Established Conditions (EC) 159 Other Health Impaired (OHI) 7,980 Total 376,074 14 According to the DOE 2002 SEA Profile, within the ESE Program the most commonly occurring student disabilities are SLD – 45%, EH/SED – 10%, SI – 15% and EMH – 8%. The table below reflects the percent of each disability within the total student population. Disability Type SLD EH/SED SI EMH All Disabilities 45% 10% 15% 8% All Students 7% 2% 2% 1% Available supports. The particular supports available to ESE students fall into three categories: supplemental aids and services, special education services and related services. Supplemental aids and services are aids, services and supports provided in general education classes (or other educational settings) to enable a student to be educated with non-disabled peers. Services may also include special accommodations. This category of supports might include such things as a personal care aide, a note taker, a voice-activated computer and other assistive technology devices. Note: Recently, certain concerns have been addressed to the Advocacy Center for Persons with disabilities regarding DOE’s Certifying the Educational Relevance of Therapies (CERT) profile chart. This tool gives schools the authority to deny occupational and physical therapy to DD and MH students, if any of the following professional documentation exists: “Student is progressing as well in this area as in other areas of development. Developmental age, physical limitation or cognitive ability limits student’s improvement.” or “Student requires totals assistance by staff.” or, “Student’s functioning in the area remains unchanged, despite multiple efforts by the therapist to remediate the concerns or to assist the student in compensating.” Special education services are specially designed instruction and/or interventions to meet the unique needs of the student, such as a special resource class. Related services are those services that the student requires to benefit from ESE, such as counseling, therapies, social work services, etc. For the 2001-02 year, the estimated funding for ESE statewide was more than $3.2 billion. This includes legislative appropriations through the Florida Education Finance Program, as well as $362.4 million in federal dollars through IDEA. Classes are available from prekindergarten through grade 12; ESE students may attend school until they graduate or they reach age 21. An Example of Exceptional Student Education – Mentally Handicapped. During the 2001-02 school year, public schools in Florida were serving 41,380 mentally handicapped students aged 21 and younger. The numbers of children with these disabilitiesranged from 21 in Glades County to 4696 in Miami-Dade County. According to DOE, a “mental handicap” is defined as significantly sub-average general intellectual functioning existing concurrently with deficits in adaptive behavior and manifested during the developmental period. Mentally handicapped students are classified as: 1) educable mentally handicapped or mildly impaired in intellectual and adaptive behavior, with development that reflects a reduced rate of learning; 2) trainable mentally 15 handicapped or moderately/severely impaired in intellectual and adaptive behavior, with development that reflects a reduced rate of learning; and, 3) profoundly mentally handicapped or profoundly impaired in intellectual and adaptive behavior, with development that reflects a reduced rate of learning. Students may be classified as eligible for participation in a mentally handicapped program on the basis of their performance on standardized tests designed to measure their intelligence. However, regardless of the student’s measured level of intelligence, he/she can only be classified as mentally handicapped if, in addition to exhibiting a qualifying level of intelligence, his/her assessed adaptive behavior falls below that of other students in the same age and socio-cultural group. State Board of Education rules identify three sub groups of mentally handicapped children that are differentiated on the basis of student performance on standardized intelligence testing. These groups include: The measured intelligence of an educable mentally handicapped student generally falls between two and three standard deviations below the mean for the test instrument used; The measured intelligence of a trainable mentally handicapped student generally falls between three and five standard deviations below the mean for the test instrument used; and, The measured intelligence of a profoundly mentally handicapped student generally falls below five standard deviations below the mean for the test instrument used. Teachers, counselors and school administrators must first rule out the possibility that a sensory or communication deficit is the cause of lowered intellectual or adaptive functioning. Before a referral can be made for an evaluation of a mental handicap, the district must first screen the child’s vision, hearing, speech and language abilities. A student is eligible for a special program for the mentally handicapped if there is evidence that the student’s measured level of general intellectual functioning is two or more standard deviations below the mean; the assessed level of adaptive behavior is below that of other students of the same age and socio-cultural group; and, the student’s demonstrated level of performance in academic, pre-academic or developmental achievement is sub-average. Furthermore, if the child has been enrolled in basic education programs for more than six weeks, the school must take other measures to address the child’s learning problem. These include: Conducting two or more conferences of parents, teachers, counselors and school administrators concerning the student’s specific problem; Developing anecdotal records or behavioral observations that cite the specific behaviors indicating a need for referral, with the observations made by more than one person in more than one situation; Conducting a minimum of two interventions or adjustments (in the schedule, teacher or instructional technique) for the student; Reviewing social, psychological, medical and achievement data in the student’s educational records; and, Reviewing the student’s attendance records and, where appropriate, investigating reasons for excessive absenteeism. 16 The minimum evaluation for all three categories of mentally handicapped students must include a standardized individual test of intellectual functioning, individually administered by a professional person qualified in accordance with the state Board of Education rules; a standardized assessment of adaptive behavior; an individually administered standardized test of academic or pre-academic achievement; a social development history compiled directly from information provided by the parent, guardian or primary caregiver; and, in addition, for children being considered for a program of profoundly mentally handicapped students, a report of a medical evaluation by a licensed physician may be required by the school district. Students eligible for and enrolled in a special program for the mentally handicapped may continue to participate in that program until dismissal from the program. Such dismissal will be based on criteria contained in the district’s Special Programs and Procedures for Exceptional Students, as required by the State Board of Education. Transportation. All transportation of students to and from ESE programs is provided by the individual school district. In addition, for 2001-02 the Transportation Disadvantaged Commission reports the provision of transportation statewide to 139,639 children with disabilities (the type of disability is not tracked) and to 69,819 children with disabilities who are also considered to be low-income. While the purposes of trips are not tracked according to riders, overall 28% of TD trips are for medical purposes and 37% are for education/training and/or daycare. Therefore, it can be assumed that a total of 210,000 children were transported for at least one of those purposes. SERVICES TO CHILDREN IN OTHER SETTINGS Children in Foster Care. Children with disabilities who are placed in foster care settings should have continued access to community based services and treatments. However, the official liaison process between the foster care system and the DDP must be initiated and completed by the foster care worker assigned to the individual child. Heavy case loads and staff turnovers can work against the successful completion of this process. As a result, a delay in initiating services or an interruption in service continuation may well occur. The liaison process is further complicated when a child is moved to a new school, where the new teacher does not know the child’s particular needs. Children in the Juvenile Justice System. Children with disabilities who remain in their homes on probation continue to receive services in the same way as before probation. However, children who are placed out of their homes and into detention centers may encounter problems with continuity of health care or services. According to a 1998-99 survey by the Department of Juvenile Justice, 5% or 529 youths were considered to have a developmental disability 17 and another 12% or 1269 showed significant deficits, which suggested a developmental disability. In 2001-02, 78 children with low intellectual functioning were placed in specialized residential programs, as a result of multidisciplinary placement staffing. Services available to these youth include case management services, behavior modification, counseling, mental health services, social skills enhancement, prevocational and vocational services, health services and family intervention. Contracted professionals provide these services in the residential treatment commitment programs. SUMMARY OF SERVICES AVAILABLE TO CHILDREN Within the State of Florida, health and educational services are available to children until they reach age 21. The Department of Health provides preventive, primary and specialty services to children with special health care needs. The Early Intervention program serves infants and toddlers with both health care and educational services. Throughout their school years, managed health care is available via the Children’s Medical Services Network. Behavioral and mental health services are also available, as needed; the latter may be provided through the Department of Children and Families. The Department of Education provides services to children with developmental disabilities from pre-kindergarten through age 21. It also provides therapies and other services to augment a child’s educational experience. There are no waiting lists for public school classes, but the therapies and services an individual child needs are not always available in all schools at all times. POTENTIAL OBSTACLES TO SERVICES FOR CHILDREN. #1) Eligibility for Children’s Medical services (CMS) is financial and medical. Children who do not meet the financial eligibility requirement may find that the services they need (e.g., intensive therapies for children with autism) are not covered under private health insurances. #2) Though school districts are mandated to provide necessary augmentative services, when such services are in short supply in certain areas of the state, the child may not receive them. #3) Certain professional documentation on a student’s CERT profile may unjustly result in the termination of needed therapies. #4) Funding caps (such as limitations on enrollment in KidCare) may preclude access to health care services, particularly for children whose physical disabilities or health care needs are less severe. Recommendations to address these and other gaps and obstacles to services for children, are proposed in Part Two of this report. 18 II. SERVICES FOR CHILDREN TRANSITIONING FROM SCHOOL While the previous section of this report described services available to children throughout their school years, this section focuses on the first major life transition encountered by individuals with disabilities—the time when they graduate from school. Nationally, less than 8% of students with a disability leave school with a job, are enrolled in post-secondary education, are involved in community recreation and leisure activities, or are living in an independent situation – according to Ellen Condon, Transition Project Director at the University of Montana. In fact, those students likely to leave school without the skills and supports necessary to work in the community are those with the most severe disabilities. Poor postschool outcomes are linked to the absence of vocational preparation, poor transition planning and ineffective linkages to adult services and supports, prior to graduation. Condon also notes that, “ A major difficulty in planning for a successful transition from school to adult life for students with ongoing support needs is overcoming the differences in how schools and adult agencies provide services.” Special education is an entitlement, services that a student receives by virtue of his or her disability. On the other hand, the services provided by VR and the DDP are based upon eligibility and availability. Even when a person is deemed eligible, availability (due to a lack of funding or provider capacity) can limit access. This is clear from developmental disabilities programs across the country, where the waiting lists average five years. Further complicating matters, the services available may not fit the needs of the transitioning student. Obtaining and administering services can also be challenging. In the school setting, educational personnel manage and oversee the provision of services. For adults, the tasks of identifying, selecting, applying for and coordinating services, sometimes from a confusing array of agencies, may be left to the graduate and the family during the transition process. Whether a child receives a regular or a special diploma, or a certificate of attendance, leaving the school environment (at the maximum age of 22) constitutes a radical change in everyday life and the attendant services and supports. Whether that change is abrupt and/or has a positive impact on the life of the individual and his or her family depends, to a large degree, upon the amount and quality of transitional planning that was done. A discussion of the public services available to help accomplish transitional planning, as well as the various life areas and supports that generally are considered after graduation follows. 19 TRANSITION RESOURCES Currently there are two publicly funded projects in Florida that specifically provide information to individuals with developmental disabilities and their families about school transitions. These projects include the Family Network on Disabilities’ TILES project, which provides training and information to enable individuals with disabilities, their parents, families, guardians and advocates to participate more effectively with professionals in meeting the vocational, independent living and rehabilitation needs of individuals with disabilities. This Clearwater-based project provides workshops and information about effective transition planning to students, aged 14-22. The second specific project is the Transition Center at the University of Florida in Gainesville. Its purpose is to provide statewide support in transition planning to students with disabilities and their families, educators, agency and community representatives. The Center has a resource library, web site and newsletter. It also provides technical assistance and training workshops to local school districts. Once a child turns 18, problems may arise if the person is not already on Medicaid. If receiving non-Medicaid insurance, he or she may experience dramatic gaps in service upon entering the adult insurance system. Medicaid recipients also experience changes at age 21, when many of the therapies received during the school years will be dramatically decreased. HEALTH CARE Some of the most important changes to affect an individual with a disability occur in the area of health care, since there are differences in coverage between adults and children under the Medicaid State Plan. When an individual reaches age 21, coverage for certain services under the State Plan decreases. The most significant of these changes are: Dental services (as of July 2002) – limited to emergency extractions and abscess treatment to alleviate pain/infections; Durable Medical Equipment (DME) – some services and medical supplies are reimbursable only for individuals under 21 years of age; Hearing services – fittings for hearing aids in both ears require prior authorization when an individual is over age 21; Inpatient hospital services – limited to 45 days per state fiscal year (July 1-June 30); Outpatient hospital services – with some exceptions for certain outpatient surgeries, reimbursement is limited to $1500 per state fiscal year; Prescription drugs – for individuals over age 21, reimbursement is limited to four brand name prescriptions per month; and, Therapies (Physical, Occupational, Speech) – these are generally not available to individuals age 21 and older. Parents of children with special health care needs who received services from CMS during their school years will find obtaining insurance difficult as these youths transition to adulthood. Insurance policies are often unaffordable and seldom cover the broad array of specialty care and prescriptions needed by young 20 adults with special health care needs. Yet, medical professionals recognize that access to quality health care for children in this population is critical for a successful transition from dependence to independence. Families of CSHCNs also report serious difficulties in finding dentists to care for their children. This issue becomes more prominent during the transition years. DENTAL SERVICES The Developmental Services Medicaid Waiver is uniquely designed to serve the needs of individuals with developmental disabilities beyond what is provided under the Medicaid State Plan. Consumers of any age who are enrolled in the Medicaid Waiver are covered for the following dental services: diagnostic, preventive and restorative treatment, extractions and endodontics, periodontal and surgical procedures. The services must prevent or remedy dental problems that would otherwise compromise the person’s health. Routine preventive cleanings may also be provided under the waiver. Adult Medicaid beneficiaries not under the waiver have the alternative of obtaining dental services from one of the 24 Federally Qualified Health Centers (FQHC) located throughout the state. FQHCs charge for dental services on a sliding fee scale, dependent on income. They provide dental services either on-site or through contracts with local dentists. As some children become adults, they may be eligible for medical care coverage under Medicare. However, dental care is not an item that is covered by Medicare. Enrique is a 20-year-old who has cerebral palsy and mild mental retardation. He will be finishing high school year next year and wants to live on his own after leaving school. His older brother has his own apartment and Enrique associates living on his own with being an adult. Living independently with a roommate is part of his transition plan, which also includes a job and attending a community recreation program. Some of the supports and services Enrique needs include supported living coaching and assistive devices for his job. EDUCATIONAL SERVICES The completion of high school is the beginning of adult life. Entitlement to public education ends, students and their families are faced with many options and decisions about the future. Under the federal mandate of IDEA, all children enrolled in an ESE program must receive transition services from their school districts. In Florida, the Department of Education, Vocational Rehabilitation Services, and, where appropriate, the Division of Blind Services are required by law to provide services to students with disabilities. Transition services (also called School-to-Work Transition) are joint, coordinated activities meant to promote successful movement from the world of school to the world of adulthood. Post-school choices that are considered in transition planning include postsecondary education, vocational training, integrated employment, (included supported employment), continuing and adult education (workforce development education, adult general education, GED test preparation, community education), adult services (generally via VR and DDP), independent living (supported living, group home, in-home supports, etc. via DDP) or community participation (recreation, leisure, 21 volunteering, civic and religious organizations). The mechanism for developing transition services is the student’s Individual Education Plan (IEP). Annual team meetings are held to formulate the Transition IEP. Members of the team include the student, parents, ESE teacher and related school staff, as well as relevant community agency personnel. Mentors or prospective employers may also participate. Within the school setting, these transition services must begin at age 14 (or younger if appropriate) and include the following specific, ongoing planning activities: 1) At age 14 and updated annually, develop a statement of the child’s transition needs within the Individual Education Plan (IEP) that focuses on the child’s courses of study; 2) At age 16 (or younger, if determined by the IEP team), a statement of needed transition services including interagency responsibilities or linkages; 3) At age 17, a statement that the child has been informed of his or her rights, that will transfer to the child upon reaching the age of 18 (legal majority). Transition Outcomes. The outcomes to result from transition planning are based upon the student’s needs, preferences and interests and include, as appropriate to the individual: 1) Specially designed instruction (as ESE) 2) Developmental, corrective or other supportive services to assist a student to benefit from ESE (transportation to employment training site, job coaching, mentoring, among others) 3) Community experiences (banking, shopping, social or recreational activities) 4) The development of employment and other post-school adult living objectives (includes registering to vote, renting a home, accessing medical services, etc.) 5) Acquisition of daily living skills (meal preparation, budgeting, home maintenance, bill paying, caring for clothes, grooming, etc.) 6) Functional vocational evaluation Marsha is a 17-year-old with mild cognitive disabilities and a hearing impairment. She has a transition goal of full-time employment upon graduation. The IEP transition team identified the following supports for Marsha: visual cues for the steps of the job, reliance on co-workers to assure safety, monitoring for errors, a flashing light on the telephone, and training to use public transportation. The primary post-school outcome statement is the student’s vision or dream for three to five years after graduation. This is an important component of the IEP process because it identifies the ultimate goal for the student. All other components of the IEP should lead to and support this outcome statement. Representatives of any agencies (VR, DDP, technical centers or other community agencies) that are likely to provide or pay for a needed transition service must be invited to Transition IEP meetings, starting at age 16. When agency representatives are unable to attend a meeting, the school district must take other steps to assure that agency’s participation in the planning process. 22 While appearing straightforward on paper, the Transition process can be a complex undertaking, particularly for students with severe disabilities. Many factors can impact its effectiveness, including the knowledge of the ESE teacher and school staff, the understanding of the process and degree of participation by the student and his/her family, the commitment of the VR and DDP programs to provide services, the existence of waiting lists for publicly funded services in the future, consistency and updating of the IEP from its inception to post school implementation and the existence of appropriate community resources and supports. Diploma Decision. The State of Florida offers students the option of obtaining a standard diploma or a special diploma upon graduation from high school. (Some schools offer a choice between two special diplomas, the second of which involves mastery of competencies related to employment and community living.) The type of diploma that a student receives will determine eligibility for post-school options and is very important. The choice of a diploma is made at the IEP meeting when a student turns 14 – the first transition IEP meeting. ESE students who do not earn a diploma will receive a special certificate of completion. However, this certificate is not a diploma and will not be accepted by vocational schools, community colleges, military recruiters or recognized by employers. Generally, when a student reaches age 16, the school will invite the VR counselor to meet with school personnel and with the IEP team to review the student’s plans and provide consultation and information. The VR counselor and student will meet on a regular basis to discuss vocational choices, plans and progress. DIVISION OF VOCATION REHABILITATION (DVR). The Division of Vocational Rehabilitation is the part of the Department of Education that provides services for eligible individuals with physical or mental impairments to prepare for, secure, retain or regain employment. Eligibility for VR services is based upon the presence of a physical or mental disability and a goal of employment. 1. The physical or mental impairment constitutes or results in a substantial impediment to employment. 2. The individual’s employment outcome can benefit from VR services. 3. The individual requires VR services to prepare for, to get, to keep or to regain employment. An eligibility decision is made within 60 days after the application for services. Individuals receiving either Social Security Disability Income (SSDI) or Supplemental Security Income (SSI) for a disability are eligible for VR services if the goal is to secure employment. 23 In addition to arranging any necessary evaluations, the VR counselor will work with the student to develop an employment plan. Various types of services and supports can be included in this plan to help the individual reach the desired employment outcome, including job placement and job coaching. Medical or psychological treatment may be provided on a short-term basis. Artificial limbs, hearing aids, wheelchairs, rehabilitation workshops, technical or trade school classes, college classes or on-the-job training may also be provided. Based on the disability and the vocational goal, VR also offers several types of services that may be required by the student. These include: Transportation and vehicle modification, whichever is the most economical mode for securing rehabilitation services and occupational goal; Books, occupational tools, equipment and other training materials; Occupational licenses; Rehabilitation technology to assist in evaluation, rehabilitation and employment; Maintenance, to cover additional costs incurred by the rehabilitation process; Interpreter services, telecommunications and other technological aids, and Referrals to appropriate community agencies. Job Placement and Closure. When the individual is ready for employment, the VR counselor assists with finding job openings in the community, including supported employment. (NOTE: If the individual is found ineligible for supported employment under VR, the service may then be provided under the DDP waiver.) The counselor can give ideas and advice on filling out job applications and interviewing for particular jobs. The counselor can also work with an employer to modify the job site and provide assistive devices to meet the individual’s needs. Once the job is secured, the VR counselor will assure that the employer and the individual are satisfied and will also determine whether other services are necessary to maintain the job. After at least 90 days of employment the counselor and individual will determine if further VR services are needed. Once no further services are needed the counselor ends his/her active participation in the process. However, if the individual’s situation should change and require additional assistance to maintain the job, this can be provided without having to reapply to VR. Quality Assurance and Monitoring. During or after the VR process an individual may be asked to complete a consumer satisfaction survey. These surveys are administered annually by Florida State University under contract with the Florida Rehabilitation Council. The federal Rehabilitation Services Administration may also conduct on-site monitoring of the VR program. The 2002 Legislature moved oversight of the DVR program from the Department of Labor and Employment Security to the Department of Education Services Provided. During FY2001-02 VR placed a total of 8579 24 individuals into gainful employment, in addition to serving other persons who have not yet reached their employment goals. Of that total, 7.3% or 626 are individuals with developmental disabilities. However, VR only considers customers with mental retardation or autism to be classified as having a developmental disability. Individuals with other conditions that are considered developmental disabilities under Florida Statute 393, such as cerebral palsy and spina bifida would likely be classified as orthopedic disabilities. The total number of people served by VR in 2001-02 according to disability type is shown in the accompanying box. VR Customers by Disability Type, 2001-02 Blind Chronic Medical Dev. Disabilities Hearing Impaired Learning Disability Mental Illness Orthopedic Dis. Substance Abuse 1.3% or 17.4% 7.3% 10% 5.7% 30.2% 23.8% 4.3% 111 1493 626 858 489 2591 2042 369 VR does not track the individuals they serve with transition services separately. These customers are included within the total. VR is often the source of assistive technology for students transitioning from school to employment. Because of the importance of this service, VR includes 10 rehabilitation engineering technology consultants around the state who provide technology assistance. The Florida Division of Blind Services also provides transition services for students with vision impairments. These services can include vocational evaluation and assessment, low vision aids and adaptive/assistive technology. After the student graduates, additional assistance may be provided, when the student’s primary diagnosis is blindness. These additional services may include mobility training, print magnifiers, Braille keyboards, note taking devices, and specially equipped computers for use on the job. ASSISTIVE TECHNOLOGY The use of assistive technology cuts across all ages and disabilities. However, because of its critical importance in the transition process, information about AT is presented here. Congress passed the Technology-Related Assistance for Individuals with Disabilities Act (Tech Act) in 1988 to increase access and availability to assistive technology by citizens with disabilities. According to the law, such technology is defined as, “any item, piece of equipment, or system, whether acquired commercially, modified or customized, that is commonly used to increase, maintain, or improve functional capabilities of individuals with disabilities.” Assistive technology enables people with disabilities to accomplish daily living tasks; 25 assists them in communication; and provides greater access to education, employment and recreation. It can maximize physical or mental functioning and minimize the impact of a disability. In other words, AT includes devices and services as well as training that help an individual select and use a device or aid. AT devices can be both off-the-shelf and customized to the individual. Some examples of assistive technology include scooters and wheelchairs, alternative automobile controls, environmental controls (handles, switches, etc.), augmentative communication aids, prostheses, hand splints and other orthotics, hearing aids, low vision magnifiers and alternative input/output devices for computers. An assistive technology service is defined as, “any service that directly assists an individual with a disability in selection, acquisition or use of a technology device.” Services can include evaluation, maintenance or repair and training for students, families or professionals. A related concept, called universal design, refers to the process of creating products and environments that are accessible to people with a wide range of abilities, disabilities and other characteristics. The aim of universal design is to make products and environments usable by all people, to the greatest extent possible, without the need for adaptation or specialized design. The more widespread adoption of universal design will greatly minimize the need for assistive technology by people with disabilities. Assistive Technology (AT) Resources. Funded by the federal Tech Act of 1988, the Florida Alliance for Assistive Services and Technology (FAAST) is concerned with making this critically important technology accessible and available to all who need it. (The Tech Act—and the programs funded by it—is scheduled to sunset in FY 2004 unless Congress takes alternative action.) To promote widespread information about AT throughout the state, FAAST has four regional demonstration centers in South, Central, Northwest and Northeast Florida. Each of these centers provides information, hands-on demonstrations, assessments and training on AT. In addition, two regional centers maintain programs to match and recycle used AT devices throughout the state. One center offers equipment exchange and three lend equipment. Newsletters are distributed across the state to keep individuals and professionals informed about current AT developments. From July 2002 through March of 2003 the regional demonstration centers provided the following services for individuals, family members and professionals: Services provided by FAAST during 2002-3/03 Information and referrals - 2685 AT items loaned 87 Training provided 2061 Newsletters sent – 10,923 AT Demonstrations 1124 26 Also, in an effort to assure knowledgeable assistive technology professionals, the Mailman Center maintains an on-line certification course for AT professionals on its web site. DEVELOPMENTAL DISABILITIES PROGRAM (DDP) It is the role of DDP staff to collaborate with VR in transition planning meetings to provide input on local support services, provide information on medical and Social Security benefits, and provide resources for counseling, advocacy, and follow-along support services for supported employment. DDP staff can also provide information on Medicaid waiver home and community based services that will enable individuals to reach their goals for independence and community integration. They should encourage students and their families to apply for the waiver if they are eligible and have not already done so. Other Transition Resources. Some school districts (such as Broward County) also distribute manuals listing area community agencies that provide some type of service related to the transition activity areas of instruction, employment, community experiences, post school adult living, daily living skills and functional vocational evaluations. These manuals can serve to educate the individual and his/her family about the myriad service and resource entities that exist in the local area. Transition informational materials for students and their families are also available through the DOE’s Clearinghouse Information Center. Student materials are most appropriate for use by individuals who do not have severe cognitive impairments. SUMMARY OF TRANSITION SERVICES Transition services are primarily initiated in the school system and include the student, parents, ESE personnel, representatives from DVR, the DDP, relevant community agencies and, where appropriate, Division of Blind Services. Other services that impact upon transition years include health care and dental services. Obtaining comprehensive information and securing appropriate assistive technology for a person with a severe disability can result in an effective transition to the world of adulthood. POTENTIAL OBSTACLES TO SERVICES #1) Lack of participation in transition process by poor, uneducated and minority families #2) Inconsistency in the quality of transition planning within and across school districts 27 #3) Lack of a seamless transfer of assistive technology across life stages, e.g., from school #4) DDP staffs sometimes discourage transitioning individuals from applying for the Medicaid Waiver, due to the current long waiting list. #5) Lack of availability of providers adequately trained to participate effectively in transition services. Recommendations to overcome these obstacles are proposed in Part Two of this report. III. SERVICES FOR ADULTS The previous sections of this report are concerned with individuals from childhood through their school years. We now turn our attention to the adult years, which comprise the largest portion of the life of an individual with a developmental disability. In addition to being the longest span of years, for many reasons, this time of life can also pose the greatest challenges to the public entities charged with providing services. (A separate, final section in Part One describes the services and unique needs of older adults with disabilities and their families.) Ira is a 39-yr-old man with cerebral palsy who uses a wheelchair. A college graduate, Ira lives with his family. With his parents getting older, Ira wants a good job and his own apartment. He needs an electronic communication device and a source of dependable transportation, as well as personal care assistance. Ira has been on the waiting list for the DDP waiver since early last year. The circumstances of each individual with a disability will differ according to the individual’s abilities, level of impairment, changes in health status, secondary disabilities, increasing age, as well as changes in personal, environmental and financial resources. Yet, the public service sector is asked to both anticipate and respond appropriately to each change in an individual’s life. We expect this sort of flexible service capacity to be available to the thousands of Florida residents with disabilities who need services and supports, in order to live as independently as possible in the community. Areas of Service Need. Among the life areas of people with disabilities to be considered in the section are: health care, residential needs and in-home supports, employment and daily life activities, and transportation. The major public service agencies mentioned here are the Department of Health (DOH), the DCF/ADM (Alcohol, Drugs and Mental Health) program, the Developmental Disabilities Program (DDP), Medicaid and Medicaid Waiver services (AHCA), the Division of Vocational Rehabilitation (DVR) and, Transportation Disadvantaged (TD). [Note: Some individuals have Medicare coverage of some aspects of their health care delivered by private providers.] Demographic Factors. With its population of nearly 16 million across 54,000 square miles, Florida is a diverse state, both ethnically and geographically. Of 67 Florida counties, 33 are considered rural by statute. Scattered across the state are also several rural 28 communities that exist within metro counties. These 40 rural living areas are served by a total of 29 rural, often small, community hospitals. An associated economic diversity also exists, with 21 of the 33 rural counties reporting a per capita income that is less than 70% of the statewide average. It is a public health axiom that living in a rural location places an individual with a disability and a chronic condition at greater risk. For example, the Georgetown University Center on an Aging Society reports that the proportion of rural residents with fair to poor physical health is almost one and a half times that reported in urban dwellers in the general population. The Center also finds that rural residents are more likely to experience higher rates of chronic conditions and activity limitations. They are also more apt to be uninsured for longer periods of time, and less likely than urban residents to receive some types of health care, including diagnostic tests for various chronic conditions. Limited access to health care in rural areas is generally associated with the fact that there are fewer providers. Dental Care. The same is true with dental care. Among persons ages 18-64, 66% of urban adults compared to 59% of rural adults have been to a dentist in the past year. There is a disparity in the supply of dentists in rural areas, with 29 dentists per 100,00 residents in most rural areas, compared to 61 per 100,00 in urban areas. Lack of access to dental care is compounded for individuals with disabilities, as providers with expertise in dealing with the complicated care are even scarcer. Dental Problems. Dental problems are more common in people with disabilities and may more occur 15-20 years earlier than in the nondisabled population. Poor tooth alignment and positioning is common, as are high rates of tooth decay and gum disease. A visit to the dentist can be difficult for a person with a developmental disability, as fear, anxiety and general discomfort run high. The individual may not be able to sit comfortably in the dental chair or may be orally hypersensitive and unable to tolerate the dental exam. Anesthesia may be needed for something as simple as a cleaning. Dentists may need to make accommodations in seating and lighting when treating people with disabilities, and provide longer appointment times and more staff. Reasons for the Shortage. Only about 4100 of a total of 200,000 U.S. dentists are available to treat people with disabilities. Lack of proper training is one reason for the shortage, but inadequate reimbursement from Medicaid and other insurers means that the extended time needed to treat patients with disabilities is without compensation. A. HEALTH CARE SERVICES It is common parlance to refer to all long-term care services as health 29 care, particularly in the case of adults with developmental disabilities, since such services emanate from the Medicaid system. However, for the purposes of this report, a distinction will be made between those services that provide a direct medical or therapeutic benefit and those, which deal with other life areas such as living arrangements, employment and community mobility. The former will be discussed under health care; the latter services under the relevant life areas presented. THE DEPARTMENT OF HEALTH (DOH) DOH has three main roles in promoting and protecting the health and safety of all people in Florida. These are 1) health protection, 2) health promotion and disease prevention and, 3) health treatment. Health Protection – Both natural and manmade environmental conditions have an effect on the well being of Florida residents. Contamination of the air, ground water, and food may cause disease or death. The focus of public health efforts is to try to prevent or contain such disease or contamination. Health Promotion and Disease Prevention – Prevention is the key to success in public health. Health promotion and education programs are designed to inform individuals about positive ways in which they can preserve or restore their own health. Disease intervention programs work to stop the transmission of diseases from a carrier to others by immunizing people against certain diseases, treating new cases as they occur, isolating carriers if necessary, and finding and testing people who have been in contact with an infected person to administer the proper treatment before the disease becomes contagious. Health Treatment – Health care of the sick and people with disabilities is a role that public health undertakes when individuals are too poor or otherwise lack access to health care services. The County Health Departments provide most of the public health services in Florida, through partnerships among the state, district offices and the counties. Most services are available at no charge or at a small fee, based upon income. County health departments offer a wide range of public health services, which includes primary care and personal health services, disease prevention, health promotion, diagnosis and treatment of diseases, and environmental surveillance and control. The scope of services offered by or through the county health departments varies among counties. However, all provide a basic core of services, which includes community health assessment, public health policy development and health assurance. 30 It is within each county health department setting that individuals with developmental disabilities may be utilizing services, though no statistics are kept of patients’ disabilities. One local department administrator suggested that the most likely areas of use are the Division of Family Health Services/Bureau of Family and Community Health, which provides primary care, prenatal and well baby clinics, and the. Division of Disease control, which deals with immunizations, HIV/AIDS and sexually transmitted diseases. The number of individuals with developmental disabilities who may be served directly or indirectly by these programs is unknown, since there is no mechanism for identifying an individual with a developmental disability. However, at any given time, an individual county health department may offer specialized clinics, prevention and education programs or other local efforts targeted to individuals with developmental disabilities. That discretion is left to the individual counties. Another area within the DOH that is likely serving individuals with disabilities is the Division of Disability Determination, which is responsible for making decisions regarding the medical eligibility of Florida citizens applying for disability benefits under the state Medically Needy program and the federal Social Security and Supplemental Security Income programs. It also conducts reviews of existing beneficiaries under the federal programs to determine their continued eligibility. THE DEVELOPMENTAL DISABILITIES PROGRAM (DDP) Developmental disabilities can be defined in a number of ways. Under federal law, a developmental disability is a mental or physical disability that occurs before age 22 and substantially limits an individual’s ability in three or more of the following life areas: self-care; expressive or receptive language; learning; mobility; capacity for independent living; economic self-sufficiency; or self-direction. Florida law defines developmental disabilities more narrowly as only those life-long conditions attributable to mental retardation, autism, cerebral palsy, spina bifida, and Prader-Willi syndrome. The Developmental Disabilities Program is one of ten programs administered by the Florida Department of Children and Families. Eligibility for services is limited to individuals three years or older who have one of the five conditions mentioned above. Children ages four and five that are at high risk for a developmental disability are also eligible. Financial requirements must also be met for some services, such as the Medicaid Waiver program. Once a person becomes a client of the program, a financial evaluation is made, to determine eligibility for Medicaid. Persons eligible for Medicaid have a choice between institutional and community care. 31 Individuals not eligible for Medicaid have more limited access to services and supports funded by general revenue dollars. The Developmental Disabilities Program receives funding from the State of Florida (General Revenue) and the federal government (Medicaid Waiver). Each year, the Legislature determines what portion of the state’s budget will be used to fund the DDP, specifying how much general revenue funds are to be used to match federal dollars in the Waiver. These combined state and federal dollars constitute the greatest portion of the DDP budget. A small portion of general revenue funds is also set aside to provide limited services for DDP clients who don’t qualify for Medicaid. Because of the nature of their disorders, adults with developmental disabilities need long-term support. Historically, Florida provided this support in large institutions, called developmental centers or developmental service institutions (DSI). Today, four of these DSIs remain, and one is scheduled to close in 2005. In 1971 Congress authorized the Medicaid program to help states pay for these services to people with developmental disabilities. However, Medicaid policies at the time entitled individuals to receive care only in institutions and not in other community settings. For many years, Florida delivered care in either public institutions (DSI) or in private institutions (Intermediate Care Facilities for Individuals with Developmental Disabilities or ICF/DDs). It was not until the early 1980s that federal and state governments began to realize that many individuals with developmental disabilities could be served in community based settings, if they received appropriate, individualized supports. Community based services offer two distinct advantages over institutional care. First, most individuals with developmental disabilities prefer community based care to institutional care and, second, many individuals can be served at lower costs in community settings. Having this knowledge, the federal government subsequently allowed states to enter into agreements that would allow them to change the service delivery system for people with developmental disabilities. Under these agreements (commonly called waivers), the federal government puts aside certain Medicaid requirements, including the mandate that care be provided within an institution. In return the state must assure that services will meet certain standards and will not cost more on average than institutional care. Medicaid Waiver Programs in Florida. Currently, Florida operates a specific Home and Community Based Services (HCBS) Medicaid Waiver for individuals with developmental disabilities. It is one of ten specialized Medicaid waivers administered by the State. The other nine waivers are: Supported Living Waiver – also operated by the DDP, for individuals aged 18 and older who are able to direct their 32 own support in most areas, and meet the level of care for an ICF/DD; Consumer Directed Care (CDC) – in part under the DDP and originally a demonstration program, this waiver won recent federal approval as a statewide Independence Plus Waiver for individuals who choose to purchase their own services; Aged/ Disabled Adult Waiver – for persons over aged 65 or adults with other disabilities; Channeling Waiver – open to those 65 and older in MiamiDade and Broward Counties who meet the nursing facility level of care; Model Waiver – for children under 21 who are diagnosed with a degenerative spinocerebellar disease; Nursing Home Diversion Waiver – a pilot program for those 65 and older who are eligible for Medicaid and Medicare and live in certain areas of the state; Project AIDS Care Waiver – for individuals with a diagnosis of AIDS who also have certain opportunistic infections; Statewide Inpatient Psychiatric Program Waiver – for children under 18 who need a maximum of 120 days hospitalization to stabilize psychiatric problems; and, Traumatic Brain Injury/Spinal Cord Injury Waiver – for persons with an external injury who are also clients of the Brain and Spinal Cord Injury Program. The DDP Medicaid Waiver is meant to provide recipients (beneficiaries) with services in certain basic life areas. These include: - Having a safe place to live - Having a meaningful day activity - Receiving “medically necessary” medical and dental services, and - Receiving the transportation required to access necessary services. For adults, a “meaningful day activity” may be a choice of paid employment, supported employment, adult day training or nonresidential support services. Furthermore, all waiver services must meet the test of being “medically necessary” and satisfy the following: Be necessary to protect life, to prevent significant illness or disability, or to alleviate severe pain; Be individualized, specific and consistent with symptoms or confirmed diagnosis of the illness or injury under treatment and not in excess of the person’s needs; Be consistent with generally accepted professional medical standards, as determined by the Medicaid program, and not experimental or investigational; Be reflective of the level of service that can be safely furnished, for which no equally effective and more conservative or less costly treatment is available statewide; Be furnished in a manner not primarily intended for the 33 convenience of the recipient, the recipient’s caretaker or the provider; Consistent with appropriate medical care, inpatient hospital services could not be effectively furnished more economically on an outpatient basis or in an inpatient facility of a different type. By way of comparison, HCBS waiver expenditures increased an average of about 14% nationally between 1998-2001. During that same period, Florida’s expenditures increased by 94%. This is consonant with efforts in other states. In 2001, $10.5 billion in waiver expenditures across the country were used to purchase community based supports for individuals with developmental disabilities. This is a larger amount than the total national expenditure of Medicaid dollars ($10.4 billion) to purchase services in ICFs/DD. However, as recently as the year 2000, that latter trend was not true in Florida, where federal Medicaid revenue was greater for ICF/DD services ($159 million) than for the HCBS waiver ($134.7 million), according to the University of Colorado, Coleman Institute. DEVELOPMENTAL SERVICES HOME AND COMMUNITY BASED SERVICES WAIVER. The DDP waiver is a Medicaid program that provides home and community based supports to eligible persons with developmental disabilities living at home or in a home-like setting, as an alternative to living in an ICF/DD. The waiver is funded by the federal Centers for Medicare and Medicaid, combined with matching state dollars. The waiver is operated by the DDP, under the authorization of AHCA’s Division of Medicaid. Local district/regional offices enter into contract with private service providers. Eligibility Requirements for the Waiver. All participants in the waiver are eligible for admission to an ICF/DD and must be provided a choice of receiving services in an institutional setting or in a home and community-based setting. In addition to meeting financial eligibility requirement for Medicaid, in order to participate in the waiver the individual must: 1. Be a consumer of the DDP 2. Meet one of the following level of care eligibility options: 1). An IQ of 59 or less; or 2). An IQ of 60-69 and the individual has a secondary handicapping condition which includes cerebral palsy, spina bifida, Prader-Willi syndrome, epilepsy, autism, ambulation, sensory, chronic health and behavior, or 3). An IQ of 60-69 and the individual has severe functional limitations in at least three of the major life activities, including self-care, 34 learning, mobility, self-direction, understanding and use of language, and capacity for independent living, or 4). A primary disability of autism, cerebral palsy, spina bifida or Prader-Willi syndrome. In addition, the condition must result in substantial functional limitations in three or more major life activities, such as self-care, mobility, learning, self-direction, understanding and use of language and capacity for independent living. In addition, the individual or his/her legal guardian must choose to receive home and community-based supports and services. According to guidelines, individuals enrolled on the waiver are to be provided with those services that have been determined to be medically necessary with reasonable promptness—within 90 days of the date of the individual’s enrollment on the waiver, or request, to the extent that sufficient provider capacity exists. A wide array of services is available on the DDP Medicaid waiver. Currently all services must be planned by and coordinated with a support coordinator. Individual clients can select locally from nearly 500 waiver support coordinators across the state, when they are enrolled on the waiver. These private waiver support coordinators work with the individual recipients and their families to determine an individual’s service needs, develop support and cost plans, coordinate service delivery and monitor the use of services. Some services are directly related to health or dental care. As mentioned earlier, other services refer to living arrangements, day activities or transportation. A number of services may overlap various life areas. The health/medical services include: adult dental, behavioral services, dietician, occupational therapy, physical therapy, private duty nursing, psychological services, respiratory therapy, residential nursing, skilled nursing services, special medical equipment and supplies, special medical home care, speech therapy, specialized mental health services and therapeutic massage. (Primary and specialty physician medical care, hospital in-patient and out-patient treatment, prescription coverage, glasses, hearing aids, etc. are provided under the Medicaid State Plan and are not covered by the waiver.) Services that deal with living arrangements include: chore services, companion services, environmental modifications, homemaker, inhome supports, personal care assistance, personal emergency response system, residential habilitation and supported living coaching. Transportation provides access to community resources and waiver services, and supports in many life areas. Services that deal with day activities include: adult day training, non-residential support services 35 and supported employment. The Medicaid State Plan covers medical trips. Persons Receiving Institutional Care 2001-02 MRDP Program Sequin Pathways (at Landmark) Public ICFs Private ICFs Total served 124 30 16 1357 2068 3611 FUNDING AND INDIVIDUALS SERVED IN 2001-02 The total budget for the DDP during this year was $880 million. According to AHCA, the number of individuals served under the HCBS Medicaid waiver during 2001-02 was 24,954. Another 1636 were served under general revenue dollars or under the Medicaid State Plan. Close to 11,000 individuals are currently on the waiting list for the Medicaid Waiver. Therefore, the combined total of individuals seeking or receiving community based services is approximately 37,600. Another 3611 people received institutional care the same year. This brings the total number of currently known individuals with developmental disabilities seeking or receiving services in Florida to more than 41,000. Individuals known to the DDP Medicaid waiver GR/Medical State Plan Waiver wait list Institutions Total 24,954 1,636 11,000 3,611 41,201 A. Measure of Florida’s Success with Medicaid waiver services. In recent years Florida has made considerable strides in the number of individuals who participate in the DDP Medicaid waiver program, as can be seen in the two following graphs. 36 On the Other Hand…As can also be noted from the above and following three graphs, Florida still lags behind the rest of the country in the amount of money it spends per participant on the Medicaid waiver. Florida also ranks last among the six largest states for the total dollars it spends on people with developmental disabilities, in relationship to the total number of state residents. 37 SERVICES PROVIDED The following table displays the health-related services provided under the DDP waiver in 2001-02. The number of people served, dollars expended and the percent of budget are shown for each service delivered. A frequently requested service, adult dental care, was provided to nearly 5000 people. As can be noted, all of these health services comprise only a small portion of the overall waiver budget. Only Consumable Medical Supplies accounts for 2% of the budget; all other services equal 1% or less, per service. 38 FY 2001-02 PHYSICAL THERAPY Behavioral Therapy Occupation Therapy Speech Therapy Adaptive Equipment Cons Med Supplies Pers Emerg Respons Private Duty Nursing Skilled Nursing Sp Med Home Care Residential Nursing Adult Dental Care Dietician Services Respiratory Therapy Therapeutic Massage Behavioral Assistant Sp Mental Hlth Ther Medication Review Recipients 728 2,759 418 885 2,034 7,158 79 76 310 75 172 4,972 283 3 270 530 534 327 Amount Paid $1,874,107 5,209,448 874,608 1,744,346 3,068,719 9,549,763 18,852 2,978,992 1,828,962 2,892,007 2,399,184 3,664,639 163,991 16,616 561,861 2,600,600 812,007 20,313 % of Budget <1% 1% <1% <1% 1% 2% <1% 1% <1% <1% <1% 1% <1% <1% <1% <1% <1% <1% Quality Assurance. Given the rapidity of recent growth in the DDP Medicaid waiver program, and the need to assure quality services and effective outcomes, in September 2001 AHCA contracted with the Delmarva Foundation (an experienced non-profit, peer review organization) to provide uniform, statewide quality assurance. During their four-year contract, Delmarva will be conducting more than 10,000 person-centered interviews with a selected sample of individuals receiving services. They will also be reviewing all providers of waiver services, either on-site or by record reviews. Delmarva is partnering with a number of recognized experts in the health and long-term care field to accomplish their tasks. Findings to Date. While the greater portion of Delmarva’s work is currently underway and will continue till 2005, some expected preliminary findings have emerged. These include the fact that, of the 26,163 individuals eligible for the Medicaid waiver program in the first year of their review, 86% are adults over the age of 21; 444 are aged 65 or older. (See the following section of this report, Services for Older Adults, for more details about this population.) 62% of these individuals on the waiver reside in their family homes. Prior Authorization. A second aspect of the checks and balances in effect for the DDP waiver is the prior authorization component for costeffectiveness, being conducted by Maximus under contract with the DDP. The role of Maximus is to assure that services requested by support coordinators are medically necessary and meet the individual consumer’s needs. They further ensure that providers deliver all services with the appropriate intensity, frequency and duration. Prior 39 service authorization does not apply to every consumer, but rather to those whose annual cost plans exceed the average cost of an ICF/DD, $77,975. It may also pertain to other consumers when the cost of a particular service is high, or when a combination of services has a higher than average cost. Services Outside of the DDP. Mental Health Care Services. Another area of health care that is available to adults, including those with developmental disabilities, is mental health services. The DCF/ADM program that operates mental health services has two main divisions: Mental Health and Substance Abuse. The funding sources for these services are State general revenue funds, a mental health block grant (primarily for children and substance abusers) and federal Medicaid dollars, matched with state funds. Across the state there are four civil mental health institutions for adults (two are privately run) with a total of 1039 beds, and three forensic facilities. ADM services are provided to three target groups: adults with severe and persistent mental illness, adults in mental health crisis and adults with forensic involvement. Most mental health services are provided through a system of some 350 community based providers throughout the state. ADM manages contracts with providers in 14 districts around the state. For access to community mental health services, provider staffs enroll clients by using a checklist to determine their eligibility through a combination of diagnosis, client characteristics (legal status, functional level) and requirements of the funding source. Historically, the ADM program did not identify the recipients of its community services by disability, so there was no way to determine how many people with developmental disabilities were being served. However, in 2002-03, some mental health programs began capturing that information. To date, 3,871 individuals receiving community services have been identified as having developmental disabilities. [Note: While the Mentally Retarded Defendant Program (MRDP) is located on the grounds of the North Florida State Hospital in Chattahoochee, it is considered a secure DDP site, not a mental health venue.] SERVICES PROVIDED. For FY 2001-02, ADM budgeted a total of $377 million and delivered the following community services to adults: 1) Served 140,000 adults, 13,000 of whom are aged 60 and older; 2) Supported adults with severe and persistent mental illness to live in the community an average of 350 days and to be employed an average of 35 days a year; and, 3) Avoided recommitment on over 98% of the community forensic clients. 40 Quality Assurance for mental health services is provided primarily through the use of performance measures, both client outcomes and service outputs, which are developed for each target group served. These performance measures for each relevant target group are included in providers’ contracts and monitored at regular intervals throughout the year. With this overview of publicly funded health care services, we turn our attention now to service needs in other core life areas—residential or living options, employment and day activities, and transportation and community mobility. RESIDENTIAL SERVICES DDP Services. The selection of a living arrangement is the basic defining characteristic that determines whether the reception of services for an individual will be in an institutional setting (public or private ICF/DD) or in a home in the community. If a certain level of care is needed, an individual and his/her family may opt for care in an institutional setting. However, that is not the choice of most people. There are four public institutions. Private ICFs/DD can be found in 28 of Florida’s 67 counties. However, not all of these venues have vacancies. For instance, beds in specialized private ICFs/DD, known as “cluster homes,” are limited and reserved for persons with the most complex medical conditions and mobility impairments. As has been noted, the four public institutions (DSIs) are being phased down. For instance, the Community of Landmark in Miami is slated for closure in 2005; individuals residing there are being transferred to community settings. On the other hand, there is a range of residential possibilities that can be considered community based. The DDP consumer may live in a foster home, a small group home, the family home, or a home or apartment of his/her own. Using state funds, the DDP pays foster parents and may pay a provider for the cost of living in a group home. Residential Habilitation (Res Hab). Individuals on the Medicaid waiver who live in group homes pay their own living expenses from SSI, SSA or SSDI benefits or private funds. These individuals then receive a waiver service called Residential Habilitation (Res Hab), to provide individualized training to help them acquire or maintain daily living skills. Though the DDP does not directly own any community residences, services to support individuals who wish to live in their own homes are available through the Medicaid waiver (supported living coaching, inhome supports, homemaker, personal care assistance, etc.) However, it is incumbent upon the individual and/or family to first obtain the home. 41 Supported Living Coaching is the second residential-specific waiver service. This service is very broad, encompassing a variety of training and support activities designed to support individuals who wish to live in their own homes or apartments, integrated into the community. Activities may include: assistance with locating appropriate housing; the acquisition, retention or improvement of skills related to activities of daily living such as personal hygiene or grooming; household chores; meal preparation; shopping; personal finances; and, the social and adaptive skills necessary to enable individuals to reside on their own. Supported living services mean the provision of all supports necessary for adults to establish, live in and maintain households of their own choosing in the community. Role of the Coach. A supported living coach performs three assessments for the individual. These are a Functional Community Assessment, a Housing Survey and a Financial Profile. The first, or Functional Community Assessment, identifies the type of training, assistance and intensity of support needed by the individual. It is a tool designed to assist the coach with becoming familiar with the individual’s capabilities and needs. This annually updated tool covers all areas of daily life include relationships, health and medical concerns, personal care, household and money management, community mobility, recreation and leisure. The Housing Survey is used to inspect a prospective home to ensure it is safe for the potential occupant. The coach updates this survey quarterly, also considering the individual’s overall health, safety and well-being, and forwards it to the individual’s support coordinator. The Financial Profile is an analysis of the household costs and revenue sources necessary to maintain a balanced monthly budget for the individual. The analysis will also substantiate the need for a monthly subsidy or initial start-up costs. It is also a source of information for determining a strategy for assisting the person with money management. If a subsidy is needed, this must be approved by DCF before the individual signs a lease. Related DDP Services. While several Medicaid waiver services may be used as supports in a residential situation (homemaker, chore, durable medical equipment and supplies, etc.), two other waiver services are often used to support individuals with disabilities who live in their own homes. These are in-home supports and environmental accessibility adaptations. In-Home Support Services. These services provide an individual in supported living with a support worker who is present from four hours a day up to 24 hours a day. This worker may provide companionship, personal care and assistance with daily living. The worker may also live with the individual in the home or apartment, sharing living expenses. These services are separate from, and in addition to, the 42 services performed by the supported living coach. Respite Care. This service provides supportive care and supervision to an individual when the primary caregiver is unable to perform these duties due to a planned, brief absence, an emergency absence, or when the caregiver is physically unable to provide care or supervision for a brief period. This service may be provided in the person’s own home, the family home or a foster home. (This service is used primarily to support parent caregivers.) Environmental Accessibility Adaptations. These are physical adaptations to the individual’s home that are medically necessary to avoid institutional placement and to enable the individual to be more independent in the home. These adaptations include such things as ramps, grab bars, widening of doorways, modification of bathroom facilities, etc. These adaptations can be made only when the person is living in his/her own home or in the family home; rental properties are limited to minor adaptations and landlord’s approval. SERVICES PROVIDED/RESIDENTIAL TRENDS The following chart displays trends in Florida residential settings for individuals who received Medicaid waiver services for the years 2000, 2001 and 2002. According to AHCA, the people receiving Res Hab services in 2000-01 numbered 5741; Supported Living Coaching services, 2870. For FY 2001-02, the totals for those services are 7609 and 3054 respectively. Florida Residential Trends: Medicaid Waiver - Years 2000, 2001, 2002 Individuals Receiving Residentialrelated Waiver Services (2001-02) 8000 6000 In-Home Supports – Environ. Adapts. – Personal Care – Chore – Homemaker – Respite - 725 727 4756 81 696 5241 Res Hab 4000 Supp. Living 2000 0 2000 2001 2002 In 2003, the DDP waiver is currently serving 6,510 individuals with Residential Habilitation (Res Hab) services and 3054 individuals with Supported Living Coaching (SL) services. [Note: Although Res Hab is a service generally provided in a licensed facility, it may also be provided in some individual and family homes.] Res Hab is the single most expensive service on the waiver. The cost of Res Hab services in 2001-02 was approximately $200 million (40% of the waiver budget). For SL services it was $17 million. During that same year, $17 million was also spent for the 834 individuals who received in-home support services. [Note: While not all individuals who live independently receive 43 both SL services and in-home supports, it is a common service in these settings.] The DDP reports that a total of 455 individuals have moved from a foster home, a group home or from Res Hab services into a supported or independent living situation since 1999. Irma is a 37-yr-old woman with mild mental retardation who has lived in a group home for 20 years. Now she wants to have her own home, where she can have some privacy and enjoy her own things. Florida Housing Coalition. The Affordable Housing Opportunities project is funded by the Florida Developmental Disabilities and conducted by the Florida Housing Coalition, a statewide non-profit organization. The Coalition brings together housing advocates and resources so that all Floridians have a safe and affordable home and a suitable living environment. This project conducted a needs assessment to determine the scale and scope of housing available to individuals with developmental disabilities. The project also provided technical assistance to stimulate demonstration-housing partnerships around the state, and studied existing examples of best practices that occurred between 1998-2002. Certain key findings emerged from their September 2002 report, Affordable Housing Opportunities for People with Developmental Disabilities: Demonstration Projects and Best Practices. Among these findings are: 1) There is a critical shortage of housing for people who have extremely low incomes; 2) People with disabilities generally have disproportionately low incomes compared to area median income levels; 3) Low income levels create such a barrier to obtaining housing that services, such as supportive living, cannot be used effectively; and, 4) Living in a home of one’s own rather than a congregate setting may be an impossible dream for many people with disabilities, unless innovative solutions are developed and used. The report also notes that for individuals with incomes under $500 per month, rental housing is the most accessible and convenient form of housing. However, an increase in existing rental assistance programs and creation of new state and local programs is needed. Overall, the study indicates that there are, indeed, a few exemplary housing programs in Florida that are creating housing for low-income households with special needs such as disabilities. Unfortunately, these exemplary efforts are not widely known or replicated statewide. More typically, a creative supported living coach discovers local housing assistance programs and initiates activities on behalf of one individual. [Note: The projects discussed in the demonstrations report take place in mostly urban areas of the state.] Another finding is that home ownership may be possible and successful for some few individuals with disabilities who have both higher incomes and good, ongoing support networks. This report and earlier Coalition project activities make it clear that there is a great need for training and technical assistance across the state, to help individuals with developmental disabilities (and the 44 professionals who work with them) access the housing resources that are available to all low-income residents. These include city and county programs, housing counseling and education providers, non-profit housing providers and the banking industry. Equally clear is the need for increased advocacy to maintain and increase funding for affordable housing at the state and federal levels, as well as increased funding for direct rental subsidies, down payment and closing cost assistance, below market rate interest and flexible underwriting for individuals who have developmental disabilities. The Need for Affordable Housing. The private housing market in Florida does not produce an adequate supply of housing that is affordable to people with low and very low incomes. A 1999 report indicated a shortage of some 1,371,970 units statewide. Housing Resources. Owning a home is dream of many people, regardless of their income, culture or geography. Almost 75% of Florida residents are homeowners. For most people, purchasing a home is possible only with financing from an outside source. For a person with a low or very low income it may be impossible to borrow money to purchase a home, because saving enough money for a down payment can be an overwhelming task on a minimum wage income. Affordable housing programs are designed to bridge the gap between savings and the down payment by adding subsidy dollars to the amount a lender is willing to loan. The subsidy amount, usually a second mortgage with flexible terms, can bridge the gap between a buyer’s savings and the amount of the first mortgage. SHIP. According to the Florida Housing Coalition, Florida ranks high among other states for the quality of its affordable housing program, SHIP. This State Housing Initiatives Partnership (SHIP) provides more than $120 million each year to local governments to fund affordable housing programs. These governments must create a Local Housing Assistance Plan (LHAP), which identifies local strategies to develop affordable housing, as a condition of participation in the program. Created in 1992 by the William A. Sadowski Affordable Housing Act, this documentary stamp surcharge produces revenue that is dedicated to affordable housing. SHIP funds can be leveraged with other money, such as private lending sources, federal programs and mortgage revenue bonds. SHIP is an excellent source of purchasing assistance because 65% of the money must be expended on home ownership activities. SHIP is also used for rehabilitating existing homes, including making accessibility modifications. Local administering agencies (cities or counties) make specific guidelines for these expenditures. Other Considerations. When weighing the potential of home ownership by a person with a developmental disability, the ability of the 45 person to make inevitable future repairs should be part of the equation. Another consideration is that some individuals with disabilities will have higher living costs than others. For example, not all medical costs may be covered by Medicaid or insurance. As a result, the individual may have to pay for certain prescriptions, treatments, equipment or supplies. Further, if a special diet is involved, food costs may be higher. Transportation costs may also be high, if the individual requires special services. All of these items must be factored into an individual’s housing plan to assure a successful outcome. Local Agencies with Home Ownership Projects. A number of non-profit agencies across the state administer programs to assist individuals with disabilities to obtain their own homes. These include: Putnam ARC, Putnam, Nassau and Levy Counties; Abilities, Inc. of Florida, Pinellas County; Bradford ARC, Bradford County; Key Training Center, Citrus County; CCAR Services, Inc., Clay County; and, Grove House, Duval County. Among the services typically provided by these agencies and their community partners are pre and follow up support services, assistance with credit checks and down payment, assistance with loan application and construction/rehab management, SHIP financing for first or second mortgages, flexible underwriting of loans and homebuyer training classes. Most of these non-profit agencies provide some degree of supported living services to the homeowners. Rental Housing. Approximately 25% of Floridians rent their homes. For people with disabilities who have very low incomes, making the transition to homes of their own is often more successful with rental housing. However, rental rates and initial deposits can be very high, seemingly putting safe, affordable housing out of reach. In addition, the costs of any necessary modifications are generally the renter’s responsibility. The solution can be local housing programs that offer low rental rates, safety, accessibility and some permanency. The use of Section 8 vouchers and other rental housing assistance are essential when planning. Beyond having adequate and affordable housing, persons with disabilities must also be assured of well-established systems of support services. Partnerships between affordable housing providers and support providers must be synchronized from the outset, so that the right combination of appropriate location, type of housing, cost, and any necessary environmental modifications, or facilities for supports (such as live-in attendants) is obtained. This sort of close collaboration forms the basic foundation for successful rental housing development for individuals with disabilities. Local Agencies with Rental Housing Projects. Several non-profit entities across the state operate projects to assist individuals with disabilities to obtain rental housing. These include: the Coalition to Assist Supported Living, Inc. (CASL) in Alachua, Lee, Sarasota & Manatee Counties; Grove House (CASA Project), Duval County; and, 46 Abilities, Inc. (condominiums), Pinellas and Brevard Counties. Various combinations of state, federal and private funds were used in these efforts. The efforts undertaken by CASL are particularly noteworthy and will be summarized as an example of a best practice by a community entity. Example of a Best Practice. A number of the members of CASL are parents of individuals with developmental disabilities. CASL recognized that, although supported living services are available from the DDP, supported living providers are not allowed to also own the housing. Consequently, there is a dearth of affordable, community based housing. To fill the existing gap, CASL determined to become an organizational homeowner and property manager. To accomplish this, the group solicited funds from Lee, Manatee and Sarasota counties, as well as the Selby and Venice Foundations. More than $2 million in initial donations enabled them to purchase 20 homes, outright, for use by more than 50 renters. Several more homes are also under contract for purchase. As the owner, CASL is responsible for the insurance, maintenance and general upkeep of the homes. Renters receive their supports from local disability and supported living providers, usually under the DDP Medicaid waiver. This simple concept of partnering a separate non-profit property management organization with support providers has proven so successful that it is under consideration in other areas now. Other Housing Resources. In addition to the specific projects described above, 33 of the total 105 Florida counties and municipalities provide some form of housing assistance. These forms of assistance can range from state funded programs like SHIP funds which can be used for emergency repairs, new construction, home rehabilitation, down payment and closing cost assistance, impact fees, construction and gap financing, mortgage buy downs, acquisition of property for affordable housing, matching for federal housing grants/programs and home ownership counseling. Federally funded resources include the Community Development Block Grant, which can support non-profit agencies providing services to low income people, for infrastructure development in low income communities and, commonly, for housing rehabilitation. Section-8 Rental Assistance is provided by the United States Department of Housing and Urban Development (HUD) to local housing authorities. It may come in two forms: 1) vouchers, which an individual may use to pay for housing in the community and, 2) Section-8 project-based assistance, which is attached to a unit to make it affordable. The voucher program typically has a long waiting list, though the local authority may designate a special priority for persons with disabilities. Project-based assistance allows a housing authority to attach rental assistance to affordable housing units that are specially designed for people with disabilities. Such units are typically found in public housing complexes run by the local housing authority. 47 Other housing-related programs that are available to individuals with disabilities are administered through the Florida Department of Community Affairs, with funds distributed via local authorities. These include the Low Income Emergency Home Repair Program, the Low Income Home Energy Assistance Program and the Weatherization Assistance Program. Eligibility for the housing programs listed above is based on comparing the individual’s income with the median income for the area (AMI), according to family size. (HUD publishes the AMI for each area periodically.) Most individuals with developmental disabilities, particularly those with SSI incomes, can qualify financially for HUD programs. Private Resources. Another potential source of housing for individuals with developmental disabilities can be homes made available by their parents. This can be done either through the purchase by the parents of a home or condo for the offspring, or the transfer of the family home to the adult child, either prior to or upon the death of the parent(s). [Also see following section on older adults for more discussion of this option.] Other community alternatives pursued by small groups of parents across the state include the development of private group homes and mixed residential developments. The latter include built-in support resources for the individuals with disabilities who live there. C. EMPLOYMENT AND DAY ACTIVITY SERVICES The previous section of this report deals with school transitions and the various public entities involved with providing transition services. In this portion of the report we look at the three public agencies— DDP, DOE and DVR—that provide employment and day activity services to adults with developmental disabilities. DDP Services. As in many states around the country, the current employment services in developmental disability programs in Florida are partly a holdover from the ubiquitous “sheltered workshops” of the 1970s and 80s. Many service providers converted their workshops to adult day training programs for the Medicaid waiver during the 1990s. [Whether this philosophical conversion resulted in more than a name change is discussed further in Part Two of this report.] Adult Day Training (ADT) Services. Day training programs are broad training services intended to help individuals take part in daily, valued routines of the community. They include work-like settings that do not meet the definition of supported employment. The services provided must stress training in the activities of daily living, self-advocacy, adaptive and social skills, and be age and culturally appropriate. The goal is to attain participation in less restrictive settings. These facilitybased programs should offer a variety of activities that are of interest to the individuals participating, and are related to personal goals and 48 outcomes desired by the individuals involved. Mobile crews, enclaves and entrepreneurial models that do meet the standards for supported employment can be included as ADT off-site services. Assistive Technology. AT is a valuable tool that can enable people with disabilities to remain in control of their lives, as well as enhance their presence and visibility in the community. Assistive devices run the gamut from low tech to high tech, computerized devices, which affect mobility, communication and independent functioning. Durable Medical Equipment (DME) is a Medicaid waiver service that provides assistive devices to individuals when such assistance is deemed “medically necessary” for that person’s health and well being, and that assistance is not provided by another source (e.g., DVR). Other sources of AT information include FAAST and the Advocacy Center for Person with Disabilities. Supported Employment. The other employment related service under the Medicaid waiver is supported employment, which may be either an individual or group format. With the individual approach, one person is helped to obtain competitive employment with the assistance of a job coach, employment specialist, or job consultant. Both intensive training (Phase I) and systematic follow-along supports (Phase Two) are provided. This model can be applied to employment in the general work force or to a business to be operated by the individual. Within the group format, three models are used. These include: Enclave – up to eight individuals work either as a group or dispersed individually through an integrated work setting, under supervision of the provider. Mobile Crew – a crew of individuals performing activities such as lawn maintenance or janitorial activities in business or other community settings, with supervision by the provider. Entrepreneurial – up to eight individuals work in a small business created specifically by or for them. SERVICES PROVIDED/EMPLOYMENT TRENDS In 2003, the DDP waiver currently serves 10,727 individuals in Adult Day Training (ADT) and 2472 individuals with Supported Employment (SE) services. Though ADT is meant to be a transitional service, it is seldom used that way. According to DDP statistics, 23 people appeared to transition from ADT programs into SE between 2001-02 and 2002-03. Another 59 individuals who received only ADT services in 2001-02 are receiving both ADT and SE services this year. (It should be noted that it is common for individuals beginning employment to work part-time and to continue to attend an ADT program part-time.) The following chart displays the trends in Florida employment services for individuals who received Medicaid waiver services in the years 49 2000, 2001 and 2002. According to AHCA, the number of individuals receiving Adult Day Training services in 2000 was 10,330; Supported Employment services, 2850. For FY 2001-02, the totals for those two services were 10,919 and 2764, respectively. The cost of ADT services in 2001-02 was approximately $63 million. This represents 13% of the waiver budget. The cost for SE services was $7 million. FL Employment Services Trends, Medicaid Waiver - 2000, 2001, 2002 12,000 10,000 8,000 6,000 4,000 2,000 0 Ad. Day Trg. Supp. Emp. 2000 2001 2002 DOE Services. Many school districts across the state offer adults with disabilities another option for day activities—adult education classes. Adult and community education classes are offered at community education sites and at off-site locations such as ADTs and some group homes. Individuals who are 16 years of age or older may choose to participate, and can be eligible for special services and assistance in those classes. Broward County Schools, for instance, also has a grantfunded non-workforce educational program to enable students with developmental disabilities to acquire and develop skills of selfsufficiency and increase community independence. Opportunities are provided for community exploration, volunteer, and work skills training. Individuals with disabilities who do not have a regular diploma or a GED may also choose to attend vocational/technical classes at vocational-technical (Voc/Tech) centers or community colleges across the state. Individuals who have a special diploma or certificate of completion may be required to take a basic skills test to prove they have the academic skills to benefit from the voc/tech training. DVR SERVICES This agency provides services for Floridians of working age with physical or mental impairments. These services allow them to prepare for, obtain, keep or regain employment. (For a detailed description of the DVR eligibility criteria and steps in the service process, see prior section of this report, Services for Children Transitioning from School.) Individuals who use DVR services have the right to choose their counselors, the services they receive, their service providers, and the jobs they attain. 50 Training and Retraining. DVR may provide necessary vocational and other training services for individuals to determine eligibility or participation in trial work. Services may also include personal or vocational adjustment to help the individual develop certain identified personal or social behavior patterns or work habits, which are necessary for successful employment. Medical and Psychological Evaluation and Treatment. Prior to employment, an individual may need medical, psychological and/or dental consultation and treatment to correct or modify a stable or slowly progressing physical or mental condition that may be a substantial impediment to employment. Angela is a petite, 30-yr-old woman with retardation who lives with her family. She has always been fond of animals, especially her beagle puppy. She would like to get a job caring for small animals and thinks a job coach can help. Supported Employment. The purpose of supported employment service is to assist people with the most severe disabilities achieve competitive employment. For this reason, it is the service most appropriate for many people with developmental disabilities. Job coaching is the core service provided through the supported employment program. DVR provides the funding for contracted job coaches who give the support needed to achieve and maintain employment. Supported employment in DVR has three distinct features. It: 1. Allows competitive work in integrated work settings; 2. Targets individuals for whom employment has not traditionally occurred, or has been interrupted or intermittent because of their disabilities; and, Provides ongoing support services as needed, for the individual to successfully maintain employment. Typically, DVR provides supported employment services to an individual with a developmental disability (Phase One), combined with services from the Medicaid waiver (Phase Two, follow-along). However, if the individual is not eligible for services from DVR, all services may be provided under the Medicaid waiver. Rehabilitation Technology. This service is the systematic application of technologies, engineering techniques or scientific principles to meet the needs of and address the barriers confronted by the individual with disabilities in areas that need education, rehabilitation, employment, transportation, independent living and recreation. Assistive Technology (AT). This comprehensive program of assistive technology services includes assessment, evaluation, and purchase of assistive technology devices. AT services and devices are meant to increase opportunities for employment. Importantly, these devices can also enable participation in educational activities, home life and community activities. Contracted Rehabilitation Technology Service Provider. This service is provided via the Contracted Rehabilitation Technology Service 51 Provider (CRTSP) at the University of South Florida. A CRTSP evaluates a referred individual and submits a detailed letter outlining recommended products and services to the referring counselor. Such services may include building modifications, worksite assistive technology, wheelchairs and scooters, computer equipment, vehicle modifications and driving assessments, and post-employment services. In addition, the following services are commonly provided by DVR: counseling and guidance, personal assistance services, tools and equipment, telecommuting, independent living services, placement and follow-up services, interpreter services, and transportation. Independent Living. DVR is also the administering agency for the statewide network of 14 Centers for Independent Living (CILs) that provide skills training, peer counseling, advocacy and, information and referral. Some CILs also provide interpreter services for the deaf, attendant care training and, Americans with Disabilities Act (ADA) architectural surveys. These centers are community based and consumer controlled. Though open to people having a broad spectrum of disabilities, the traditional focus of Florida’s CILs has been on assisting people with sensory impairments or physical disabilities. SERVICES PROVIDED. According to their 2001-02 report, DVR successfully placed 8759 individuals in jobs during that year. Of that number, 37% are considered severely disabled and 42% most severely disabled. 7.3% or 626 have developmental disabilities; 24% or 2042 have orthopedic disabilities (Total 2668). [As mentioned in the previous section, DVR classifies only individuals with mental retardation and autism as having developmental disabilities; those with the conditions of cerebral palsy and spina bifida are classified as have orthopedic impairments.] Other categories of individuals served by DVR are those who are blind or hearing impaired, persons with a chronic medical condition, a learning disability, a mental illness or those who abuse substances. Less then 33% of people with disabilities work at all; only 18% work full time. Obstacles to Employment for People with Disabilities. The U.S. Census bureau reports that while less than one-third of people with disabilities work at all, only 18% work full time. Perhaps shedding some light on the reasons behind those appalling numbers, a March 2003 report by Rutgers University presented the following results from a recently completed employer survey. Only 26% of employers state that their company employs at least one worker with a physical or a mental disability. Nearly 17% of employers believe that the lack of skills and experience on the part of the job seeker is the greatest barrier. 15% cite employer reluctance to hire workers with disabilities. 52 Only 40% of employers surveyed provide training of any kind to their employees regarding working with or providing accommodations to people with disabilities. Employers admit internal barriers such as: discomfort with disabled workers; belief that the job cannot be performed by a person with a disability; and, fear of accommodation costs. 60% of employers say that the federal government should offer tax incentives to employers for hiring people with disabilities and to pay for workplace accommodations. Employers in the hospitality industry are the most likely to support tax incentives. Of all the workers with disability who are hired, the hospitality industry hires the largest number of workers; the manufacturing industry the least. However, nearly 74% of employers also believe that employers, government and workers are equally responsible for equality in the workplace. Only 11% of employers have developed recruiting methods and strategies that specifically target people with disabilities. Only 12% have changed the format of job applications to make them more accessible, or changed the tests or evaluations used in hiring or promotion. Only 7% have changed the company’s web site to make it more accessible to people with disabilities. Other Day Activities under the Medicaid Waiver. For individuals with disabilities who do not participate in competitive or supported employment, few options exist for alternative day activities. However, some other options may be provided with the use of Companion Services or Non-Residential Support Services. A non-waiver option that an individual may choose to pursue is participation as a volunteer in a community service setting. Companion Services. An individual who lives in his/her own home, foster home or family home may receive companion services – either in the home or while engaged in a community activity. Companion service is defined as non-medical care, supervision and socialization provided to an adult on a one-to-one basis. Acceptable companion activities might include going to the library, getting a library card, checking out books or videos, shopping for groceries, going to an animal shelter to learn about animals and, volunteering or assisting at the animal shelter. These activities are not merely diversions, but relate to a goal or outcome desired by the individual. 3034 individuals received these services in 2000-01. Non-Residential Support Services. This service consists of individualized training activities for an individual in an integrated, nonresidential community setting. These services are concerned with: 1) developing communication and social skills to assist the person to 53 function with maximum independence in the community; 2) developing the skills needed to increase independence in the community; and 3) developing the skills needed to maintain a living environment, use community resource and conduct activities of daily living. Older individuals may be interested in using this service to attend senior citizen programs or licensed adult day care centers. 3499 individuals received these services in 2000-01. An Overlooked Employment Resource: National and Community Service Programs. Individuals who choose to participate as members in AmeriCorps and Senior Corps programs (which exist across the state) have the opportunity for further community integration, the chance to contribute to their local communities, a way of developing work skills and exploring job possibilities, and exposure to potential future job contacts. In addition, full time members receive a living stipend and an educational award, which can be used for training or education at any accredited school in Florida. This little known opportunity can be an excellent means of exploring a field of employment. These programs also emphasize the inclusion of persons with disabilities in their programs. Since access to the community, and to the many resources available to the general public, is of vital importance to individuals who have disabilities, we now turn our attention to the core area of transportation. D. TRANSPORTATION SERVICES Accessibility and availability of transportation remains an obstacle for many people with disabilities, in getting to work and into the community. The National Organization on Disability (NOD), reports that the transportation gap for people with disabilities has grown over the past decade. It continues to be a factor militating against community inclusion. In addition to rides provided by family and friends, transportation services for people with developmental disabilities in Florida usually consist of paratransit trips provided via city and county governments, private transportation providers, and disability service providers. Different funding sources cover the costs of the trips, depending upon the purpose of the specific trip. For example, Medicaid covers medical trips; Medicaid waiver covers supported employment trips; DVR may cover trips for training/education, etc. Some trips may also require fees to be paid by the individual (e.g., for community outings). Transportation Disadvantaged System. Florida has a coordinated system of transportation, mandated by F.S. Chapter 427, for residents who are considered transportation disadvantaged (TD). Each county or area of the state has a county transportation coordinator (CTC) who is responsible for arranging or providing the trips in that county. This TD system provides publicly funded services to eligible people who are 54 elderly (35%), children under age 16 (20%), have disabilities (22%) or have low incomes (18%). A disability is considered to be any physical or mental impairment that substantially limits at least one major life activity. TD providers do not identify the type of disability of the people they serve. As a result, it is not possible to determine how many of the total number of people with disabilities who are served have a developmental disability. Local coordinating boards hold regular public meetings as part of their oversight role to determine how effectively local transportation needs are being met. Written complaints about transportation are documented by the TD Office and forwarded to local CTCs for investigation and response. 49 Community Transportation Coordinators, who serve all of Florida’s 67 counties, coordinate the system and report to the statewide Transportation Disadvantaged Commission in Tallahassee. The mission of the Commission is to ensure the availability of efficient, cost-effective and quality transportation services for individuals who are transportation disadvantaged. Chapter 427 also established the TD Trust Fund, as one source of funding for the system. The $271million in total 2001 funding for the TD system emanated from many different federal, state and local entities. These include: Commission for Transportation Disadvantaged (9%); DCF, includes DDP, (11%); AHCA (30%); Department of Transportation (5%); Department of Elder Affairs (3%); DOH and DOE (4%); and, local governments (38%). As can be noted, local governments and Medicaid (AHCA) support 2/3 of the TD program. Services Provided. TD statistics are kept according to the calendar year. During 2001, a statewide total of 51.5 million one-way trips were provided to 654,432 people. 5.7 million one-way trips were provided to 155,000 people with disabilities. 29% of the trips were for medical purposes, 16% for employment and 23% for education or training. There were also more than 1.5 million trip requests from all callers that could not be met in 2001. Current Transportation Issues. Transportation services vary greatly among Florida’s 67 counties, of which nearly ½ are rural and lacking in mass transit. In those counties where paratransit services do exist quality and consistency of service are major issues. At local TD Committee meetings, riders with disabilities complain of late pick-ups, unconscionably long delays for return trips, rude and uncaring drivers and unresponsive call center staffers, and virtually non-existent services during evening and weekend hours. In some areas, calling systems are difficult to use by people with disabilities and long waiting times on the telephone are not uncommon. New drivers, unfamiliar with area or with local directions are common, due to frequent turnover in staff. 55 Despite the need of a consumer to get to a medical appointment, an employment related activity or a long-anticipated community event, services do not extend to all areas of all counties at all times. Nor, generally, can trips be scheduled to cross county lines for any reason. These restrictions on community participation and everyday life severely limit persons with no other means of transportation. DDP/AHCA Transportation. As noted above, paratransit trips provided through funding from all federal, state or local sources, i.e., the DDP and AHCA, are included in the statewide TD statistics. Eligibility for those transportation services is based upon the individual’s disability and participation in the DDP Medicaid waiver program or receipt of services under the Medicaid State Plan. Individuals with disabilities may receive additional transportation services not covered under public funding by meeting the criteria for disability and income used by their local CTC, and paying a sliding scale trip fee based on income. Individuals must have no other means of transportation and be unable to use public transit. In many areas of the state, the DDP provides funding for transportation services for individuals with disabilities via contractual arrangements with disability service agencies to transport the people to and from their service facilities. These providers are considered coordinated contractors by the CTCs. However, should an individual require a type of trip that is outside of the contractual arrangement of that particular provider, the CTC becomes the transportation provider, using one of its own or a subcontracted operator for the trip. WAIVER TRANSPORTATION SERVICES PROVIDED For 2001-02, 10,267 individuals received transportation services under the DDP Medicaid waiver. Mass Transit. Most urban areas have mass transit systems, which vary in their accessibility and “user friendliness” for persons with disabilities, though some provide rider assistance. Barriers Identified. The barriers identified in the Jacksonville system are typical of other metro areas and are used here as examples. In a 1997 report, the Jacksonville Community Council found the top priority transportation needs for people with disabilities are getting to medical appointments and employment related services. They also identified several barriers to using local public transportation. Those that are specific to individuals with developmental disabilities include: 1) Some people who have mobility impairments are unable to get to a bus stop due to its location, lack of sidewalks, lack of curb cuts or because they cannot safely cross busy streets to reach the bus stop. 2) Individuals who have access to the bus system may learn to use it, but only 56 after intensive training. Even then, some are easily confused by a bus break down or a missed connection. Special assistance from bus drivers is sometimes needed. Additionally, many guardians of individuals are reluctant to allow them to walk long distances to reach the bus stops. 3) Differing eligibility requirements cause confusion for individuals whose transportation can be paid by multiple funders. As a result, some individuals find the TD system difficult to use and may not use it at all. [Note: Recommendations for specific transportation barriers identified by focus group participants will be detailed further in Part Two of this report.] Mobility Training and Bus Passes. The following Florida counties offer special assistance to riders who have disabilities: Alachua County – The Center for Independent Living works with the regional transportation system and offers a mobilitytraining course. Broward County – The Transit system has a full-time travel trainer available. Duval County – Jacksonville Transportation Authority opened a new ADA Mobility and Training Center on 4/01/03. Escambia County – Offers mobility-training to anyone needing assistance using fixed route services. Hillsborough County – Has a mobility-training program available upon advance request. Leon County – Has a bus accessibility-training program conducted by the Florida Institute of Rehabilitation Education and the Leon County School Board. Miami-Dade County – Miami-Dade Transit has a travel mobilitytraining program that orients riders on how to use the fixed route service in the county. Orange County – Has two mobility-training programs; one fixed route, one paratransit. o The fixed route program (LYNX) has an in-house trainthe-trainer program aimed at training counselors/instructors how to train others with “How to Ride LYNX.” This a 4-6 hour program focused on training how to read schedules, time points and maps, as well as safety issues and fares. It teaches how to obtain special IDs and provides a hands-on bus ride for trainees. o The Access LYNX program is a travel training program set up as part of this paratransit system’s functional assessment of potential riders. It is also available on request for existing paratransit riders requesting more assistance. o Pasco County – Has staff available to do mobilitytraining. 57 o Pinellas County – Has a ride buddy program to teach new riders to use the system. COMMUNITY AND FAMILY SUPPORTS Two recent disability surveys—a 2000 NOD/Harris Poll on Community Participation and the 2001 federal National Health Interview Survey— confirm the fact that there are serious gaps in participation in community life between people with and without disabilities. Overall community participation is, naturally, related to time spent away from home each day. Surveys reveal that people with severe disabilities spend an average of two hours less per day out of their homes than people without disabilities. That gap is to 4.5 hours per day for people with disabilities who are unemployed. Fully 40% of people with severe disabilities are not at all involved in their communities, almost twice the percentage for people without disabilities, and one and one-half times the percentage for people with less severe disabilities. These lower participation rates have varying causes of emotional hurdles such as fear or perceived negative attitudes, more practical hurdles such as lack of transportation, or most importantly, the lack of encouragement from community organizations. In general, only 33% of people with disabilities say they are very satisfied with their lives. There are a number of ways that people with disabilities can stay connected with their communities and with the larger world. Use of these methods was queried in these national surveys. The Internet. The Internet has had a dramatic impact on the quality of the lives of people with less severe disabilities, allowing them to extend their reach to others, to become effective advocates and to be better informed about the world. However, this electronic marvel has not yet become accessible or user-friendly for people with severe disabilities. Regarding satisfaction with community involvement, almost half express that they are dissatisfied with their community experiences. Of that total, 23% are not at all satisfied. On a related note, people with disabilities also express a greater sense of detachment from their communities. People with disabilities are one and one-half times more likely to say they feel left out of things in their communities. Those with severe disabilities are more likely to confront obstacles such as transportation or communication issues, making the community less accessible to them. Only 29% of people with severe disabilities say they are regularly invited to give their opinions on important community issues. Specific Community Activities. 81% of people with disabilities say they never go to community service organizations, either to attend activities 58 or to avail themselves of the organizations’ services. Also, more than 52% of people with severe disabilities never attend religious services. Almost four out of ten people with severe disabilities never attend cultural events or organizations such as the library, theater, ballet, opera or museums. A similar gap exists for attendance at outdoor community places such as the beach, or park. Only 44% of people with disabilities go to these places at least once a month. This may not be surprising for people with physical disabilities, since it involves some sort of physical activity, which may be prohibitive. In addition, 56% of people with severe disabilities never volunteer in their communities. However, the largest gap in community participation for people with and without disabilities is found in going to entertainment. Only 32% of adults with disabilities report going out to shows, movies, sports events or club meetings. The smallest gap is for socializing with relatives and friends, either in person or by phone. Many people with disabilities are able to socialize on a regular basis, like their counterparts without disabilities. The U.S. Department of Health and Human Services (HHS), Office of Disease Prevention and Health Promotion, is concerned about the level of community participation and life satisfaction that is experienced by people with disabilities. They understand that barriers to social participation and access to the community impact health, and have included goals to reduce these barriers in Healthy People 2010. Within the general goal to, Promote the health of people with disabilities, prevent secondary conditions and eliminate disparities between people with and without disabilities in the U.S. population, HHS include suggestions for a number of activities to increase access to community health and wellness programs and to bring assistive technology and devices into the reach of all who need them. Public and Privately Funded Resources. Throughout Florida, there are a number of programs and activities sponsored by city and county governments in which adults with disabilities regularly participate. These athletic events, leagues, classes and social activities may be either targeted to the disability population or integrated aspects of general community events. Such activities are usually quite popular and well attended (see details in Part Two). Other disability-specific organizations that are partly supported by public funds, such as Special Olympics and Best Buddies, offer year round activities for individuals and groups of persons with disabilities. Certain civic and community organizations are sponsors of annual disability events that are popular with individuals and families alike. Religious organizations welcome members with disabilities to participate in their programs and worship services, often by playing integral roles in these ceremonies. Such organizations also sponsor classes and social outings, summer camps and other activities for children and young adults with disabilities and their families. Certain specific recreational activities such as sailing, swimming with dolphins 59 or horseback riding exist solely for people with disabilities and often have months’ long waiting lists. Family Supports. In addition to those resources previously mentioned in this report, there are several publicly funded entities that exist to provide supports to families in their attempts to successfully navigate the disabilities service system. These include the 15 Family Care Councils that exist in each DCF district/area that inform and conduct educational outreach to families. These volunteer groups receive funding from the DDP to support their activities. The DDP also provides an electronic E-Bulletin to 700 individuals and families, as a means of keeping them abreast of system activities and to provide answers to questions from families. The DDP web site is also a source of information for those concerned about services for people developmental disabilities, and includes a link to the AHCA site for information about Medicaid and the waiver. The ASCEND Project of the Family Network on Disabilities (FND) is also a source of information for families, with its newsletter, web site and toll-free information line. This project, which is underwritten by the DDP, also provides periodic workshops around the state to support families and self-advocates. POTENTIAL OBSTACLES TO SERVICES #1) #2) #3) #4) #5) #6) #7) Two services, ADT and Res Hab, comprise more than 50% of the waiver budget The funding for ADT is nine times that for SE, to serve four times as many people Funding for more independent services, SE and SL, is not increasing Nearly 11,000 people are currently on the waiting list for the Medicaid waiver AT is very expensive and resources to subsidize or obtain needed devices are few There is a shortage of affordable, accessible housing in Florida Support coordinators and SL coaches must become familiar with housing resources In this section we reviewed the services available in three major adult life areas – living arrangements, employment and day activities, and transportation, as well as community and family supports. The concluding section in Part One presents an overview of the unique service needs of older adults with developmental disabilities and their families. 60 IV. SERVICES FOR OL DER ADULTS Some Florida Aging Demographics. Twenty-three percent of Florida’s population (more than 3.6 million people) is over the age of 60. People who are 75 and older make up 9.2% of the population and will be close to 10% by the year 2010. Florida has more elders than 17 other states and the District of Columbia combined. Persons aged 100+ are the fastest growing age group in the state. This population of elders will all age differently. Some have lifelong disabilities or chronic conditions that occurred before age 60. Others are beset by agerelated impairments. Still others live their whole lives without the need for long-term medical or social services. OLDER ADULTS WITH DEVELOPMENTAL DISABILITIES The previous sections of this report discussed those services that are available to individuals from childhood, to school years and through adulthood. We now turn our attention to the unique needs of older adults. Services needed by, and available to, older adults are very similar to those discussed in the prior section, Services for Adults. However, the emphasis differs, in that at least three of the core life areas served primarily by the Medicaid waiver—health, housing and day activities—often change with the onset of old age. The factors affecting this shift in emphasis may be either intrinsic (within the individual) or extrinsic (circumstances surrounding the individual). Intrinsic Factors. One simple caveat that bears remembering here: Some older people with developmental disabilities, primarily those with Down Syndrome and individuals with severe, multiple disabilities, age earlier than their chronological years. Research has shown that men with Down Syndrome can age as much as twenty years earlier than their non-Down’s counterparts; women may age ten years earlier. People with Down Syndrome also develop Alzheimer’s Disease at an earlier age and at a rate as much as 40% higher than others. Research is still ongoing to determine all of the effects of aging upon individuals with cerebral palsy. To date it is clear that many secondary disabilities can compromise the health, communication and mobility of persons with CP. For these reasons, it is not uncommon to consider that people with severe developmental disabilities become “older adults” in their 50s. Once that acknowledgement is made, appropriate adjustments in outcomes and services should also follow for individuals of that age. Extrinsic Factors. It is well known that the majority of individuals receiving publicly funded services in Florida continue to live at home with their families. Parents of people with disabilities frequently accept the role of being a lifelong caregiver, providing myriad supports to the individual over the course of a lifetime. Once individuals with 61 disabilities enter their fifties, their parents are often in their eighties. When the vicissitudes of old age become a reality for these elderly parents, their own resources are no longer adequate to continue in the caregiver role. As a result, they turn to the service system for help in planning the transition of future care to others. Areas of Need. Among the changing life areas of older adults with disabilities to be considered in this section are: health care, residential needs, in-home supports, daily life activities, and transportation. The primary public service agencies presented in this section are the DDP, AHCA, TD and the Department of Elder Affairs (DOEA). Other locally funded public resources will also be referenced, since many aspects of the Aging Network that are available to the general older population are also available to older people with developmental disabilities. A. HEALTH CARE SERVICES While the population of individuals with mild disabilities generally ages at the same rate as non-disabled persons, it is individuals with more severe disabilities that are more apt to be receiving services from the DDP. The tendency of this latter group to show early signs of aging is further compounded by the onset of normal aging changes and agerelated disabilities. Furthermore, the ability of an older individual to provide informed consent for health care now becomes more of an issue, as the frequency of health care encounters increases with age. Healthy lifestyle choices also become more critical for older adults. The obtaining of guardianship or guardian advocacy by parents to protect the rights of their offspring with disabilities is commonplace today, where admonitions to do so emanate even from the school systems. However, 30-40 years ago, this was not always the case. Parents often eschewed the option of legally removing all of their children’s rights, and this was the only legal choice available when many of today’s older adults came of age. Further, in years past when adults with disabilities lived with their parents, family physicians widely accepted parents’ substitute consent for health care and treatment. It in only in recent years that greater accountability and insistence upon informed consent by the patient or his/her legally appointed guardian became standard operating procedure for health care professionals. Beyond that, the philosophy in institutional care that prevailed 40 years ago caused many parents of then-young adults to mistrust the disability system and avoid signing any legal documents. With that historical background, it is easy to understand why a number of older adults who are unable to independently exercise their own rights and give informed consent are still lacking legal guardians. Older parents must be encouraged to obtain either guardian advocacy or guardianships for their older adult children, and simultaneously appoint one or more successor guardians. 62 The Department of Health (DOH). The various aspects of the DOH described in the previous section as being available to adults with disabilities pertain here as well. However, the DOH programs more likely to be used by older adults are based in primary health clinics, which have geriatric specialties in some counties. However, as a general rule, these clinics (and other DOH programs) do not keep statistics on the types of disabilities presented by the people served. The Developmental Disabilities Program (DDP) & AHCA. All of the services described in the prior section for adults—particularly the DDP Medicaid waiver—will also be relevant for older adults, with a different emphasis in needs, due to aging. Basic health care may continue to be provided under the Medicaid State Plan for primary and specialty physicians, hospital in-patient and out-patient treatment, prescription coverage, hearing aids and glasses. Waiver services may take on a different emphasis for aging individuals, with perhaps a greater frequency and level of intensity required for certain types of care and supplies. Major health issues for adults living in the community are proper nutrition and sufficient exercise. Obesity is higher among this population than it is in general. Health monitoring, and services dieticians, are essential from to help older adults live healthier lives as they live longer lives. (The role of the Aging Network in providing additional, health-related services will be detailed below under day activities.) B. RESIDENTIAL SERVICES According to AAMR, there are an estimated 526,000 adults aged 60 with developmental disabilities, nationally. This number will double by 2030, to more than 1 million, when all of the baby boom generation reaches their sixties. AAMR also cites a recent national survey that reports 60,876 people with disabilities on waiting lists for residential services in 37 states. As adults age, there is a growing need for housing options outside of the family home. AHCA & DDP Services. The most common, universal fear of elderly parents is the uncertainty about the future care and well being of their loved ones with disabilities. This is particularly true for older adults who have spent their lives with their parents in the family homes. More often than not, future care plans and residential arrangements are tentative or non-existent. As their own lives shorten, some aging parents may look to immediate group home placements as solutions to their concerns. Usually they are not aware of the various options that they and their adult children might have. One way for parents to assure future care and living arrangements for their children is by using a supplemental or Special Needs Trust. They should be apprised of the need to seek the assistance of an attorney who is knowledgeable in 63 disability law to assure that this trust is properly established. Parents without a large estate may be unaware that such a trust can be funded with the proceeds of their life insurance, for example. A properly drawn will direct such proceeds to the trust. Given complete information and support, parents might well opt to leave the family home as their child’s future residence, with the appropriate safeguards in place to assure permanence of residence, supported living and in-home services, and a roommate to share expenses (if desired by the person), upkeep and maintenance. Funds for supplemental activities/needs can be provided to the individual from the trust without impinging upon his/her Medicaid waiver eligibility. Information about alternative residential options should also be considered. The urgency for elderly parents to make written future–care plans should be acknowledged, and their efforts guided by using existing tools and formats for such purposes, such as those that are available on the websites of The Florida Developmental Disabilities Council and of The Mailman Center. Certainly, the role of a supported living coach and the importance of in-home supports can not be overestimated when these services can enable an older adult to remain in a familiar, lifelong home. Related Services. Another waiver service that may attain greater emphasis with the increasing age of the individual is Environmental Accessibility Adaptations. Ramps, grab bars, bathroom modifications, etc, may become more important in allowing the older person to maintain his/her independence in the community home. Other Resources. While an older adult may certainly wish to make use of the same community housing resources as a younger individual (such as Section-8 vouchers, etc.), the existence of public housing that is specifically available to older people should not be overlooked as an option. In addition, the same private housing resources made available by groups of parents should be explored as possible residential choices for older adults. C. DAY ACTIVITIES The previous sections of this report discussed several employment options available for children transitioning from school and for adults. Though some may wish to continue working, even on a part-time basis, most older adults will choose to retire from the world of work to enjoy other day activities. This life area marks the greatest change in service emphasis, just as the arrival of the retirement years makes a similar life change in the population at large. AHCA &DDP Services. As individuals with severe disabilities decline 64 in function as they age, the use of waiver services such as assistive technologies and environmental accessibility modifications take on even more prominence, in assuring continued community independence and participation. From the aspect of specific day activities, some of the ADTs discussed in the prior section include social or community programs for older adults who seek a non-work option for their day activities. Such “senior activities” commonly include participation in local community senior resources, some of which belong to the Aging Network. Department of Elder Affairs (DOEA). DOEA is the agency that administers human service programs to help elders keep their selfsufficiency and self-determination. It also has the primary responsibility for developing policy recommendations for long-term care. The majority of programs administered by DOEA are privatized, with services being provided by not-for-profit agencies and local governments, under contract through the state’s 11 Area Agencies on Aging (AAA). Funding for these programs, which are often referred to as the Aging Network, are a combination of federal, state and private funds. Following are the descriptions of the major DOEA programs of interest to persons with developmental disabilities. Older Americans Act Services. The federally funded Older Americans Act (OAA) provides a variety of services to all people ages 60 and older, targeting individuals in the greatest economic and social need. The services include adult day care, information and referral, medical transportation, shopping assistance, counseling and congregate dining. Many of these services emanate out of senior centers and nutrition sites in local communities. Using supplemental local funds, centers also provide a variety of social and leisure activities, from arts and crafts to classes in exercise, dance, cooking, etc., and day trips and excursions. The range of activities generally offers options for individuals on several functional levels, from frail elders to healthy and energetic older people, and all those in between. These activities can also be of great assistance to older individuals in maintaining healthy lifestyles. OAA Eligibility Criteria. Because they are open to anyone who has attained the age of 60, Senior Centers and Adult Day Care Centers can often be appropriate choices for older individuals with developmental disabilities. Furthermore, OAA guidelines also allow the dependent adult child below the age of 60 to participate in the congregate dining program when both the over-60 parent and adult child attend the center together. Another way for a person below 60 to participate is by providing voluntary assistance at the center. OAA services also include in-home services like homemaker, chore, and personal care as well as home delivered meals. However, there is often a long waiting list for in-home services, due to the high demand from the oldest elders. 65 DOEA Waiver Programs. While any individual can only participate in one waiver at a time, DOEA also operates several Medicaid waiver programs aimed specifically at keeping frail, homebound individuals out of institutions. These waivers were mentioned earlier in this report and include: the Aged/Disabled Adult Waiver for those aged 65 and older, or adults with other disabilities; the Channeling Waiver in MiamiDade and Broward Counties for those aged 65 who meet the nursing facility level of care; the Nursing Home Diversion Waiver which is a pilot program for those 65 and older who are eligible for Medicaid and Medicare and live in certain areas of the state; and, the Assisted Living for the Frail Elderly Waiver for persons age 60 and older who are at risk of nursing home placement and meet additional specific functional criteria. This waiver provides extra support and services to individuals residing in certain assisted living facilities. Waiver Eligibility Criteria. Waiver services are available to individuals who meet the financial requirements for Medicaid, as well as the age and functional levels specific to each described waiver program. [Note: DOEA waivers use a case management model to coordinate and plan services for recipients, versus the DDP model of support coordination. The role of a support coordinator has expanded responsibilities and greater accountability to recipients, particularly for advocacy.] Other DOEA Programs. The other major programs administered by DOEA include: 1) Community Care for the Elderly, which provides inhome services for those aged 60 and above who are functionally impaired. Primary consideration is given to persons referred from Adult Protective Services. 2) Home Care for the Elderly, which provides services to very low income persons over the age of 60 who are at risk of nursing home placement and who have a willing adult caregiver; 3) Emergency Home Energy Assistance for the Elderly, for households with at least one member over the age of 60, that also have a heating or cooling emergency and incomes no more than 125% of poverty guidelines. DOEA also sponsors other programs for specific elders, such as the Alzheimer’s Disease Initiative, which offers diagnostic services, respite care and targeted day care services for individuals with this condition, and training for their family caregivers. DOEA also participated with the DDP in the Robert Wood Johnson Consumer Directed Care Project. Other Community Aging Resources. Senior adult resources are likely to be found in any Florida community, both large and small. These ubiquitous programs may be identified as senior centers, adult day care centers or nutrition sites. Some of these are sponsored by DOEA funds, as noted above. Others, held in community centers or private facilities, may be supported by city or county governments or by private funds or sponsored by civic, charitable or religious organizations. Any 66 with disabilities, to and all of these centers are resources that are available to older adults further their personal goals of increased participation in social and leisure activities of the community. DOEA SERVICES PROVIDED During 2001, there were 114,000 elders who received services at senior centers and other senior focal points in their communities. In the same year, an additional 133,000 frail seniors received in-home services of some type. Though DOEA does not track types of disabilities, 39,238 frail seniors are identified as having a disability. C. TRANSPORTATION SERVICES As with many of the other needs described in this section, as adults age their need for assistance in getting from one place to another in the community increases. Thus, the provision of waiver transportation service likewise increases in prominence in their hierarchy of needs. As with all age groups, information about the transportation provided to older adults is captured by the TD system. However, it is not tracked by disability type. SERVICES PROVIDED TD statistics show that more than 18 million riders on publicly funded transportation during 2001 were elders. Of that total, 3.8 million are disabled and another 2 million are disabled and low income. Not unexpectedly, rides to older adults comprised 35% of the total trips. POTENTIAL OBSTACLES TO SERVICES #1) #2) #3) #4) #5) #6) There are few flexible options for day activities for older adults under the waiver Elderly parents are often no longer able to provide care for their adult offspring Older parents should be informed about how to make formal plans for future care Obesity and insufficient exercise are health problems of older adults with disabilities There is a lack of residential options appropriate for older adults with disabilities. Geriatricians are not trained to provide health care to older adults with developmental disabilities. …………………………… This concludes Part One of this report. Part Two presents the study’s conclusions and recommendations, including input received statewide from individuals with developmental disabilities, their family members, and disability professionals. 67 PA R T T W O C ONCLUSIONS AND R ECO MMENDATIONS I. INTRODUCTION A. Summary of Part One. The first part of this report presented a description and analysis of the publicly funded services available to individuals with developmental disabilities in Florida. This information was given chronologically, with four different sections focusing on: 1) Services Available to Children; 2) Services for Children Transitioning from School; 3) Services for Adults; and, 4) Services for Older Adults. Each section discussed the areas of greatest need during that life period, presented the primary service agencies that meet those service needs, and, detailed the types and amounts of services delivered. Program eligibility criteria and methods of assuring quality were also described. Some obvious service gaps or obstacles were listed, and further details about these issues are presented in this part of the report. Quantity of Services. The following chart displays the services that accounted for the majority of expenditures in the DDP waiver for 2001-02. Five Services Account for Over 3/4 of Waiver Expenditures 2001-02 Res Hab Other 27% Res Hab 40% Per. Care 8% Per. Care Trans. Supp Coor 8% Trans. 4% ADT Supp Coor ADT 13% Other Of those services in the “Other” category, SL is 4%; SE is 1% and InHome Supports account for 4%. Companion and Respite are 2% each, while Non-Residential Support Services is 3%. The remaining 13% of expenditures are comprised of all other waiver services, which generally are less than 1% each. B. Purpose and Description of Focus Groups. In addition to the gathering of quantitative service data, The Council directed that this report should also contain the qualitative findings of three 68 focus groups, held in different geographic areas of the state. Participants in these groups were individuals with disabilities, family members and service providers. Focus groups are a particularly useful method of gathering information, since they: Can elicit the shared meaning of everyday experiences from participants Capitalize upon the synergy created among the members of the group Produce information that is difficult to obtain in individual interviews Emphasize participants’ interactions and other points of view Provide opportunities for participants to validate information from others Clarify arguments and reveal diversity in perspectives, and Enable the collection of large amounts of information in a relatively short time. The three focus groups conducted for this report consisted of the following membership and locations. 1) The first meeting was held on October 16, 2002 in Winter Park (Central Florida), with 18 members of the District Seven Family Care Council. Fifteen respondents are parents or family members; three are people with disabilities. The parents and family members present range in age from 58-81. The individuals with disabilities they represented range in age from 30-56, with half in their thirties. 2) The second meeting was held on November 21, 2002 in Miami (D11, South Florida) with 14 members of the local People First chapter, a self-advocacy group for persons with disabilities. The group was evenly split between males and females, who have retardation, CP or autism. Their ages range from late twenties to 50. 3) The third meeting was held on January 28, 2003 in Jacksonville (D-4, North Florida) with 12 providers. Three of these 12 Waiver Support Coordinators are also parents of people with disabilities (two adults and one school-aged child). Providers have a range of service experience from 1.5 -7.5 years, with an average span of five years. The 44 total focus group respondents included persons who are White, Black, Hispanic and East Indian. Various disabling conditions were also represented in the three groups with retardation, CP, autism, epilepsy and multiple disabilities listed. Each focus group was limited in size, to allow maximum participation. Respondents volunteered their personal knowledge or described their own experiences in response to a series of formal questions. (These questions were repeated for each group.) Successive respondents voiced either agreement or different perspectives, 69 producing a variety of opinions and information. Sessions lasted an average of 1.5 hours. Each session was tape-recorded and a verbatim transcript produced. Themes experiential episodes and illustrative quotations were derived from each transcript. The barriers identified and the recommendations made in the three groups are included here. C. Purpose and Descriptions of Surveys Distributed. In addition to the required three focus groups, The Center also prepared and distributed anonymous surveys to individuals with disabilities, family members and providers, asking essentially the same questions that were used with the focus groups. These surveys were distributed at random by project staff to participants at various state and regional meetings, that were conducted during the last half of 2002 and the first quarter of 2003. The purpose of these surveys was to expand the information collected to include data from other areas in the state, not represented in the focus groups. Fifty-four surveys were returned. Of these, 39 were from family members or individuals; 15 were from providers. Between surveys and focus groups, a total of 98 stakeholders contributed data for this report. Opinions of individuals from DDP districts 4, 7 and 11 were obtained in the focus groups. Additional information was provided by the surveys received from individuals in districts/region 2a, 3, 4, Sun Coast, 7, 8, 9, 10, 11a, 11b, 13, 14, 15, and 23. This widespread distribution is helpful in determining whether the service improvements observed, the service barriers identified and the recommendations made are statewide in nature or specific to certain areas of the state. I I . G E N E R AL R E S P O N S E S TO F O C U S G R O U P S AN D S U RV E Y S A. Observations about Recent Service Improvements. Focus Group participants differentiated their responses to this question by describing service aspects of availability, access and quality. Unanimous opinions across the three focus groups declared that service availability has greatly improved over the past two years, also improving the lives of many consumers. Factors listed as contributing to this increase include: energetic support coordinators; more people being served on the waiver; the CDC pilot program; increased commitment of the individuals involved with consumers; and, a greater variety of services that promote community inclusion. The vast majority of survey respondents also report improvement in the amount of services available over the past two years, confirming that this is a statewide phenomenon. Similarly, both group and survey respondents agree that, with some exceptions, there is a greater access to services now than in the past. Consumers and 70 families see the contributing factors as both an increase in the number of service providers and improved information dissemination efforts by the DDP and Family Care Councils. Providers cite the existence of more service providers, especially those requested by consumers, and an increase in the amount of funding for services. However, despite these improvements, both groups mention that there is still a shortage of certain service providers. Families name dental care, speech therapy and some transportation services; providers list a shortage of therapists, personal care and companion agencies, as well as transportation and dental services. In rural areas these shortages are exacerbated and include a scarcity of residential options. Furthermore, support coordinators, in both groups and surveys, also describe systems problems and relate how the process of obtaining services has been lengthened, especially with the addition of prior service authorizations. They relate that while the lives of the consumers they serve have improved, as a whole, their jobs as support coordinators have become more difficult and frustrating. B. The Quality of Services. The issue of service quality evoked decidedly mixed responses from both group and survey participants. The overwhelming sentiment seems to be that while the issue of availability is being positively addressed, it is time now to focus on the quality of services offered. Families note an inconsistency of service quality, often from large multi-service agencies, where one service is very good and another poor in quality. Group homes, ICF/DDs and some Res Hab providers got high marks, particularly for their efforts in community inclusion. ADT providers received the most criticism from families, who cite well meaning but poorly trained staff with constant turnover. As a result, many programs are no more than “baby sitting services,” where consumers learn few if any skills, in the estimation of several family members. Transportation services statewide are also cited as being inconsistent and undependable, whether offered by paratransit providers or disability agencies. Providers voice concerns about the quality of transportation, with inadequate and unreliable service for vulnerable consumers. Consumers report poor service quality in transportation, especially for work and for community activities. They also say they do not receive consistently good quality services from personal care workers and in some group homes. The latter venues suffer from high staff turnover and an inability to keep “…good staff, who know about me.” They also point to the poor quality of most Res Hab services, where individuals receive inadequate or no training to live more independently. Similarly, they report that ADT programs lack any consistent programs that are directed toward the individual consumers’ planned goals. Here too, high staff turnover rates, inadequate training of staff and a lack of accountability by service providers are cited as factors. In general, survey respondents made 71 the same sorts of comments about the quality of services, particularly emphasizing extreme inconsistencies in transportation services. C. Satisfaction with Non-DDP Services. Focus group participants limited their discussion of services primarily to formal DDP services. They did describe informal supports and community resources. These will be detailed further below. Survey participants mentioned a number of publicly funded services and their degree of satisfaction with them. Among these are the DOE. In general, providers and parents of school-aged children responded to services from the school system as varying by school district. Comments included “very good,” “satisfied,” and “varies,” to “some services are still an area of contention” and “…not happy with the services.” For adults, satisfaction is good for ABE classes and community instructional programs. Department of Education, Division of Vocational Rehabilitation (DOE, DVR) is another public entity whose services varied, but responses are more negative than positive. Some examples: “services are limited,” “not satisfied, very poor,” “don’t deliver what they say…unhappy with them,” and “Change the requirement to go through DVR first. In some areas (D-3) they don’t serve our clients.” Yet, in one county (D-10), DVR transitional services are rated more favorably: “DVR has been very cooperative. They provided postsecondary educational services and my clients are very happy.” The same provider then notes that, “I’m very satisfied with DVR services for students with mild to moderate disabilities that do NOT require long-term follow-up.” Conversely, another provider in that same district cites problems in obtaining appropriate transition services. Whether this is an issue with a particular school or with that district’s DVR staff is not clear. Department of Health, Children’s Medical Services (DOH/CMS) also received varying ratings from some respondents. These include, “very good” and “sometimes happy with therapies…other times not.” DCF/ADM received two accolades from providers who are satisfied with community mental health services, while a third provider notes difficulty in making connections between the severely emotional disturbed (SED) program and the DDP. D. Satisfaction with Community Resources. Enthusiastically, participants in both the family members’ and self-advocates’ focus groups discussed their general satisfaction with the social, recreational and community resources in their local areas. Whether the individuals with disabilities live in family homes, in supported living arrangements, in group homes or ICF/DDs, there has been a tremendous increase in community participation. Most families and advocates live in the Miami or Orlando areas, but some in Central Florida live in smaller suburbs or rural areas. Naturally, the resources named by members in the two groups vary across and within 72 counties, but they are representative of the types of resources and community experiences that people with disabilities are now enjoying in apparently increasing numbers. A few of the community resources cited by group participants include the general: art classes that are open to all in the community, a statewide, church-sponsored clogging group, community bowling leagues, performing designated roles in church/religious services, volunteering with Habitat for Humanity, square dancing, church choirs and holiday caroling, swimming teams, equestrian clubs, boating trips, picnics, college football games and Friday night dances. Some of the disability-specific community activities in which individuals participate include: Best Buddies, both individual and group activities; agency-sponsored trips to theme parks; Special Olympics; parties sponsored by churches and civic groups; dedicated outings and activities sponsored by city recreation departments. Other activities include disability advocacy roles, such as participation on a local human services coalition and a disadvantaged transportation committee. One caveat accompanied about the lack of transportation the enthusiasm: Without the availability of parents or the willingness of agencies to transport individuals, there would be few opportunities for community participation. During evenings and on weekends, paratransit services are rarely available or, if available, are very undependable. Nonetheless, several parents aver that their adult children have busier social lives than they do. Some report that their offspring do not want to come home on weekends now, for fear they will miss a favorite activity. While some parents have regularly fostered community participation over the years, it is clear now that there are many more community activities in which their children participate and to which they are welcome. The worry—What happens when they are not there? III. SPECIFIC RESPO NSES FROM FOCUS GROU PS AND SURVEYS A. Service Obstacles and System Problems Identified. While a number of service problems were identified earlier in this section, it is clear that for a number of services there are completely different perspectives. Therefore, the identified service problems that follow are those that are repeatedly identified in more than one area of the state. That is, these are statewide service obstacles rather than local ones. #1. ADT programs do not provide skills training or otherwise further the goals of the individuals receiving these services. 73 #2. Res Hab services do not provide adequate training for the individuals receiving this service to live more independently. #3. Direct support staff in both of these service settings have very high turnover rates, inadequate pay and are not well trained or held accountable for providing the required services. #4. The van transportation typically available to group home residents often mitigates against individual choice, since the priority needs of one or two residents will limit the use of the van. #5. Paratransit transportation is sometimes not available and often unreliable, to the point of jeopardizing the health and safety of its more vulnerable riders. #6. Statewide, there is a serious lack of dental care providers who are familiar with and available to treat individuals with disabilities. #7. It is extremely difficult to develop an SE follow-along plan for students who are not on the waiver. #8. There is a lack of available companions and PCAs to assist consumers who wish to become or remain living independently in the community. A number of systems problems that deal primarily with the administration or implementation of the DDP Medicaid waiver were also identified by both focus group participants and survey respondents. These systems issues include: #9. The size and time of delay on the waiting list is a source of frustration for many families and individuals who are now unserved or underserved. #10. In at least two districts, DDP case managers discourage families from applying for the Medicaid waiver since they are not “in crisis.” #11. There has been a fourfold increase in the paperwork process for obtaining services in the past year; some of it is duplicative. #12. Some Maximus liaisons appear to have biases for/against certain services, making it difficult to obtain these disfavored services when they are needed. #13. Medicaid provider application packages are complex and difficult to complete, discouraging potential providers (e.g., 74 dentists) from applying. #14. The paperwork and processing time now required for cost plan amendments can result in service interruptions to the individuals. #15. The need to show “medical necessity” for services for individuals who do not have a lot of medical problems can be extremely difficult and seems to conflict with making individual choices. Suggestions for Addressing Service Obstacles and Systems Problems. In addition to identifying service obstacles and systems problems, focus group and survey respondents also suggested ways to address these issues that would improve/expand access to services. These suggestions are listed below, and numbered according to the issue above that each addresses. #1. Staff and supervisors in ADT programs should be well trained and accountable for helping each individual served with making measurable progress toward meeting individual goals. #2. Providers of Res Hab services should be held accountable for helping each individual served to make measurable progress toward meeting the individuals’ goals toward more independent living. #3a. Direct support staff in ADTs and Res Hab settings should be given adequate pay and other retention-oriented incentives, as well as receive adequate pre-service and ongoing in-service training. #3b. Develop and offer on-line and teleconference training for staff in Res Hab and ADT settings. #4. Seek waiver coverage of supplemental transportation for community participation, day activities, volunteer work etc, for group home residents when such activities are part of an individual’s plan. #5. Paratransit providers should be held accountable for a higher quality of service and not reimbursed for service that fails to meet such standards; drivers should receive more intensive training. #6. Dental staff and resources of DSIs should be partnered with dental schools and used to provide pre-service training to dental students and continuing education certification to current practitioners. 75 #7. Seek DVR funding for SE follow-along for transitioning students who are not on the waiver and do not have a support coordinator. #8. DDP should recruit Medicaid home health agencies and offer training in caring for persons with developmental disabilities to companions and PCAs. #9. While seeking full funding and rapid implementation of services to individuals on the waiting list, the DDP should develop a mechanism for updating families every six months about their status on the list, and to determine any changes in client or family circumstances. #10. All DDP staff must be informed immediately that they should encourage all eligible individuals to apply for the Medicaid waiver. #11. The paperwork process for obtaining services and for obtaining prior authorizations should be streamlined and automated to the greatest extent possible. #12. Maximus staff should be trained on the need to be objective when evaluating prior service authorization requests and refrain from displaying any bias for or against certain types of services. #13. Medicaid provider application packages must be streamlined and the application process abbreviated for dental professionals who are in such great demand statewide. A financial incentive for potential dental providers might also be considered. #14. Paperwork and processing time for cost plan amendments must be reduced to a maximum time limit of 15 days, which would prevent any interruption in services to beneficiaries. #15. Consider broadening the term, “medically necessary” when applying it to services for otherwise eligible individuals with developmental disabilities, who are seeking more community independence. B. Individuals with Developmental Disabilities Who Are Not Receiving Services. Focus group and survey respondents were queried regarding their knowledge of individuals with developmental disabilities who are not currently receiving services from DDP. Those who identified unserved individuals were also asked to provide reasons for the lack of services. The following descriptions of individuals and reasons were presented. 76 Respondents from eight different districts acknowledged knowing individuals with disabilities who are not receiving services. Two of the individuals described are otherwise eligible for services but do not qualify for Medicaid. Furthermore, There are currently 70 DDP clients in Monroe County who do not receive any DDP services. (Whether there is an absence of providers for the services in question is not explained.) Several foster children with disabilities in district 14 are not DDP clients because the constant changing of foster care staff has made processing of their applications difficult for DDP staff. Several respondents mentioned a large number of individuals who have been on the waiting list for a long time, but who are not considered to be “in crisis.” Several respondents describe nearly 30 individuals whom they know that were turned away by DDP staff. One respondent mentioned knowing of a number of individuals who do not receive services because their parents and guardians are either new to the area or they are poor and uneducated and do not understand/are intimidated by the system. IV. CONCLUSIONS AND RECOMMEND ATIONS FROM THIS STUDY A. The Overall Service Picture in Florida. While there is a wide array of publicly funded social and health services available to the residents of Florida, the DDP remains the primary provider (through AHCA) of services to adults with severe developmental disabilities. The majority of these services are now provided under the DDP’s HCBS waiver. Over the past several years, a considerable increase has occurred in the amount of services provided and the number of people being served, due to an aggressive pursuit of Medicaid waiver funds. This success has been tempered by the fact that whenever an individual on the waiver waiting list has been served, another person appears to take his/her place. This phenomenon gives weight to the estimate that there are likely about 80,000 people with developmental disabilities in Florida who need or will need services. This number is approximately twice the total of people now being served in either institutional or community based settings. Conflicting Service Trends. Though the DDP does not “market” its services, in a real sense, new service expectations are being created. While DD services evolved over the past 50 years from being institutional based to being community based, living arrangements became smaller. As the current generation of potential consumers moves out of the school system, they are not looking for sheltered work and group living environments, rather they are expecting individualized service settings. Inspired by self- 77 determination principles and the right to choose, they expect to be accommodated by the services they desire. Yet, there remains an established group of older individuals and their families that expects and is comfortable with group homes and day programs. And they, too, expect to be accommodated. Simultaneously, in a state that long lagged behind other states in providing services to adults with disabilities, a pent-up demand for services is being released. As a result, the DDP must manage services to accommodate both sets of expectations, while continuing to see a waiting list for services that never seems to disappear. One telling sign of the power of the new wave of expectations is the “system redesign” which is now underway in the DDP. Many of the stakeholder groups involved in planning the redesign are champions of individualized services and community independence. Over time, the emerging consumer market will likely redefine the services which providers offer. And, as in other states, the roles of day programs and group homes will probably diminish. Group homes may gain a different service emphasis, and will increasingly become the choice for older adults who have lived their entire lives with, and supervised by, their parents. The existence of current and future recipients with different service expectations will undoubtedly result in tensions within the system. A current indicator of such tension is heard in the adamant voices of some advocates who call for moving individuals from the sheltered services of Res Hab and ADT to the independent services of SE and SL. The rationale is, that moving some individuals from more expensive services into less expensive, will clear the way for people on the waiting list to obtain services. Overall, they believe, more people will be served with the same amount of money. Given the fact that the state budget shows no immediate hope for fully funding services for those on the waiting list this year, the demand to move people to less expensive services might sound appealing. But there are two important caveats here. First, many individuals currently receiving group services would need intensive, long-term support services in both SL and SE to be successful in those independent settings. The cost of these additional supports would quickly erode (and perhaps outstrip) any savings that resulted from the initial transfer. When the dust finally settles from these transfers, fewer (rather than more) people may end up being served. From a fiscal perspective, it would be more prudent to consider moving only those individuals whose transfers would result in a cost savings. 78 Second, and more important, individuals receiving group services may do so out of preference and comfort level. Since a hallmark of the waiver is choice and self-direction, no one can be forced to accept more independent services when both types exist, even in light of the Olmstead decision. Therefore, a more thoughtful approach to balancing these two “rights” and managing this tension must be achieved by the DDP. A Change in Service Intensity. Another trend to consider is the escalation of service expenditures, as a result of families growing older. In the state of Arizona, for instance, 65% of the people receiving services live at home with their parents, whose average age is 62. These demographics are very similar to the situation in Florida. With aging caregivers, the number of services hours for inhome support services will tend to increase. This becomes necessary, not due to any change in the health of the care recipients, but because their parents’ ability to provide care diminishes. An increase in costs results, due to more service units being needed. B. Obstacles and Recommendations from the Study. The following obstacles, gaps in services and recommendations are derived from the data gathered in the analysis of services and from the data gleaned from the input of stakeholders. As in Part One, these are presented in chronological order. Services for Children. 1.1 Obstacle: Children who are not eligible for Medicaid may not receive expensive therapies or treatments that are not covered by private insurance. 1.1 Recommendation: Work to enact legislation requiring private insurance coverage of certain expensive therapies and treatments that are needed by children with developmental disabilities. 1.2 Obstacle: There is a lack of service providers of various adjunctive therapies for children in all school district areas. 1.2 Recommendation: Work to enroll more Medicaid providers of various therapies for children, to assure they are available to provide services to school districts in all areas of the state. 1.3 Obstacle: Certain professional documentation on a student’s CERT may unjustly result in the termination of adjunctive therapies. 1.3 Recommendation: Support the efforts of the Advocacy Center in neutralizing the effect of CERT documentation upon the status of adjunctive therapies. 1.4 Obstacle: Funding caps may preclude children with less 79 severe physical disabilities from accessing health care services. 1.4 Recommendation: Provide a sufficient safety net to assure health care access for children who may have less severe physical disabilities or health care needs. Services for Children Transitioning from School 2.1 Obstacle: Transition of health care services for children who are transferring from pediatric health care providers to adult providers of care is poorly planned; access to experienced providers is severely limited. 2.1a Recommendation: Develop a mechanism akin to school transition services that will ensure the continuity of health care for transitioning students to experienced providers. 2.1b Recommendation: Support the use of materials developed by the Adolescent Health Transition Project at the University of Washington, to educate individuals and their families about transitioning health care services. 2.2 Obstacle: Poor, uneducated and some minority families do not participate in the transition planning process with their children. 2.2 Recommendation: Develop outreach training and mentoring for poor, uneducated families, using low reading level and alternate language materials. 2.3 Obstacle: There are inconsistencies in the quality of transition services within and across school districts. 2.3 Recommendation: Create a position of “Transition Facilitator” within each school district or area to assure consistency of transition services and to work with families. Facilitator positions should be filled with non-educator candidates who have prior, real world disability experience and training. 2.3 Obstacle: There is no seamless transfer of assistive technology devices for transitioning students. 2.3 Recommendation: Alternative methods of paying for assistive technology devices should be in place prior to a student’s transition from school. Consider allowing continued use of district owned technology for students continuing to post-secondary education, pending DVR purchase of replacement devices. 2.4 Obstacle: In some districts DDP staffs discourage transitioning students from applying for the Medicaid waiver, since a long waiting list exists. 80 2.4a Recommendation: All DDP district staff must be trained and updated yearly on understanding the purpose of transition services and of the necessity for preparing for their roles in the Transition IEP meetings. 2.4b Recommendation: All DDP staff must be informed immediately that they should encourage all eligible individuals to apply for the Medicaid waiver. 2.5 Obstacle: Lack of availability of providers adequately trained to participate effectively in transition services. 2.5 Recommendation: Require all providers of adult services to be adequately trained to participate in transition services. Services for Adults 3.1 Obstacle: ADT and Res Hab service expenditures comprise more than 50% of the waiver budget. 3.1 Recommendation: Work to increase the number of providers for SE and SL Coaching services; identify consumers for these options when services exist. 3.2 Obstacle: Nearly 11,000 people are currently on the waiting list for the waiver. 3.2 Recommendation: Support full funding to serve all individuals on the wait list. 3.3 Obstacle: The cost of AT is often prohibitive for consumers who are not covered by the waiver or eligible for DVR services. 3.3 Recommendation: Encourage federal subsidies for AT development to lower prices for consumers; expand AT recycling efforts of FAAST. 3.4 Obstacle: There is a shortage of affordable, accessible housing in Florida. 3.4 Recommendation: Support federal and state subsidies for the development of affordable, accessible housing. 3.5 Obstacle: SL coaches and support coordinators are often unfamiliar with the housing resources in their local communities. 3.5 Recommendation: Develop specific multi-media training materials on local housing resources for continuing education of SL coaches and WSCs. 3.6 Obstacle: Statewide, there is a serious lack of dental care providers who are familiar with and available to treat individuals with disabilities. 3.6 Recommendation: Dental staff and resources of DSIs 81 should be partnered with dental schools and used to provide pre-service training to dental students and continuing education certification in disabilities to current dental practitioners. 3.7 Obstacle: There is a lack of understanding, reporting and prosecution of crimes committed against people with disabilities. 3.7 Recommendation: Increase public awareness of these crimes by conducting a statewide educational campaign and providing widespread training of individuals, families, disability professionals and criminal justice professionals. Services for Older Adults 4.1 Obstacle: There are few options for day programs for older adults or younger individuals with severe cognitive impairments. 4.1 Recommendation: To avoid duplication of effort, allow older individuals (and those with severe cognitive impairments) on the DDP waiver to receive cross-waiver, adult day care services (Aged and Disabled Waiver) as a substitute for ADT services. Recipients should not lose their DDP residential services or support coordinators, when this is the best service choice for the individual’s needs. 4.2 Obstacle: Elderly parents are often no longer able to provide care for their adult offspring, and are fearful about the lack of available residential options. 4.2 Recommendation: Using existing models, the DDP should begin developing specialized group homes for older individuals in all districts across the state. 4.3 Obstacle: Elderly parents do not make future-care plans for their offspring. 4.3 Recommendation: All support coordinators should attend “train-the-trainer” sessions in future-care planning as part of their required continuing education. This will equip them to train, guide and counsel all elderly families they serve in using the tools and completing the activities of future-care planning. 4.4 Obstacle: Obesity and lack of exercise are common health problems of older adults with developmental disabilities. 4.4 Recommendation: Adopt healthy lifestyles training as a core part of training programs for all individuals receiving Res Hab services or living in group homes. 82 Taken together, the gaps, obstacles to services and recommendations for improvement listed above, and those identified by stakeholders, comprise a litany of opportunities to achieve better coordination and an expansion of services to individuals with disabilities in Florida. Acknowledging the heterogeneity of individuals with disabilities, no attempt was made to rank these obstacles and recommendations in order of importance. In fact, many of the issues identified are consistent with The Council’s 2003 Legislative Priorities. The new issues that surfaced in this report may provide the impetus for future action. V. E M E R G I N G N AT I O N A L T R E N D S A N D T H E I R I M PA C T I N F L O R I D A A. Employment. There is ample data to prove that people with disabilities are the most unemployed and underemployed individuals in the country. Yet the vast majority of these people are willing and able to work. Rather than depending on federal benefits and services to survive, thousands of people with disabilities would rather have a good, steady job and be productive, tax paying citizens. The Workforce Investment Act is the federal government’s approach to job training for the general population. The concept is that, through One-Stop delivery centers, job seekers can access job training and other related programs. People with disabilities are expected to be one of the constituencies that use these centers. However, job seekers with disabilities are finding it difficult, if not impossible, to make their way through the One-Stop mazes. Here in Florida, the DVR is working together with DLES in pilot programs in several counties, to assure that One-Stop users with disabilities looking to connect with DVR are able to do so successfully. B. Housing. To be part of the community and live as independently as possible is one of the most important dreams shared by many individuals with disabilities, their families and advocates. Across the country, at least 640,000 individuals live with their aging parents who are over the age of 65. People with cerebral palsy and other mobility impairments find it nearly impossible to locate housing with even basic accessibility features. This difficulty is magnified in rural counties where rental housing is scarce and new homes are rarely built. The U.S. Department of Housing and Urban Development (HUD) is responsible for providing housing and housing assistance available to those in need. HUD reports that the housing needs of most lowincome people across the country have improved. At the same time, 83 however, the most urgent housing needs of people with disabilities have only deteriorated. Section 8 Rental Assistance, with its Housing Choice Voucher program, currently mandates that all 50,000 vouchers designated for people with disabilities since 1997 continue to be set-aside for people with disabilities. However, the Bush Administration is proposing to block grant the Section 8 voucher program and transfer it to the states to administer, rather than the public housing authorities. Should this occur, people with disabilities will lose out, since states will be forced to choose between reducing the monthly subsidies on the vouchers, or reduce the number of households who receive assistance. A National Affordable Trust Fund Act has been introduced into Congress. By using a portion of FHA profits to establish a trust fund, this bill would triple affordable housing construction across the country. States and non-profits could draw from this trust to build affordable housing. This should dramatically increase the number of wheelchair-accessible housing units nationwide. In Florida, continued funds will be available to purchase new homes and rehabilitate existing affordable, accessible homes for people with disabilities, since the Sadowski Trust Fund, which supports the SHIP program, escaped Legislative efforts to transfer its funding into general revenue this year. C. Assistive Technology. The use of assistive technology devices has greatly increased since the early nineties, due to the aging of the population as well as to advances in technology, public policy initiatives and changes in the delivery and financing of health care. Two decades ago there were 60 U.S. companies manufacturing assistive technology products. Today, there are hundreds of companies nationwide and about a thousand worldwide. Assistive technology is a part of the lives of about 1/3 of the 54 million people with disabilities in this country—more than 18 million people. According to the National Center for Health Statistics, across the country, an estimated 7.4 million persons with mobility impairments use assistive technology devices. Of these, 1.5 million use wheelchairs. Another 4.6 million use back braces and artificial limbs to compensate for orthopedic impairments. 4.5 million people use hearing aids, amplified phones, closed captioned television and other assistive devices for hearing impairments. An additional 500,000 individuals use these devices for vision impairments. Assistive technology plays an important role in increasing the presence of people with disabilities in their communities. Yet, 36 million people with disabilities do not use assistive devices. Many of them are unemployed, underemployed and uneducated for 84 the workplace. To remedy this loss of productivity, the National Council on Disability offers the following guidelines: a. “Manufacturers must expand their marketing programs so more people with disabilities and their families learn about these products. An improved marketing program will sell more products and, consequently, reduce their cost. The high cost of some products has often discouraged potential buyers. b. Federal and state governments must help subsidize the high development costs of assistive technology products. c. Creative ways must be found to help consumers pay for this equipment, so that no one is left behind. d. Public and private sector employers must hire people with disabilities. In doing so, they must consider the purchase of assistive technology as a capital investment and not an extra expense. e. We must ensure that all students with disabilities who require assistive technology devices have them. We can no longer afford to have hundreds of students with disabilities drop out of schools annually, because schools lack qualified teachers and the AT equipment to educate them. It is essential to continue to develop and distribute these tools, which can enhance the independence and abilities of people with disabilities, not merely because it is right…but because it benefits the country.” In Florida, the responsibility for providing assistive services and technology to people with disabilities is distributed across a range of agencies: DOE, school districts, DVR, DOH (CMS), DDP, AHCA, FAAST and the Advocacy Center for Persons with Disabilities. Each of these entities plays a different role in the delivery system, but there is no entity coordinating these roles. Florida must support legislation to establish a coordinated system for delivering the appropriate assistive technology devices to the people with disabilities who need them, regardless of funding source, across their lifetimes. Such a system would also recycle devices that have been outgrown. Another element in the system might be an AT voucher, which informed consumers could use to purchase the services and devices they require. D. Consumer Directed Care. This is a national trend that is already affecting Florida. Many individuals with disabilities and their families prefer to directly manage the services and supports they receive. They want to make the decisions about who will come to the home to provide services and when they will come. This is one way of insuring that the services and supports they receive are tailored to 85 their needs and preferences. Over the past several years, around the country and in Florida, several consumer and family-directed care demonstration programs were conducted with funding from Medicaid and the Robert Wood Johnson Foundation. Unanimously, the participants in these programs proclaimed greater satisfaction with their services and with their lives. The success of such programs has led to a number of states—including Florida—applying for and receiving new Medicaid waivers called Independence Plus, which feature consumers and families directing the delivery of care. This new waiver is expected to begin in Florida sometime later in 2003. The clamor for more control and flexibility in managing care has also had an impact of the service delivery format that DDP expects to implement, under the System Redesign that is currently underway. A chief feature of the redesign is that, once individual service budgets are approved, a flexible services menu will allow individuals and families to move easily between service categories as the needs of individuals change. Purchases of services based on those changes will require no further DDP approval, as long as the overall budget is the same. Also, with service providers submitting their own billing under the new system, service recipients will have an opportunity to review monthly bills for the services they receive. E. Medicaid. The national trend that is likely to have the most impact on Florida residents with disabilities is the Bush Administration’s proposal for converting Medicaid into a program with capped allotments, essentially making it a block grant. While the proposal offers states additional money for Medicaid for the next seven years, it also requires that state accept a capped allotment that requires them to repay advanced federal funds in later years. According to the current proposal, states opting not to choose the block grant will continue to administer Medicaid programs under existing rules and without additional funding. Though the receipt of additional funds sounds like a boon to cash strapped states, the acceptance of capped allotments would preclude states from accepting more enrollees and destroy Medicaid’s role as an entitlement program. Over 1.5 million individuals with disabilities are now Medicaid “optional” beneficiaries, including individuals eligible for home and community based waivers. The services used by these individuals vary. Under this proposal, states would have the unfettered discretion to define both eligibility and benefits for people with disabilities, so that coverage would no longer be guaranteed. In an environment of decreasing state revenues and escalating Medicaid costs, decreases in services to people with disabilities would seem inevitable. Important federal protections regarding service access and service quality would be at risk. Cutbacks would exacerbate the crisis in the availability of direct care workers, further affecting service quality. 86 With the State of Florida looking at a waiting list of nearly 11,000 new people for the DDP HCBS Medicaid waiver, the enactment of this proposal would be a devastating blow, whether or not this state chose to participate in the block grant option. Either way, the result would be unacceptable: inevitably, there will be fewer services for less people with disabilities, now or in the future. ………………………………… 87 REFERENCES USED IN THIS REPORT AAMR. (2003). Fact Sheet: Aging – Older adults and their aging caregivers. Retrieved 3/31/03 from http://www.aamr.org/Policies/faq_aging.shtml A guide for professionals to vocational rehabilitation and school-to-work transition services. (Pamphlet). Florida Department of Labor and Employment Security. Division of Vocational Rehabilitation A profile of older Americans. (2001). U.S. Department of Health and Human Services: Administration on Aging. Affordable housing opportunities for people with disabilities: Demonstration projects and best practices. (2002). Florida Housing Coalition for the Florida Developmental Disabilities Council, Inc. Agency for Health Care Administration. (2002). Florida Medicaid Summary of Services. State of Florida: Author. Ashbaugh, J. (2001). Better managing the delivery of services and support to people with developmental disabilities using information technology. Mental Retardation, 39 (4), 322326. Children’s Medical Services: CSM Network. (2003). When youth with special health care needs transition to adulthood. Retrieved 4/3/03 from http://www.cms-kids.com/CMSNTransition.htm Children’s Medical Services: CMS Network. (2003). Assistive Technology. Retrieved 4/3/03 from http://www.cms-kids.com/CMSNTrans9.htm Children’s Medical Services: Infants & Toddlers Early Intervention Program. (2002). Program Data and Reports. Retrieved 4/3/03 from http://www.cms-kids.com/InfantPrgData.htm Consumer directed care - The Florida cash and counseling demonstration. (2003). Medstat. Department of Elder Affairs Major Programs – requirements and services. (2002). State of Florida: Department of Elder Affairs. Developmental Services waiver services, Florida Medicaid: Coverage and limitations handbook. (2002). Agency for Health Care Administration. Dixon, K.A., Kruse, D., & Van Horn, C.E. (2003). Americans’ attitudes about work, employers and government work trends: Restricted access: a survey of employers about people with disabilities and lowering barriers to work. The State University of New Jersey, John J. Heldrich Center for Workforce Development. 88 Executive Summary: 2000 N.O.D./ Harris survey of community participation. (2002). National Organization on Disability. Retrieved 3/4/03 from http://www.nod.org/content.cfm?id=1078 FAAST. (2000). K-12 Students Rights to Assistive Technology in Florida. Florida Alliance for Assistive Services and Technology. Retrieved 5/3/03, from http://faast.org/atresources/students.htm. Final SCHIP Annual Report Framework - Section VI: Program challenges and accomplishments. State of Florida. Florida Department of Education. (2001). Education Information and Accountability Services. Statistical Brief: Bureau of Education Information & Accountability Services, Series 2002-06B. Florida Department of Education. (2000). Developing quality individual educational plans: A guide for instructional personnel and families. Florida Department of Education: Division of Public Schools and Community Education. (2000). Diploma decisions for students with disabilities: What parents need to know. Florida Department of Education. (2000). Accommodations and modifications for students with disabilities: Vocational education and adult general education. Florida Department of Education: Vocational Rehabilitation Services. (2001). Annual Report of Fiscal Year 2000-2001. Florida Developmental Disabilities Council, Inc. and Florida Dept. of Health. (2002). The health of Florida’s children and youth: Atlas of key status indicators, goals, and objectives for strategic planning. Florida Developmental Disability Program. Where DDP stands (and the challenges ahead). PowerPoint presentation. (2002). State of Florida: Department of Children and Families. Florida Statewide Quality Assurance Program Annual Report 2001-2002. (2002). Delmarva Foundation, Joint Commission on Accreditation of Healthcare Organizations, Medstat, The Council on Quality and Leadership, & Garcia and Ortiz. Fox, H., Limb, S., & McManus, M. (2003). SCHIP Innovations for children with special needs in managed care. Center for Health Care Strategies, Inc. Resource Paper. Frequently asked questions to program evaluation unit. Florida Department of Elder Affairs. Retrieved on 10/9/02 from http://www.myflorida.com/doea/2830dep/2820faq.html HHS approves Florida independence plus waiver to allow more people with disabilities to control their care. (2003). United States Department of Health & Human Services. Health and Human Services: Developmental Disabilities CHAMPS General Information. Delmarva Foundation Responsible for Statewide Quality Assurance Program for DS Waiver Services. Retrieved 10/8/02 from http://myflorida.com/cf_web/myflorida2/healthhuman/ddp/qa&i/champs/gen_info.html 89 Hoenig, H., Taylor, D.H., Sloan, F.A. (2003). Does assistive technology subsitute for personal assistance among the disabled elderly? American Journal of Public Health, 93 (2), 330337. Jacksonville Community Council Inc. (1997). Transportation for the disadvantaged. JCCI, 1-28. Larson, S.A., Lakin K.C., Anderson L., Kwak, N., Hac Lee, J., & Anderson, D. (2001). Prevalence of mental retardation and developmental disabilities: Estimates from the 1994-1995 National Health Interview Survey Disability Supplements. American Journal on Mental Retardation, 106 (3), 231-252. McCall, D. (2000). Florida Health Care News. State Center for Health Statistics. Retrieved from http://www.floridahealthstat.com/publications/ruralhealth.pdf Medicine & Health Review. (2003). Key to outcomes is treatment quality, not quantity. Health Care Information Center, 57 (1), 7. Medicaid recipients with disabilities benefit from directing their own personal care services, study finds. (2003). United States Department of Health & Human Services. Retrieved 4/21/03 from http:///www.hhs.gov/news/press/2003pres/20030415.html Medicaid Summary of Services. (2002). Ambulatory surgical centers. State of Florida: AHCA. Membership in programs for exceptional students (2003). State of Florida: Department of Education, Bureau of Education Information and Accountability Services, Series 2003-11B. National Center for Health Statistics. Disabilities/Impairments. Retrieved 3/17/03 from http://www.cdc.gov/nchs/fastats/disable.htm National Center for Health Statistics. (1997). New report on disability available from NCHS. Retrieved 3/17/03 from http://www.cdc.gov/nchs/releases/97facts/disable.htm National Center on Secondary Education and Transition. (2001). Current challenges facing the future of secondary education and transition services for youth with disabilities in the United States (Draft). University of Washington: Author. Office of Program Policy Analysis and Government Accountability, Office of the Florida Legislature. (2002). Legislative options to control rising developmental disabilities costs. OPPAGA Program Review, Report No. 02-09. Office of Program Policy Analysis and Government Accountability: Office of the Florida Legislature. (2000). Justification Review. Developmental Disability Program: Florida Department of Children and Families. OPPAGA Program Review Report No. 00-17. Office of Program Policy Analysis and Government Accountability: Office of the Florida Legislature. (2000). Performance Review. Developmental Disability Program: Florida Department of Children and Families. OPPAGA Program Review Report No. 99-31. 90 Osborn, S. (2000). Trends in assistive services & technology: In the nation and in the state of Florida. Florida Alliance for Assistive Services and Technology Organization. Retrieved 5/3/03 from http://faast.org/atresources/trends.htm Rowland, C. (2002). White paper: The role of technology in preparing youth with disabilities for postsecondary education and employment. Utah State University, Center for Persons with Disabilities, Web Accessibility In Mind (WebAIM). Rural and Urban Health. (2003). Challenges for the 21st century: Georgetown University, Chronic and disabling conditions, 7. Schneider, G. (2001). An opening and a closing bring tears of joy in SW Florida. Housing News Network, 16 (2), 9. Smith, G.A., Prouty, R., and Lakin K.C. (2001). Medicaid long-term services for people with developmental disabilities – That was then, this is now. Mental Retardation, 39 (6), 488-491. State of Florida, Developmental Disabilities Program Office. Redesign focuses on service delivery. (2002). Developmental Disabilities Program Office E-Bulletin, 1 (14). State of Florida, Developmental Disabilities Program Office. Redesign focuses on service delivery. (2002). Employment: An important part of adult life. Developmental Disabilities Program Office E-Bulletin, 1 (18). State of Florida, Developmental Disabilities Program Office. Redesign focuses on service delivery. (2002). Provider Cost Survey another piece of system redesign. Developmental Disabilities Program Office E-Bulletin, 1 (18). State of Florida, Developmental Disabilities Program Office. Update on developmental system redesign activities. (2002). Developmental Disabilities Program Office E-Bulletin, 1 (10). State of Florida, Developmental Disabilities Program Office. (2002). Developmental disabilities program legislative budget request for fiscal year ‘03-’04 released. Developmental Disabilities Program Office E-Bulletin, 1 (13). State of Florida, Developmental Disabilities Program Office. (2003). What’s Next in the System Redesign? Developmental Disabilities Program Office E-Bulletin, 1 (22). State of Florida, Developmental Disabilities Program Office. (2003). Prior Services Authorization. Developmental Disabilities Program Office E-Bulletin, 2 (1). State of Florida, Developmental Disabilities Program Office. (2002). Facts about developmental disabilities and the developmental disabilities program. Developmental Disabilities Program Office E-Bulletin, 1 (2). State of Florida, Developmental Disabilities Program Office. (2002). Stakeholders Provide input into developmental. Developmental Disabilities Program Office E-Bulletin, 1 (4). 91 Texas Council for Developmental Disabilities. (2001). 2000 Biennial report: Imagine the possibilities, Imagine the hope. Texas: Texas Office for Prevention of Developmental Disabilities. The ARC, AAMR, UCD, UCP. (2003). Policy paper on the Assistive Technology Act. The Commission for the Transportation Disadvantaged. (2002). 2001 Annual Performance Report. State of Florida. The Family C.A.F.E. (2002). Florida Developmental Disabilities Status Report. Tobias, C., & Haberlin, K. (2001). A study of the health care system for adults with developmental disabilities in Florida. United States Dept. of Health and Human Services, Administration for Developmental Disabilities, and the Florida Developmental Disabilities Council, Inc. Transportation Access: Facts & Statistics - Access to transportation. (2001). National Organization on Disability. Retrieved 3/4/03 from http://www.nid.org/content.cfm?id=798 United States Census Bureau: State and County QuickFacts. Retrieved 12/15/02 from http:quickfacts.census.gov/qfd/states/12000.html University of Colorado, Coleman Institute. (2000). The State of the States in Developmental Disabilities: Florida. Retrieved 7/31/02, from http://www.cusys.edu/ColemanInstitue/stateofthestates/statehomepage.htm University of Miami, Department of Pediatrics: Mailman Center for Child Development. Early intervention and assistive technology working together. Retrieved 1/24/03 from http://pediatrics.med.miami.edu/mailman/assist_tech.htm University of Minnesota, The College of Education & Human Development. (2000). Prevalence of metal retardation and/or developmental disabilities: Analysis of the 1994/1995 NHIS-D. MR/DD Data Brief, 2 (1). Ward, T. (1999). Student performance standards. Florida Alliance for Assistive Services and Technology. Retrieved 5/3/03 from http:www.faast.org/atresources/papers.htm Ward, T. (2002) Florida housing resource guide. Florida Alliance for Assistive Service and Technology. Williams, J. (2003). Assistive Technology – What is it and how it improves our lives. National Organization on Disability. Retrieved 3/17/03 from http://www.nod.org/content.cgoom?id=1354 92